접수:2006년 3월 29일, 수정:2006년 5월 20일 승인:2006년 6월 3일
교신저자:김인순, 서울시 성동구 행당동 17번지
133-792, 한양대학교병원 내과 Tel: 02-2290-8333, Fax: 02-2298-9183 E-mail: kimis@hanyang.ac.kr
119
Tumor Lysis Syndrome in Lymphoblastic Crisis of CML
Duk-Joo Lee, M.D., Chi-Un Choi, M.D., Chung-Sik Lee, M.D., Hak-Hyun Lee, M.D., Jin-Kyu Park, M.D., Jung-Hye Choi, M.D., Young-Yeul Lee, M.D.
and In-Soon Kim, M.D.
Department of Internal Medicine, College of Medicine, Hanyang University, Seoul, Korea
Tumor lysis syndrome (TLS) defines the metabolic derangements that occur with tumor breakdown following the initiation of cytotoxic therapy. TLS results from the rapid destruction of malignant cells and the abrupt release of intracellular materials and their metabolites into the extracellular space. The syndrome causes hyperuricemia, hyperkalemia, hyperphosphatemia, secondary hypocalcemia and uremia.
It can result in acute renal failure and be fatal. Early recognition of patient at risk and preventive measures are important. There is a high incidence of TLS in tumors with high proliferative rates and large burden such as acute lymphoblastic leukemia and Burkitt's lymphoma. It less commonly occurs in solid tumors such as testicular cancer, breast cancer and small cell lung cancer. There are only a few reports on TLS complicated in CML in blast crisis. So we report a 45-yr-old woman presenting with TLS associated with CML in lymphoblastic crisis after the initiation of cytotoxic chemotherapy. (Korean J Hematol 2006;41:119-123.)
Key Words: Tumor lysis syndrome, Chronic myelogeous leukemia, Blast crisis
Correspondence to:In-Soon Kim, M.D.
Department of Internal Medicine, Hanyang University Hospital 17, Haengdang-dong, Seongdong-gu, Seoul 133-792, Korea Tel: +82-2-2290-8333, Fax: +82-2-2298-9183
E-mail: kimis@hanyang.ac.kr INTRODUCTION
Tumor lysis syndrome is an oncologic emerg- ency that is characterized by electrolyte abnor- malities, such as hyperkalemia and hypocalcemia, and acute renal failure. The syndrome results from the rapid destruction of malignant cells and the abrupt release of intracellular ions, nucleic acids, proteins and their metabolites into the ex- tracellular space. And it typically occurs in pa- tients with lymphoproliferative malignancies, most often after the initiation of treatment.1) And tumor lysis syndrome rarely occurs in patients with solid tumor, that is, advanced gastric cancer,
advanced hepatocellular carcinoma, metastatic meduloblastoma and prostatic cancer.2-5) In addi- tion, it is reported that the syndrome rarely occurs in patient with chronic myelogenous leukemia, especially in blast crisis.6)
So we report a case of 45-yr-old woman with chronic myelogenous leukemia in blast crisis (ly- mphocytic) who presented a tumor lysis syndro- me after the initiation of cytotoxic chemother- apy.
CASE REPORT
A 45-yr-old woman complained of purplish bruises at both upper extremities and left thigh
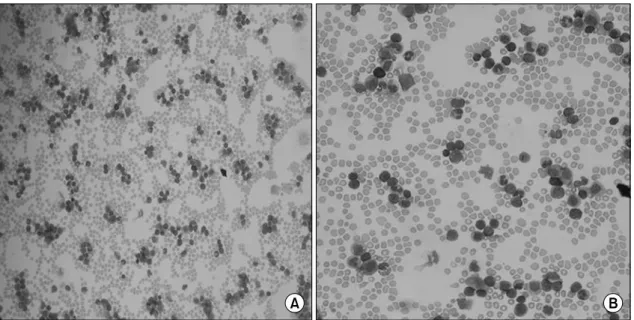
Fig. 1. Peripheral blood smear. Marked leukocytosis composed of immature blasts (44%), band form (5%), promyelocyte (3%), myelocyte (10%), metamyelocyte (7%), segmented neutrophils (13%), eosinophils (3%), monocyte (2%) and lymphocytes (9%) is observed. Moderate decrease of platelet component is also observed. (A) ×40, (B) ×200.
family history of similar symptoms. She visited a local clinic where she was found to be with mar- ked leukocytosis and thrombocytopenia. And she was transferred for further evaluation on the abnormal findings.
