103
The Prognostic Significance of Carotid Intima-Media Thickness in Patients Who Underwent Percutaneous Coronary Intervention
Taek-Geun Kwon, MD, Ki-Hong Kim, MD, Hyun-Ju Yoon, MD, Dae-Woo Hyun, MD and Jang-Ho Bae, MD
Cardiology Division, Heart Center, Konyang University Hospital, Deajeon, Korea ABSTRACT
Background and Objectives:Increased carotid intima-media thickness (IMT) is known to be associated with adverse cardiovascular events in the patients with risk factors or established atherosclerosis. However, the prognostic importance of carotid IMT is uncertain in the patients who underwent percutaneous coronary intervention (PCI).
We sought to evaluate the association of carotid IMT with major adverse cardiovascular events (MACE) and restenosis in the patients who underwent PCI. Subjects and Methods:The study population consisted of 308 consecutive patients who underwent PCI, and they were followed up for mean of 30.6±13.3 months. Base on the median values of carotid IMT, which was measured in the right common carotid artery at the time of PCI with using high-resolution ultrasound and a semiautomatic method, the subjects were divided into the thick (n=156, 1.003±0.14 mm) and thin IMT (n=152, 0.748±0.07 mm) groups, and they were followed up for at least 1 year. Results:Patients with thick carotid IMT were older (61±9 years vs. 57±10 years, respectively, p=0.001), had a higher body mass index (25.0±3.0 vs. 23.9±4.0, respectively, p=0.017), a history of previous myocardial infarction (20% vs. 9%, respectively, p=0.008), more multivessel disease and more restenosis (34.6% vs. 23.0%, respectively, p=0.025) than those patients with a thin carotid IMT. However other MACEs such as death, myocardial infarction, stroke, heart failure and target lesion revascularization did not show any significant differences between the two groups. Multivariate Cox regression analysis showed that carotid IMT was an independent predictor of restenosis (odds ratio: 1.754, 95% confidence interval: 1.1296 to 2.726, p=0.012). Conclusion:An increased carotid IMT is associated with restenosis, but it does not have clinical prognostic importance for the patients who underwent PCI during a mean follow up period of 31 months.(Korean Circulation J 2007;37:103-107) KEY WORDS:Carotid arteres;Angioplasty, transluminal, percutaneous coronary;Prognosis.
Introduction
The carotid intima-media thickness(IMT) is increased in patients who are at risk for cardiovascular disease and in those patients with atherosclerotic disease such as coronary artery disease(CAD), and IMT is well known as a noninvasive surrogate marker of atherosclerosis.1-8) Carotid IMT has also been reported to be associated with the extent or severity of CAD.9-12) Furthermore, O’Leary et al.13) reported that an increased carotid IMT is associated with a higher risk of stroke and acute myo- cardial infarction(AMI) in an elderly population and it
is also a more powerful predictor of cardiovascular disease than the conventional risk factors for atherosclerosis.
The Framingham heart study showed that carotid IMT is independently associated with the 10-year coronary heart disease risk, which supports its usefulness as a prognostic marker.14)
However, the prognostic significance of carotid IMT in patients underwent percutaneous coronary intervention (PCI) has not been reported. The aim of this study was to evaluate the association of carotid IMT with major adverse cardiovascular events(MACE) and restenosis in the patients underwent PCI.
Methods
Study populationWe enrolled a total of 308 consecutive patients who underwent PCI at the catheterization laboratory at Konyang University Hospital, Daejeon, Korean, from 11
Received:January 9, 2007 Accepted:February 21, 2007
Correspondence:Jang-Ho Bae, MD, Cardiology Division, Heart Center, Konyang University Hospital, 685 Gasoowon-dong, Seo-gu, Daejeon 302-718, Korea
Tel: 82-42-600-9420, Fax: 82-42-600-9400 E-mail: janghobae@yahoo.co.kr
March 2002 to 3 December 2004. All the patients had their carotid IMT measured at the time of PCI. The baseline demographic, clinical and angiographic charac- teristics were gathered by trained research technicians.
