ARTICLE Vol. 2, No. 2, November 2009
Received February 20, 2009 / Accepted July 17, 2009
Correspondence: June-Key Chung, MD, PhD, Department of Nuclear Medicine, Seoul National University College of
Medicine, 28, Yeongeon-dong, Jongno-gu, Seoul 110-744, Korea
Tel: 82-2-2072-3376, Fax: 82-2-766-9083, E-mail: jkchung@plaza.snu.ac.kr
Usefulness of SUV Ratio for Differentiating Benign from Malignant Focal Thyroid Lesions Incidentally Detected by F-18 FDG PET/ CT:
Comparison with SUV Analysis
Bom Sahn Kim, MD 1 , Won Jun Kang, MD 2 , So Won Oh, MD 3 , Dong Soo Lee,
MD 3,5,6 , June-Key Chung, MD 3,4,5 and Myung Chul Lee, MD 3
Department of Nuclear Medicine, Ewha Womans University College of Medicine
1; and Division of Nuclear Medicine, Department of Radiology, Yonsei University College of Medicine
2; and Department of Nuclear Medicine
3; Cancer Research Institute
4; Research Institute of Radiation Medicine
5, Department of Molecular Medicine and Biopharmaceutical Science
6, Seoul National University College of Medicine, Seoul, Korea
Background and Objectives: We investigated the usefulnesses of SUV and SUV ratios in terms of discriminating focal thyroid lesions incidentally detected by F-18 FDG PET/CT (FDG PET) in patients with various cancers.
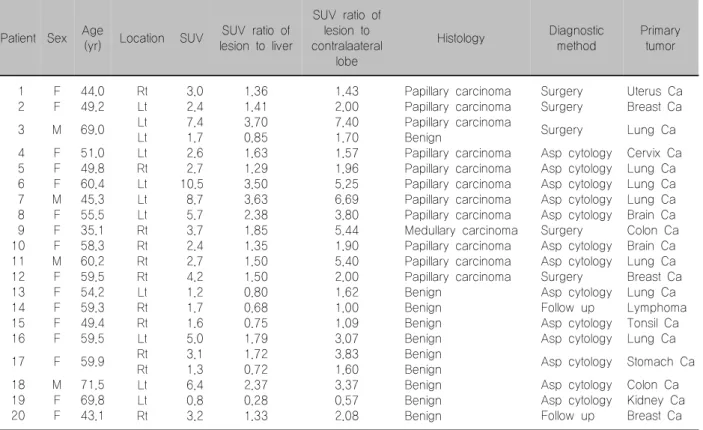
Materials and Methods: Among 2,635 patients, 20 patients with 22 thyroid incidentalomas (benign vs.
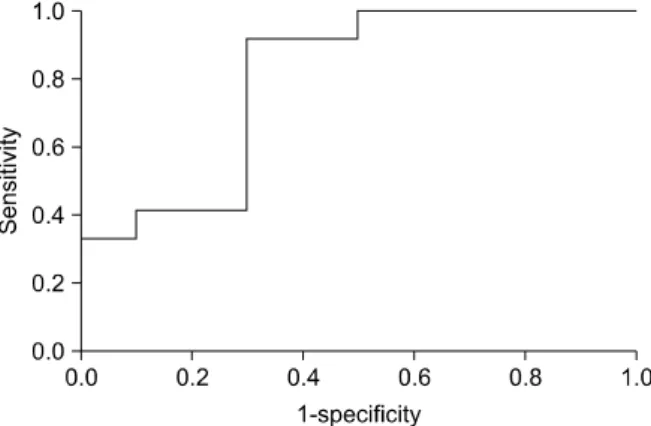
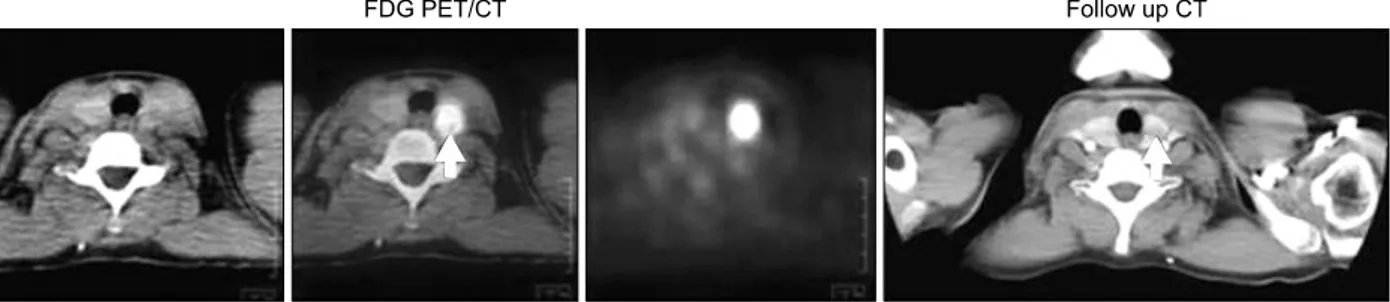
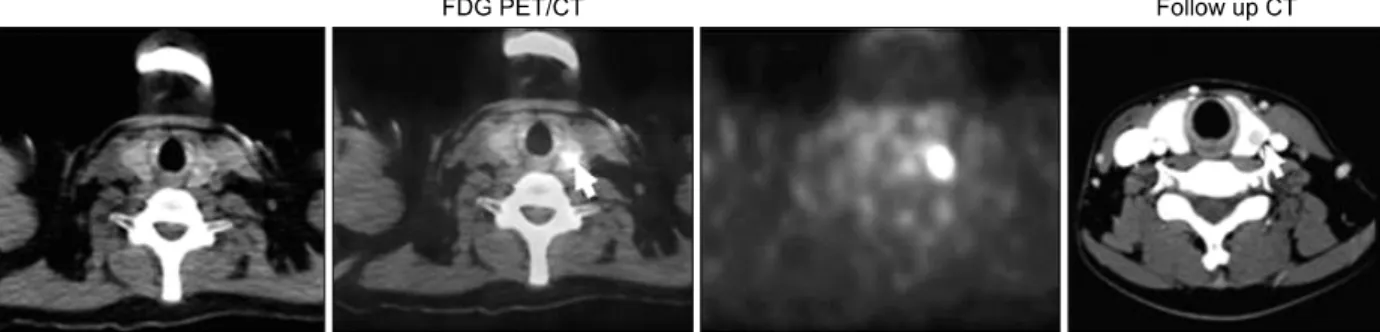
malignant=10 vs. 12) on FDG PET were assessed. Maximal SUV was measured by drawing a ROI on thyroid lesions, on contralateral thyroid lobes, and on the liver. SUV ratio was calculated as the thyroid lesions versus the contralateral lobes and liver. Results: A marginally significant difference in maximal SUV was found between malignant and benign