관련 문서
• A predictor of patient’s survival and technical survival - high solute transport: mortality risk↑. - less UF, high protein
Post-surgical use of radioiodine (131I) in patients with papillary and follicular thyroid cancer and the issue of remnant ablation: a consensus
Here, we found that TAMR-MCF-7 cells had undergone EMT, evidenced by mesenchymal-like cell shape, down-regulation of the basal E-cadherin expression
Patient had laparoscopic surgery on the adnexal tumor and excised tissue was removed through Douglas pouch incision by single surgeon.. Results: The mean age
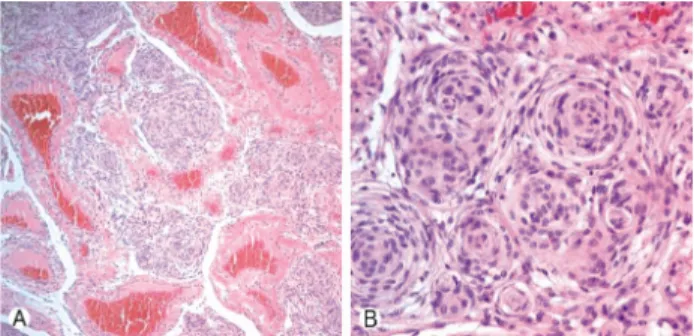
Purpose: Giant cell tumor of the tendon sheath are the most common tumors after ganglionic cysts in benign soft tissue tumors which could be recurred after surgical
Conclusion: Aromatherapy with neroli essential oil had a difference in brain wave and brain utilization ability according to the MBTI personality type
Sometimes called a direct neural interface or a brain-machine interface, is a direct communication pathway between a brain (or brain cell culture) and an external device..
Conclusions : No significant corelation of the patency rate was shown in the study on the effects of local irrigation and systemic application of heparin