Informed consent was obtained from all the participating patients. Those patients who were hemodynamically unstable, and those with life-threatening malignancy, other severe combined disease or poor quality of their carotid image, those lost to follow up or those who refused study procedures were excluded. The study protocol was approved by the hospital ethics committee.
Carotid artery scanning
Carotid artery scanning was performed with a high- resolution ultrasonographic unit(Hewlett-Packard Sonos- 5500), equipped with a 7.5 MHz linear array transducer, and with the subjects in the supine position. An ECG signal was synchronized to the end of diastole for image analysis. All ultrasonographic examinations were per- formed by one specially trained technician, who was unaware of the study subjects’ clinical information.
The carotid artery IMT was defined as the distance from the leading edge of the lumen-intima interface to the leading edge of the media-adventitia interface of the far wall. The IMT was measured in a 10 mm long seg- ment just proximal to the carotid bulb in the common carotid artery with using a semi-automatic technique with MATH® software(version 2.01, METRIS Co., Argenteuil, France). This computerized detection technique is 4 times more precise than ordinary calliper measurements for determining the carotid IMT.15)
Percutaneous coronary intervention
Patients were premedicated with aspirin(at least 100 mg) and unfractionated heparin(5,000 to 10,000 IU).
A loading dose of 300mg clopidogrel was administered before PCI. Coronary angiography(CAG) was performed through the femoral or radial artery by using standard technique. Stent implantation was performed if the residual stenosis was over 50% after balloon angioplasty.
Bare metal stents were mostly implanted(78.9%) during this study period(Table 1). Angiographically successful results were achieved in all the patients without any significant complications in the catheterization room such as hypotension requiring intraaortic balloon pum- ping, myocardial infarction, loss of a side branch, stroke and death.
Follow-up
Clinical follow-up was performed for at least 1 year (mean: 30.6±13.3 months) and follow-up CAG was planned at 6 months. Combined antiplatelet therapy included daily administration of aspirin(100 mg) and clopidogrel(75 mg). Dual antiplatelet therapy was rec- ommended for at least 6 months for the patients with
bare metal stent and for at least 1 year for the patients with drug eluting stent. Adverse events were documented by making phone calls to the patients and by reviewing the hospital records. MACEs were defined as death from cardiovascular events, AMI, stroke, target lesion revas- cularization and hospitalization with congestive heart failure(CHF).
The definition of AMI included two of the following three criteria; prolonged chest pain of more than 20 minutes, elevation of cardiac enzymes(CK, CK-MB or the relative index) more than 2 times the normal levels and ST-T wave changes or new Q waves on serial ECGs that were indicative of myocardial damage. Stroke was
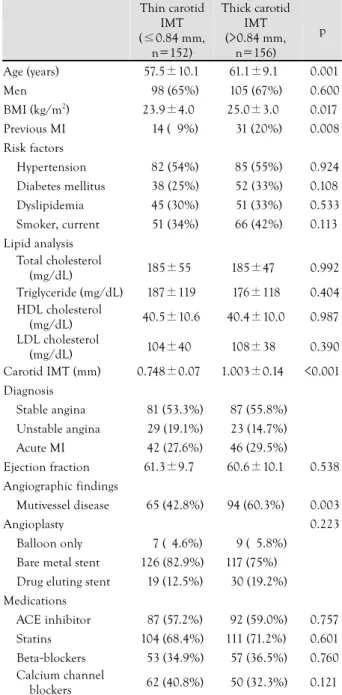
Table 1. Characteristics of the patients Thin carotid
IMT (≤0.84 mm,
n=152)
Thick carotid IMT (>0.84 mm,
n=156) p
Age (years) 57.5±10.1 61.1±9.11 0.001
Men 198 (65%) 105 (67%) 0.600
BMI (kg/m2) 23.9±4.01 25.0±3.01 0.017 Previous MI 114 (09%) 131 (20%) 0.008 Risk factors