nodules (4.67±2.78 vs. 2.59±1.84, p=0.05). However, more significant differences were found using SUV ratio to normal organs than that of SUV. Malignant nodules had a higher SUV ratio versus liver than benign nodules (2.09±0.96 vs. 1.13±0.65, p=0.012). The SUV ratio of lesions versus contralateral lobes were found to significantly predict the presence of malignancy (3.74±2.19 vs. 1.89±1.17, p=0.027). By ROC curve analysis, the best SUV value cut-off for the prediction of malignancy was 2.42 with a sensitivity of 91.7% and a specificity of 60.0% (AUC=0.758). Similarly, the best SUV ratio cut-off versus the liver was 1.34 with a sensitivity of 91.7% and a specificity of 70.0% (AUC=0.808). But, there was no significant difference between areas of the ROC curves (p=0.736). Conclusion: The SUV ratio had a tendency to discriminate benign from malignant thyroid incidentalomas better than the SUV method. Further investigations with larger number of patients are needed.
Key Words: FDG PET/CT, Thyroid incidentaloma, SUV, SUV ratio
Introduction
Thyroid incidentaloma is defined as a coinci- dentally detected thyroid lesion during image studies, such as, ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI) con- ducted for other purposes.
1) According to one autopsy study, the incidence of thyroid nodules was over than 50% in patients without a history of a thyroid ab-
normality.
2) Therefore, the detection of thyroid inci- dentaloma during radiology studies is not uncom- mon. In previous reports on US, the detection rate of thyroid incidentaloma was 19∼46%. However, most conventional imaging modalities are not efficient at discriminating malignancy.
3-5)
Recently, F-18 fluorodeoxyglucose positron emi-
ssion tomography (FDG PET) has been widely used
for the detection and staging of various cancers,
6) and
frequently detects thyroid incidentalomas. Some in-