pISSN 2765-7833 eISSN 2765-7841
Journal of implantology and applied sciences 2021; 25(2): 84-94
https://doi.org/10.32542/implantology.2021009
Received: March 10, 2021 Accepted: March 30, 2021 ORCID
Youngdeok Chee
전체 글
Received: March 10, 2021 Accepted: March 30, 2021 ORCID
Youngdeok Chee
수치

관련 문서
This study was performed to confirm the effect of the stress distribution on short implant supporting bone according to horizontal bone loss using a three-dimensional
3 Mean percentages of bone implant contact ratio in the control group and experimental groups at 6 and 12 weeks after placement of the
These results suggest that, the ZrN coated Ti-Nb alloy is a good corrosion resistance for dental implant compared with non-coated Ti-Nb alloy... The
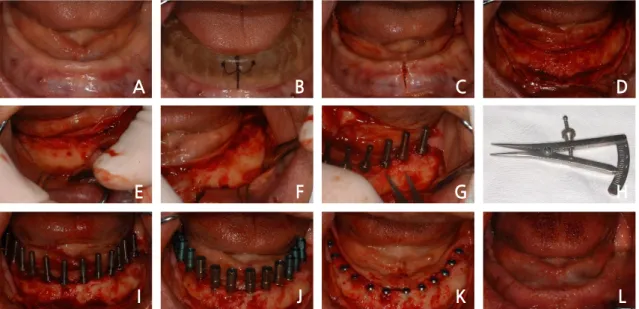
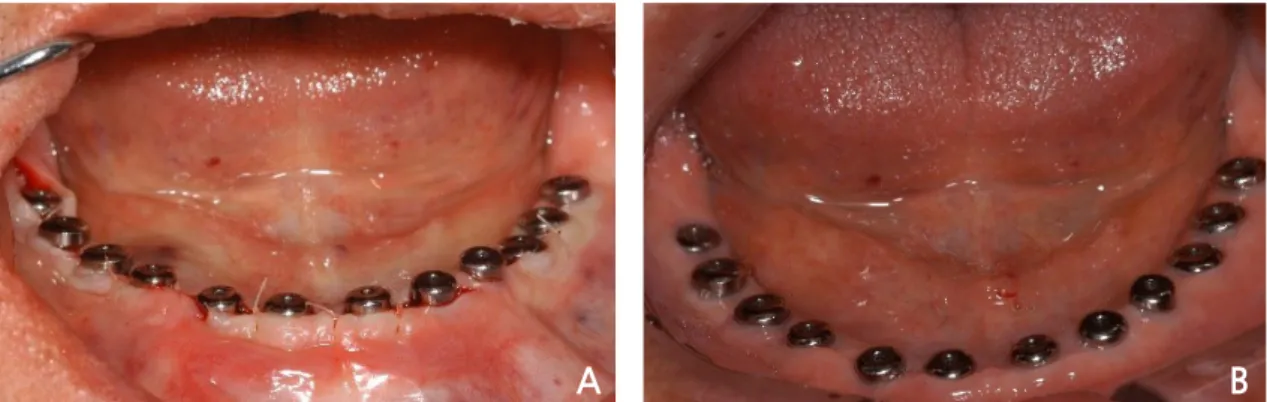
Methods to overcome insufficient bone due to poor bone quality, the pneumatization of a maxillary sinus and other anatomical limitations of implant placement
Salama H, Rose LF, Salama M, Betts NJ : Immediate loading of bilaterally splinted titanium root-form implants in fixed prosthodontics.. A technique reexamined:
A clinical study of the efficacy of gold-tite square abutment screws in cement-retained implant restorations.. An abutment screw loosening study of a Diamond
Histopathologic findings of control group at 4 weeks show little bone- implant contact (BIC) around the implant (asterisks) and new-bone formation in the defect
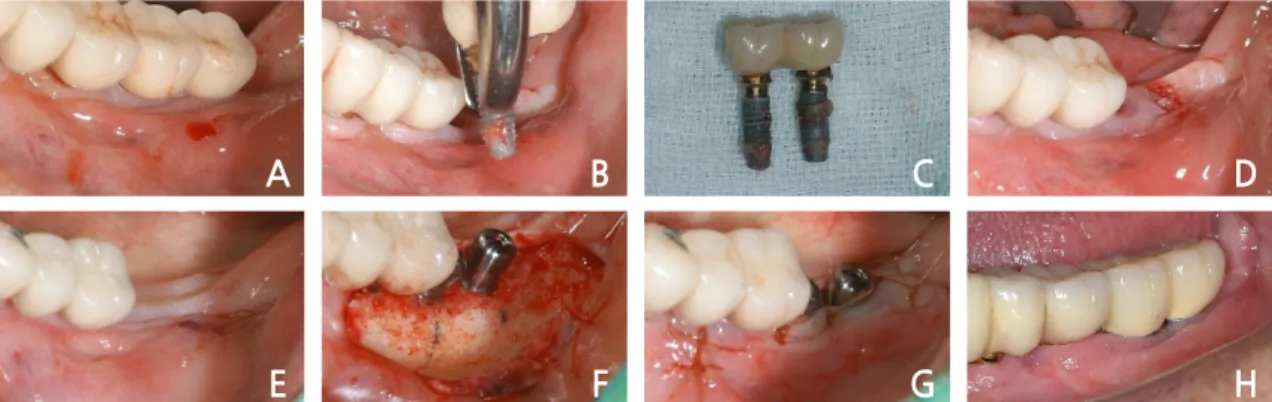
Measurement of proximal contact tightness between the left first molar and second molar(dental implant) in the mandible... Clinical dental anatomy, histology,