Hypertension 182 (54%) 185 (55%) 0.924 Diabetes mellitus 138 (25%) 152 (33%) 0.108 Dyslipidemia 145 (30%) 151 (33%) 0.533 Smoker, current 151 (34%) 166 (42%) 0.113 Lipid analysis
Total cholesterol
(mg/dL) 185±550 185±471 0.992
Triglyceride (mg/dL) 187±119 176±118 0.404 HDL cholesterol
(mg/dL) 40.5±10.6 40.4±10.0 0.987
LDL cholesterol
(mg/dL) 104±400 108±381 0.390
Carotid IMT (mm) 0.748±0.070 1.003±0.140 <0.001 Diagnosis
Stable angina 181 (53.3%) 187 (55.8%) Unstable angina 129 (19.1%) 123 (14.7%) Acute MI 142 (27.6%) 146 (29.5%)
Ejection fraction 61.3±9.71 60.6±10.1 0.538 Angiographic findings
Mutivessel disease 165 (42.8%) 94 (60.3%) 0.003
Angioplasty 0.223
Balloon only 117 (14.6%) 119 (15.8%) Bare metal stent 126 (82.9%) 117 (75%).1 Drug eluting stent 119 (12.5%) 130 (19.2%) Medications
ACE inhibitor 187 (57.2%) 192 (59.0%) 0.757 Statins 104 (68.4%) 111 (71.2%) 0.601 Beta-blockers 153 (34.9%) 157 (36.5%) 0.760 Calcium channel
blockers 162 (40.8%) 150 (32.3%) 0.121 Values are means±SDs. IMT: intima-media thickness, BMI: body mass index, MI: myocardial infration, ACE: angiotensin converting enzyme, HDL: high density lipoprotein, LDL: low density lipoprotein
defined as a loss of neurological function caused by an ischemic event, and this loss persisted for more than 24 hours or it left residual signs, and hospitalization with CHF was defined as new symptoms of CHF or increased symptoms of CHF that required hospitalization. All deaths were considered to have been from cardiac causes unless a noncardiac cause could be identified. Restenosis was defined as stenosis of more than 50% of the luminal diameter on the follow-up CAG. Revascularization of the target lesion was defined as ischemia-driven PCI of the target lesion owing to restenosis or reocclusion within the stent or in the adjacent 5 mm of the distal or proximal segments.
Statistical analysis
The data is expressed as means±SDs or as frequencies (percentages). Patient characteristics between the two groups were compared using the t-test for continuous variables and the chi-square test for categorical variables.
Cumulative event rates were calculated according to the Kaplan-Meier method and the log-rank test. Cox regres- sion analyses were performed to determine the variables that were independently associated with restenosis. A p<0.05 was considered statistically significant. All ana- lyses were conducted with the use of statistical software (SPSS for Windows, version 11, SPSS Inc., Chicago, Illinois).
Results
Patient characteristicsThe study population consisted of 308 patients(203 males: 65.9%, mean age: 59.3±9.8 years. The carotid IMT ranged from 0.4 to 1.86 mm, with a mean(±SD) of 0.88±0.17 mm and a median of 0.85 mm. Base on the median values of carotid IMT, the subjects were divided into the thick(n=156, 1.003±0.14 mm) and thin IMT(n=152, 0.748±0.07 mm) groups. The patients with thick carotid IMT were older(61.1±9.1 vs. 57.5±
10.1, respectively, p=0.001), they had a higher body mass index(25.0±3.0 vs. 23.9±4.0, respectively, p=
0.017), and a higher prevalence of pervious myocardial infarction(20% vs. 9%, respectively, p=0.008), and mul- tivessel disease(42.8% vs. 60.3%, respectively, p<0.001) than those patients with thin carotid IMT. The other coronary risk factors did not show any significant dif- ference between the two groups. This may be explained as the study population consisted of patients with significant coronary artery disease that needed intervention. The baseline demographics of the study patients are summa- rized in Table 1.
