Pulmonary Cryptococcosis That Mimicked Rheumatoid Nodule in Rheumatoid Arthritis Lesion
Dong Won Jang, M.D.
1, Ina Jeong, M.D.
1, Seon Jae Kim, M.D.
1, Seok Won Kim, M.D.
1, Soo Yeon Park, M.D.
1, Yong Hwan Kwon, M.D.
1, Yeon Oh Jeong, M.D.
1. Ji Yeon Lee, M.D.
1, Bo Sung Kim, M.D.
2, Woo-Shik Kim, M.D.
3and Joon-Sung Joh, M.D.
1Departments of
1Internal Medicine,
2Pathology, and
3Thoracic and Cardiovascular Surgery, National Medical Center, Seoul, Korea
Recently, the incidence of pulmonary cryptococcosis is gradually increasing in rheumatoid arthritis (RA) patients.
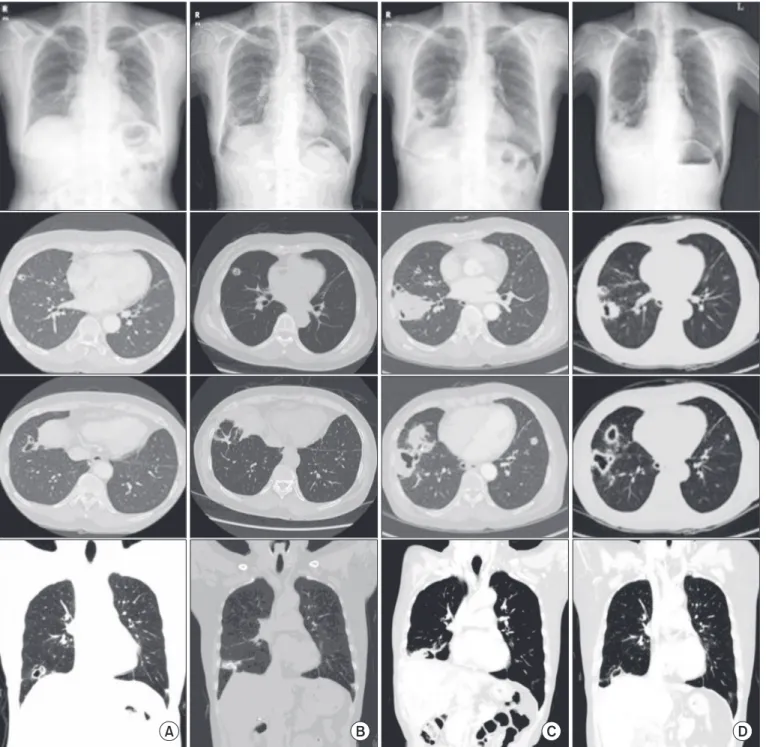
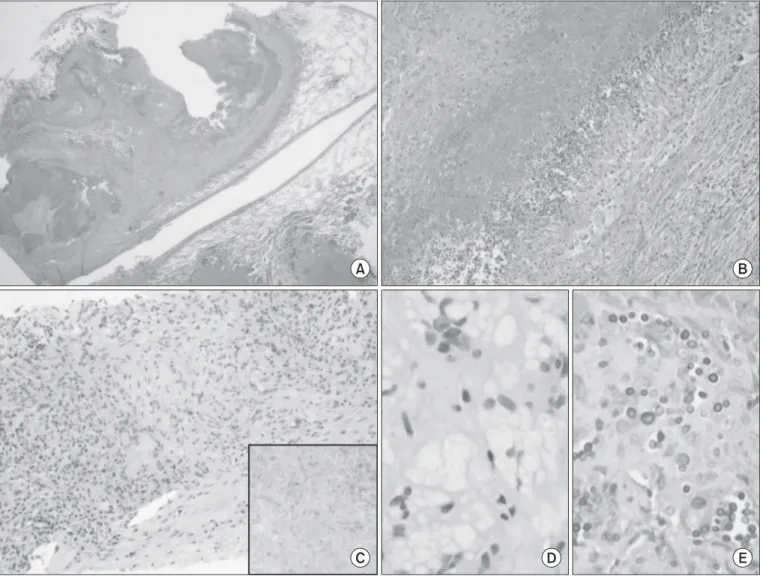
Pulmonary rheumatoid nodules (PRN) are rare manifestations of RA. Eighteen months ago, a 65-year old woman was admitted to hospital due to multiple nodules (2.5×2.1×2 cm) with cavitations in the right lower lobe. She was diagnosed with RA three year ago. She had been taking methotrexate, leflunomide, and triamcinolone. A video-assisted thoracoscopic surgery biopsy was performed and PRN was diagnosed. However, a newly growing huge opacity with cavitation was detected in the same site. Pulmonary cryptococcal infection was diagnosed through a transthoracic computed tomograpy guided needle biopsy. Cryptococcus antigen was detected in serum but not in cerebrospinal fluid.
The patient was treated with oral fluconazole which resulted clinical improvement and regression of the nodule on a series of radiography. Herein, we report the case of pulmonary cryptococcosis occurring in the same location as that of the PRN.
Keywords: Cryptococcus; Cryptococcosis; Rheumatoid Nodule; Arthritis, Rheumatoid
cryptococcosis may affect immunocompetent hosts but is more common in immunocompromised hosts, especially, in patients with human immunodeficiency virus infection, diabetes, malignancy, and organ transplantation. It can also develop as a complication of RA therapy that includes tumour necrosis factor alpha inhibitor or disease-modifying anti-rheu- matic drug use
3. However, clinical and radiographic features are difficult to distinguish between these two disease condi- tions. Pulmonary rheumatoid nodules usually do not need treatment, but disseminated cryptococcosis needs urgent antifungal therapy. Cryptococcosis is more often reported in RA patients, but pulmonary cryptococcosis that mimics a rheumatoid nodule in the same lesion has not been reported before. We report a case of pulmonary cryptococcosis that presented as a cavitary lung mass in the same site as that of the previous rheumatoid nodule.
Copyright © 2014
The Korean Academy of Tuberculosis and Respiratory Diseases.
All rights reserved.
Introduction
The prevalence rate of pulmonary rheumatoid nodules ranges from <1% on chest radiography (CXR) to 32% in lung biopsies of rheumatic arthritis (RA) patients
1,2. Pulmonary
Address for correspondence: Ina Jeong, M.D.
Department of Internal Medicine, National Medical Center, 245 Eulji-ro, Jung-gu, Seoul 100-799, Korea
Phone: 82-2-2260-7323, Fax: 82-2-2260-7281 E-mail: inajeong@gmail.com
Received: Jul. 14, 2014 Revised: Aug. 4, 2014 Accepted: Aug. 28, 2014
cc