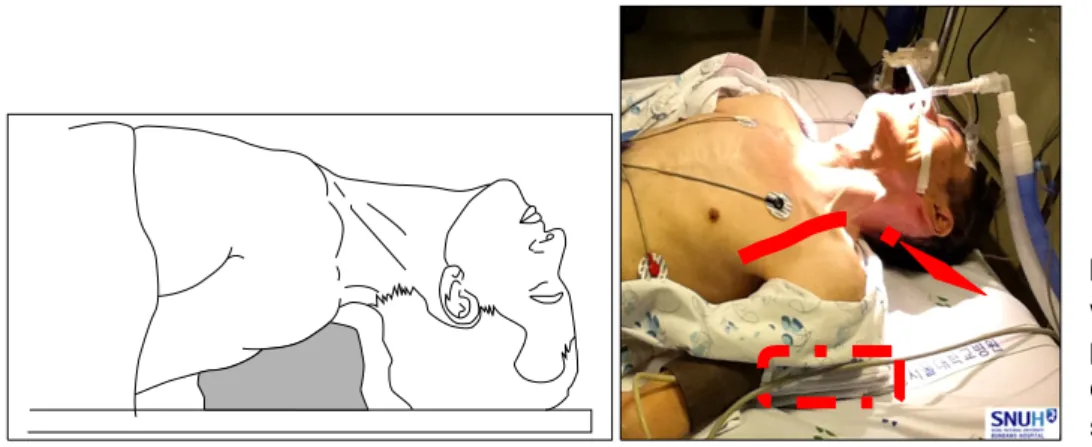
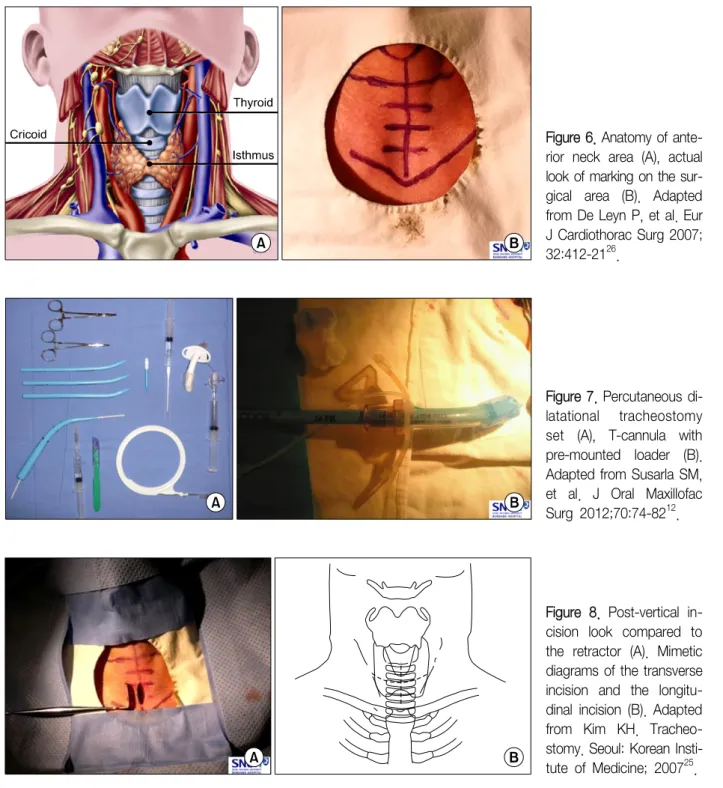
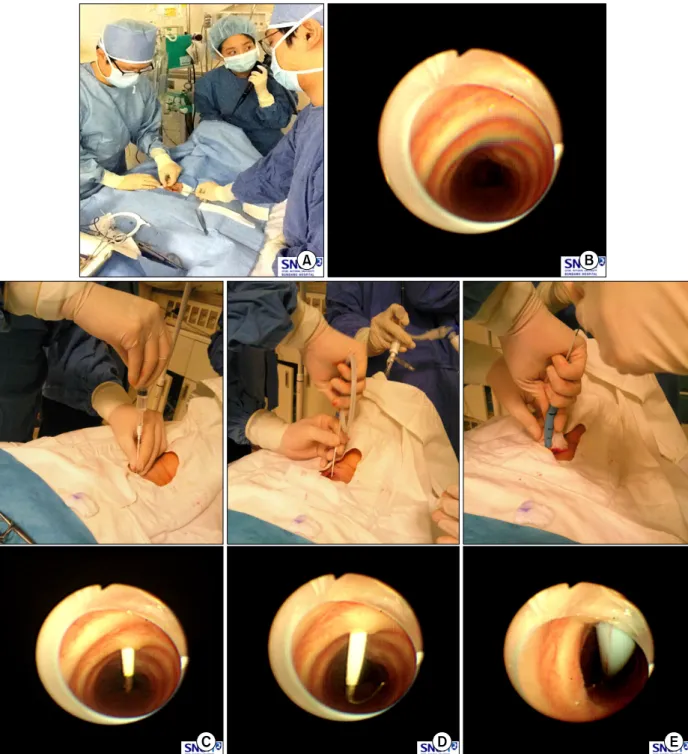
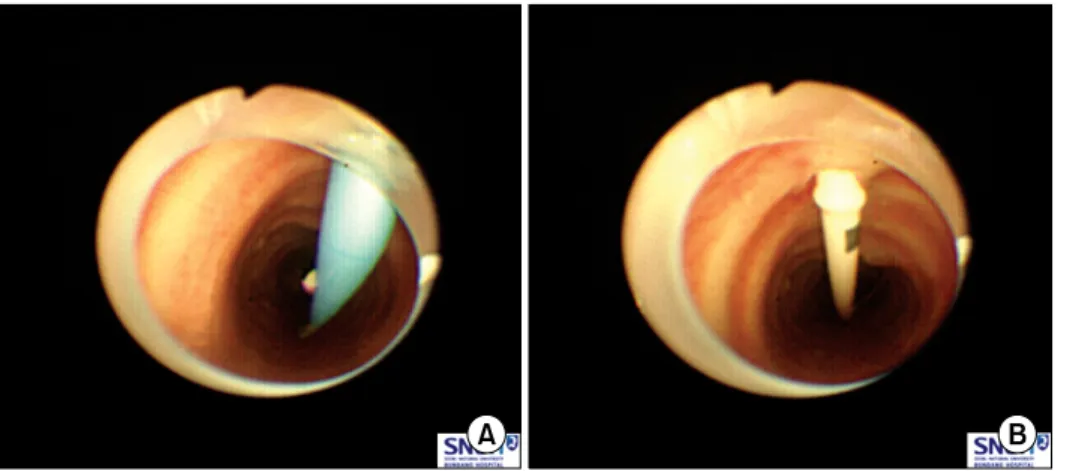
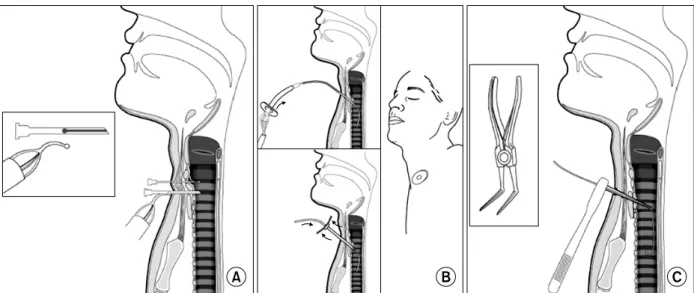
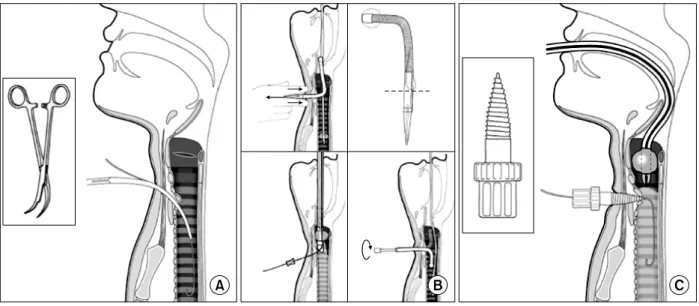
Percutaneous Dilatational Tracheostomy
전체 글
수치
관련 문서
A new intravenous fat emulsion containing soybean oil, medium-chain triglycerides, olive oil, and fish oil: a single-center, double-blind randomized study
(2002) Blinded, randomized, multicenter study to evaluate single administration pegfilgrastim once per cycle versus daily filgrastim as an adjunct to chemotherapy in
For Kummell’s disease with persistent pain and without neurological symptoms, percutaneous vertebroplasty (VP) or balloon kyphoplasty (KP) has been known to
The preparation of osseodensification technique should start with a smaller diameter than conventional technique because of the recovery of elastic strain. It
With uses of a techniques named mola that pursues modern and Korean image by overlapping of cloth with various colors, and a technique named slash that
Pelvic floor muscle training versus no treatment for urinary incontinence in women.. Acute back pain: a control-group comparison of behavioral vs
Background The aim of this study was to compare the surgical outcomes of robotic single-site (RSS-H) and laparoendoscopic single-site total hysterectomy (LESS-H) and to
Keywords: decompression; discogenic low back pain; epidurography; intervertebral disc dis- placement; low back pain; lumbar radicular pain; nucleoplasty; outcome;