Vital signs were blood pressure 120/70mmHg, pulse rate 68/min, respiratory rate 20/min and body temperature 36.9oC. She appeared acutely ill and alert. On physical examination, purplish bruises on both upper extremities and left thigh were observed. And splenomegaly was observed with 3 finger breadths below the costal margin at the left midaxillary region. There is no other peripheral lymphadenopathy. Laboratory findi- ngs on admission were as below: hemoglobin 12.6 g/dL, hematocrit 37.3%, leukocyte count 340,000/
μL with segment neutrophils 15%, band form 6%, lymphocytes 3% and blasts 63%, platelet co- unt 33,000/μL, uric acid 22mg/dL (reference range; 2.2~8mg/dL), blood urea (BUN) 15mg/
dL (reference range; 7~20mg/dL), creatinine 2.2 mg/dL (reference range; 0.6~1.8mg/dL), calcium 10.2mg/dL (reference range; 7.0~10.7mg/dL), phosphorus 4.6mg/dL (reference range; 2.5~4.5
(reference range; 60~200IU/L), sodium 138mEq/
L (reference range; 135~145mEq/L), potassium 3.6mEq/L (reference range; 3.5~5.5mEq/L) and chloride 101mEq/L (reference range; 96~110 mEq/L). Abdominal sonogram revealed a spleno- megaly sized 12cm and no signs of urinary obs- truction. On the peripheral blood smear, marked leukocytosis composed of immature blasts (44%), band form (5%), metamyelocyte (7%), segmented neutrophils (13%) and lymphocytes (9%) was observed (Fig. 1). A bone marrow aspiration and biopsy were done. The aspiration was dry tapped and the biopsy showed a hypercelluarity (90%) for her age and more than 30% of all hema- topoietic cells replaced with immature cells. The immature cells showed high nuclear/cytoplasmic ratio, one or more prominent nucleoli, and fine nuclear chromatin. The myeloid series increased in proportion and revealed normal maturation.
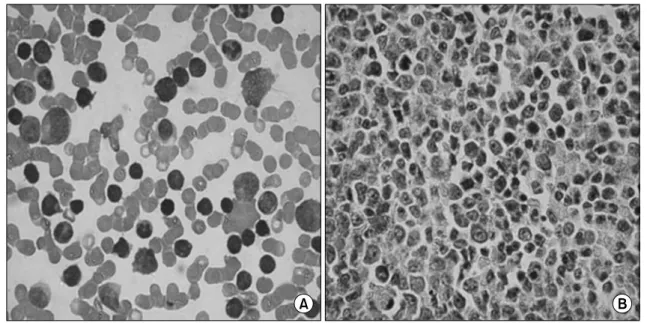
The megakaryocytes decreased in number (Fig.
2). Due to the dry tapping of bone marrow, the chromosomal study could not be performed. So the cytogenetic study for Philadelphia chromosome was done with peripheral blood. The immuno-
Fig. 2. Bone marrow biopsy. (A) Bone marrow biopsy imprint (touch preparation), More than 30% of all hematopoietic cells are replaced by immature cells. These cells show high nuclear/ cytoplasmic ratio, one or more prominent nucleoli, and fine nuclear chromatin. These cells also vary in size from medium to large. The myeloid series are increased in proportion and reveal normal maturation. The erythroid series are decreased in proportion and reveal normal maturation. The megakaryocytes are decreased in number. (B) The bone marrow section is hypercellular (90%) for her age. Immature cells are seen throughout section intermingled with other hematopoietic cells.
Table 1. Immunophenotyping result
Anti Anti Anti Anti Anti Anti Anti Anti Anti Anti Anti Anti
CD3 CD5 CD7 CD10 CD13 CD14 CD19 CD20 CD22 CD33 CD34 CD45
(-) (-) (-) (+) (+)* (-) (+) (-) (+) (-) (+) (+)
*CD13: abberant expression.
CD10: 80.38%, CD13: 58.05%, CD19: 77.94%, CD22: 68.66%, CD34: 85.32%, CD45: 93.64%.
phenotyping result of peripheral blood showed positive for CD10, CD19, CD 22 and CD34, that is, positive for B-lineage lymphocytic stem cells (Table 1). We considered two disease entities, such as CML in lymphoblastic crisis and ALL (Ph+). In peripheral blood, all series of cell linage were noted. So we preferred the diagnosis of CML in lymphoblastic crisis. Because of initial high uric acid and LDH levels, we considered a possibility of the development of tumor lysis syndrome.