Follow up
Clinical follow-up data were obtained from all the patients. During the 12 months of the clinical follow-up
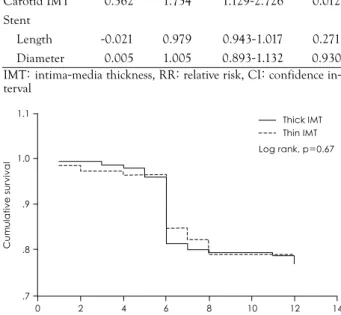
period, there was a total of 2 deaths, 5 acute myocardial infarctions, 59 target lesion revascularizations, 16 hospi- talizations with CHF and 6 strokes. In all, 88 patients experienced at least one MACE. The Kaplan-Meier survival curve showed no significant difference in MACE (cardiac death, AMI, target lesion revascularization, stroke and hospitalization with CHF) between the two groups (Fig. 1).
A total of 270 patients(87.7%) had follow-up CAG performed at a mean 6.0±1.4 months and the remain- ing 38 patients refused follow-up CAG because there
Table 2. Predictors of restenosis by multivariate Cox regression analysis
Beta RR 95% CI p
Age (years) -0.012 0.988 0.965-1.012 0.327 Male gender -0.244 1.277 0.787-2.071 0.322 Carotid IMT -0.562 1.754 1.129-2.726 0.012 Stent
Length -0.021 0.979 0.943-1.017 0.271 Diameter -0.005 1.005 0.893-1.132 0.930 IMT: intima-media thickness, RR: relative risk, CI: confidence in- terval
Cumulative survival
1.1
14 1.0
.9
.8
.7
0 2 4 6 8 10 12
Months
Thick IMT Thin IMT Log rank, p=0.67
Fig. 1. Kaplan-Meier curves for event-free survival showed that MACEs (cardiac death, acute myocardial infarction, target lesion revascular- ization and stroke) were not associated with carotid intima-media thickness (Thin IMT group; patients whose carotid IMT≤0.84 mm, Thick IMT group; patients whose carotid IMT>0.84 mm). MACEs:
major adverse cardiovascular events, IMT: intima-media thickness.
Fig. 2. Major adverse cardiovascular events were not different between the thick carotid IMT group (carotid IMT>0.84 mm) and the thin carotid IMT group (carotid IMT≤0.84 mm), except for restenosis.
*: p<0.05. AMI: acute myocardial infarction, CHF: congestive heart failure, TLR: target lesion revascularization, IMT: intima-media thickness.
Thin IMT Thick IMT
Event rate (%)
40
30
20
10
0 Death Stroke AMI CHF TLR Restenosis
*
was no clinical evidence of restenosis. Restenosis was more common in the patients with thick carotid IMT than in the patients with thin carotid IMT(34.6% vs.
23%, respectively, p=0.025)(Fig. 2). On multivariate Cox regression analysis, carotid IMT was an independent risk factor of restenosis even after adjustment for age, male gender, and the length and diameter of the stent(Odds ratio: 1.754, 95% confidence interval: 1.129 to 2.726, p=0.012)(Table 2).
Discussion
The present study shows that an increased carotid intima-media thickness in patients who underwent PCI was not related to an increased risk of MACE, but it was related to restenosis.
Carotid IMT has been recognized as a surrogate marker of atherosclerosis. It is associated with cardiovascular disease risk factors and CAD, and it is also associated with the outcomes of cardiovascular disease.1-8) However, the role of carotid IMT in secondary prevention is cur- rently undefined. But the relationship between carotid IMT and future cardiovascular events has been shown by several trials of patients with known coronary heart disease. In the Cholesterol Lowering Atherosclerosis Study trial, the risk of myocardial infarction or coronary death increased not only with increments of the carotid IMT, but also with the rate of progression of the carotid IMT.16) Therefore, by attenuating the carotid IMT pro- gression in patients with known CAD, therapies directed toward atherosclerosis such as statins, fibrates and niacin would improve the future cardiovascular risk.17-22) In our study, the baseline carotid IMT didn’t show any prog- nostic importance in patients who underwent PCI, except for restenosis. For secondary prevention, statins were prescribed not only to the patients with thick carotid IMT, but also to the patients with thin carotid IMT in our study(Table 1). This probably contributed the ap- parent lack of association of adverse events with the baseline carotid IMT.