Vigorous hydration and furosemide injection were done before the beginning of cytotoxic che- motherapy. We also administered 300mg of allo- purinol per day. At the follow-up laboratory fin-
dings after 2days, the level of uric acid was 8mg/
dL, BUN 16mg/dL, creatinine 1.7mg/dL, calci- um 10.6mg/dL, phosphorus 5.5mg/dL, LDH 1671IU/L, sodium 140mEq/L, potassium 2.8 mEq/L and chloride 99mEq/L.
Induction chemotherapy consisting of idaru- bicin, Ara-C, vincristine, methylprednosolone was done. Next day, the follow-up laboratory findings showed that the level of uric acid was 7.0mg/dL, BUN 43mg/dL, creatinine 1.8mg/dL, calcium 8.8 mg/dL, phosphorus 13.1mg/dL, LDH 3808IU/L, sodium 140mEq/L, potassium 7.1mEq/L and chloride 98mEq/L. We continued vigorous hydra- tion, and administered calcium gluconate, insulin mixed dextrose fluid and sodium polystyrene
laboratory findings, the level of uric acid was 4.4mg/dL, BUN 25mg/dL, creatinine 0.9mg/dL, calcium 8.8mg/dL, phosphorus 3.5mg/dL, LDH 555IU/L, sodium 139mEq/L, potassium 3.7mEq/
L and chloride 102mEq/L. Two weeks after the intiation of therapy, the presence of BCR/ABL fusion gene was confirmed in the peripheral blo- od previously examined and added imatinib (400mg per day). After the induction therapy, leukocyte count decreased to 4,600/μL, no imma- ture cells were observed on peripheral blood and platelet count was recovered to 282,000/μL. The bone marrow biopsy showed a normocellularity (70%) for her age and 3.2% of hematopoietic stem cells were immature cells. The splenome- galy disappeared. By the impression of clinical complete remission, the consolidation chemother- apy was started. After 2 cycles of therpy, the absence of BCR/ABL transcript by RT-PCR was noted on peripheral blood sample. She had an HLA-identical sibling donor, e.g. elder brother, but refused the allogenic bone marrow transplan- tation due to the risk and predicted of poor outcome of the procedure. At present, she is on the 3rd cycle of consolidation chemotherapy and has no sign and symptom of the disease.
DISCUSSION
Tumor lysis syndrome is defined as the me- tabolic derangements that occur with tumor brea- kdown following the initiation of cytotoxic thera- py. The syndrome can overwhelm the normal homeostasis and cause hyperuricemia, hyperkal- emia, hyperphosphatemia, secondary hypocalcemia and acute renal failure.1) While it may occur spontaneous prior to cytotoxic therapy, it is most commonly observed after the initiation of chemo- therapy. In tumors with a high proliferative rate, a large burden, and high sensitivity to chemo- therapy or radiotherapy, the treatment often results in the rapid release of intracellular anions, cations and the metabolic products of proteins
Cario and Bishop proposed the classification of tumor lysis syndrome, that is, laboratory tumor lysis syndrome (LTLS) and clinical tumor lysis syndrome (CTLS). LTLS is defined as either a 25% change or level above or below normal for any 2 or more serum values of uric acid, potas- sium, phophorus and calcium with 3 days before or 7 days after chemotherapy. And CTLS is defined as the presence of LTLS and any 1 or more of seizure, cardiac arrhythmia/sudden death and elevation of serum creatinine level (1.5 times over upper limit). Clinical manifestations may include nausea, vomiting, lethargy, edema, con- gestive heart failure, dysrhythmia, seizure, mu- scle cramps and sudden death. These may occur prior to therapy, but commonly present within 12
~16hr after the cytotoxic therapy.8)
The principles in the successful management of tumor lysis syndrome are maintaining a high index of suspicion, immediately identifying pa- tients at high risk and aggressive prophylactic efforts to prevent and/or reduce the severity of it.