Another main finding of this study was that carotid IMT is associated with restenosis. The incidence of an- giographic restenosis varies from 10% to 50% and it depends on the absence or presence of several risk factors such as female gender, diabetes mellitus and/or unstable angina pectoris. The angiographic risk factors for resteno- sis are stenosis of a longer length, chronic total occlusions and angiographically identifiable thrombus. Disease in saphenous vein grafts and in small native vessels(<3.0 mm) is associated with higher rates of restenosis. One of the leading predictors of angiographic stenosis after angioplasty is the postprocedural diameter.24) In our study, restenosis developed in 34.7% of the patients. The rel- atively high incidence of restenosis is explained that most of patients(78.9%) had bare metal stent implanted.
When we analyzed the risk factors for restenosis in the patients with implanted bare metal stent, only carotid IMT was an independent risk factor of in-stent restenosis after adjustment for the length and diameter of the stent.
This result suggests that a thick carotid IMT is another risk factor of in-stent restenosis after PCI. Inflammation is associated with in-stent restenosis25)26) and with carotid IMT.27-29) Although we did not evaluate inflammatory markers in the present study, an association between carotid IMT and in-stent restosis may be related to inflammation.
In conclusion, the present study suggests that an increased carotid IMT is independently associated with restenosis, but not with MACE in the patients who un- derwent PCI. Thus, carotid IMT is useful for predicting in-stent restenosis in the patients who underwent PCI, in addition to its role as a marker of atherosclerosis.
Study limitation
One year was too short to evaluate the prognostic power of carotid IMT in the patients who undergo PCI;
this needs more long-term follow up. We did not measure the carotid IMT on the follow-up study. Measurement of the regression of carotid IMT or attenuation of the carotid IMT progression may be better to evaluate the role of carotid IMT for secondary prevention. The res- ponse of carotid IMT to lipid lowering agents must be evaluated in a future study.
REFERENCES
1) Bae JH, Seung KB, Jung HO, et al. Analysis of Korean carotid intima-media thickness in Korean healthy subjects and patients with risk factors: Korea multi-center epidemiological study. Korean Circ J 2005;35:513-24.
2) O’Leary DH, Polak JF, Kronmal RA, et al. Thickening of the carotid wall: a marker for atherosclerosis in the elderly? Stroke 1996;27:224-31.
3) Mannami T, Konishi M, Baba S, Nishi N, Terao A. Prevalence of asymptomatic carotid atherosclerotic lesions detected by high- resolution ultrasonography and its relation to cardiovascular risk factors in the general popular of a Japanese city: the Suita study. Stroke 1997;28:518-25.
4) Jeong IB, Kim KY, Bae JH, et al. The carotid intima-media thickness as a screening test for coronary artery disease. Korean Circ J 2005;35:460-6.
5) Burke GL, Evans GW, Riley WA, et al. Arterial wall thickness is associated with prevalent cardiovascular disease in middle- aged adults: the Atherosclerosis Risk in Communities(ARIC) study. Stroke 1995;26:386-91.
6) Crouse JR, Goldbourt U, Evans G , et al. Risk factors and segment- specific carotid arterial enlargement in the Atherosclerosis Risk in Communities(ARIC) cohort. Stroke 1996;27:69-75.
7) Tonstad S, Joakimsen O, Stensland-Bugge E, et al. Risk factors related to carotid intima-media thickness and plaque in children with familial hypercholesterolemia and control subjects. Arterio- scler Thromb Vasc Biol 1996;16:984-91.
8) Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal- medial thickness is related to cardiovascular risk factors mea- sured from childhood through middle age: the Muscatine Study.
Circulation 2001;104:2815-9.
9) Park KR, Kim KY, Yoon SM, Bae JH, Seong IW. Correlation between intima-media thickness in carotid artery and the extent of coronary atherosclerosis. Korean Circ J 2003;33:401-8.
10) Grobbee DE, Bots ML. Carotid artery intima-media thickness as an indicator of generalized atherosclerosis. J Intern Med 1994;236:567-73.
11) Hulthe J, Wikstrand J, Emanuelsson H, Wiklund O, de Feyter PJ, Wendelhag I. Atherosclerotic changes in the carotid artery bulb as measured by B-mode ultrasound are associated with the extent of coronary atherosclerosis. Stroke 1997;28:1189-94.
12) Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation 1986;74:1399-406.
13) O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults.
N Engl J Med 1999;340:14-22.
14) Kieltyka L, Urbina EM, Tang R, Bond MG , Srinivasan SR, Be- renson GS. Framingham risk score is related to carotid artery intima-media thickness in both white and black young adults:
the Bogalusa Heart Study. Atherosclerosis 2003;170:125-30.
15) Barth JD. Which tools are in your cardiac workshop?: carotid ultrasound, endothelial function, and magnetic resonance imaging.
Am J Cardiol 2001;87:8A-14A.
16) Hodis HN, Mack WJ, LaBree L, et al. The role of carotid intima- media thickness in predicting clinical coronary event. Ann Intern Med 1998;128:262-9.
17) Crouse JR 3rd, Byington RP, Bond MG , et al. Pravastatin, lipids, and atherosclerosis in the carotid arteries(PLAC-II). Am J Cardiol 1995;75:455-9.
18) Hodis HN, Mack WJ, LaBree L, et al. Reduction in carotid ar- terial wall thickness using lovastatin and dietary therapy. Ann Intern Med 1996;124:548-56.
19) McMahon S, Sharpe N, Gamble G , et al. Effects of lowering average or below average cholesterol levels on the progression
of carotid atherosclerosis: results of the LIPID Atherosclerosis Substudy. Circulation 1998;97:1784-90.
20) Taylor AJ, Kent SM, Flaherty PJ, Coyle LC, Markwood TT, Ver- nalis MN. ARBITER: Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol: a randomized clinical trial comparing the effects of atorvastatin and pravastatin on carotid intima medial thickness. Circulation 2002;106:2055-60.
21) Taylor AJ, Sullenberger LE, Lee HJ, Lee JK, Grace KA. Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol(ARBITER) 2: a double-blind, placebo-controlled study of extended-release niacin on atherosclerosis progression in secondary prevention patients treated with statins. Circulation 2004;110:3512-7.
22) Pitt B, Byington RP, Furberg CD, et al. Effect of amlodipine on the progression of atherosclerosis and the occurrence of clinical events. Circulation 2000;102:1503-10.
23) Rajagopal V, Rockson S. Coronary restenosis: a review of me- chanisms and management. Am J Med 2003;115:547-53.
24) Buffon A, Liuzzo G , Biasucci LM, et al. Preprocedural serum levels of C-reactive protein predict early complications and late restenosis after coronary angioplasty. J Am Coll Cardiol 1999;
34:1512-21.
25) Hojo Y, Ikeda U, Katsuki T, et al. Interleukin 6 expression in coronary circulation after coronary angioplasty as a risk factor for restenosis. Heart 2000;84:83-7.
26) Amar J, Fauvel J, Drouet L, et al. Interleukin 6 is associated with subclinical atherosclerosis: a link with soluble intercellular adhesion molecule 1. J Hypertens 2006;24:1083-8.
27) Sander D, Schulze-Horn C, Bickel H, Gnahn H, Bartels E, Conrad B. Combined effects of hemoglobin A1c and C-reactive protein on the progression of subclinical carotid atherosclerosis. Stroke 2006;37:351-7.
28) Elkind MS, Rundek T, Sciacca RR, et al. Interleukin-2 levels are associated with carotid artery intima-media thickness. Atheros- clerosis 2005;180:181-7.