So patients at risk should be treated with pro- phylactic measures before the administration of chemotherapeutic agents.7)
In a retrospective study of 722 patients with acute leukemia and non-Hodgkin's lymphoma (NHL), hyperuricemia occurs in 18.9% of pa- tients and a tumor lysis syndrome in 5%. Overall, 1.9% of patients died from the syndrome-related complications. In relation to the underlying mali- gnancy, the respective percentages were 2.5% in ALL patients, 2.2% in AML patients and 3.9%
in NHL patients.9)
Tumor lysis syndrome is most commonly ob- served following chemotherapy for high-grade lymphoproliferative malignancies such as acute lymphoblastic leukemia (ALL) and Burkitt's lym- phoma. Other hematologic malignancies that have been less commonly associated with it include chronic lymphocytic leukemia,10) acute myeloid leukemia and plasma cell disorders. And solid tumors such as testicular cancer, breast cancer
and small cell lung cancer are also associated with it.8) Rarely the syndrome was reported in patients with advanced gastric cancer, advanced hepatocelluar carcinoma, metastatic meduloblas- toma and prostatic cancer.2-5)
In addition, tumor lysis syndrome rarely occurs in patients with chronic myelogenous leukemia, especially in blast crisis. In a report, a patient with chronic myelogeous leukemia in accelerated phase who was treated with imatinib underwent an acute tumor lysis syndrome. The report has suggested that patient with CML in accelerated phase/blast crisis with leukocyte count >20,000/
μL should routinely be prescribed allopurinol and vigorous hydration and observed for the syn- dorme.11)
We report a case of chronic myelogenous leu- kemia in blast crisis associated with tumor lysis syndrome. Especially, it is a rare case in the point of tumor lysis syndrome associated with lympho- blastic crisis of CML.12) Maybe it is the first case report of tumor lysis syndrome associated with lymphoblastic crisis of CML in our country as far as we know. And we suggest that in patients with CML in blast crisis associated with high uric acid and LDH levels, the possibility of tumor lysis syndrome should be considered and aggressively treated.
REFERENCES
1) Davidson MB, Thakkar S, Hix JK, Bhandarkar ND, Wong A, Schreiber MJ. Pathophysiology, clinical con- sequences, and treatment of tumor lysis syndrome. Am J Med 2004;116:546-54.
2) Woo IS, Kim JS, Park MJ, et al. Spontaneous acute tumor lysis syndrome with advanced gastric cancer. J Korean Med Sci 2001;16:115-8.
3) Lee CC, Wu YH, Chung SH, Chen WJ. Acute tumor lysis syndrome after thalidomide therapy in advanced hepatocellular carcinoma. Oncologist 2006;11:87-8.
4) Baeksgaard L, Sorensen JB. Acute tumor lysis syndro- me in solid tumors--a case report and review of the literature. Cancer Chemother Pharmacol 2003;51:
187-92.
5) Wright JL, Lin DW, Dewan P, Montgomery RB.
Tumor lysis syndrome in a patient with metastatic, androgen independent prostate cancer. Int J Urol 2005;12:1012-3.
6) Chen SW, Hwang WS, Tsao CJ, Liu HS, Huang GC.
Hydroxyurea and splenic irradiation-induced tumour lysis syndrome: a case report and review of the liter- ature. J Clin Pharm Ther 2005;30:623-5.
7) Spinazze S, Schrijvers D. Metabolic emergencies. Crit Rev Oncol Hematol 2006;58:79-89.
8) Cairo MS, Bishop M. Tumour lysis syndrome: new therapeutic strategies and classification. Br J Haematol 2004;127:3-11.
9) Annemans L, Moeremans K, Lamotte M, et al. Inci- dence, medical resource utilisation and costs of hyper- uricemia and tumour lysis syndrome in patients with acute leukaemia and non-Hodgkin’s lymphoma in four European countries. Leuk Lymphoma 2003;44:77-83.
10) Hussain K, Mazza JJ, Clouse LH. Tumor lysis syn- drome (TLS) following fludarabine therapy for chronic lymphocytic leukemia (CLL): case report and review of the literature. Am J Hematol 2003;72:212-5.
11) Vora A, Bhutani M, Sharma A, Raina V. Severe tumor lysis syndrome during treatment with STI 571 in a patient with chronic myelogenous leukemia accele- rated phase. Ann Oncol 2002;13:1833-4.
12) Przepiorka D, Gonzales-Chambers R. Acute tumor lysis syngdrome in a patient with chronic myelogenous leu- kemia in blast crisis: role of high-dose Ara-C. Bone Marrow Transplant 1990;6:281-2.