분지병변에서 측부간지 폐쇄의 기전에 대한 혈관내 초음파 연구
굿모닝병원 순환기내과1, 국민건강보험 일산병원 심장내과2
이원경
1, 오성진
2, 문용선
2, 전동운
2, 양주영
2Mechanisms of Side Branch Jailing with Stenting at Bifurcation Lesions:
Volumetric Intravascular Ultrasound Analysis
Won Kyung Lee
1, Seung Jin Oh
2, Yong Seon Moon
2, Dong Woon Jeon
2, Joo Young Yang
21Division of Cardiology, Good Morning Hospital, Pyeongtaek,
2Division of Cardiology, Department of Internal Medicine, National Health Insurance Corporation Ilsan Hospital, Goyang, Korea
Background: Although plaque shift is believed to be the principal mechanism of side branch (SB) jailing in the percutaneous coronary intervention (PCI) of bifurcation lesions, objective evidence is lacking.
Methods: We analyzed volumetric intravascular ultrasound parameters before and after PCI in 55 bifurcation lesions. The lesions were classified into jailed (n=23) or patent group (n=32) according to SB jailing occurrence. Cross sections were analyzed by 1 mm intervals in segments that were 5 mm proximal and distal to the SB ostium, and were analyzed separately (proximal vs.
distal portion).
Results: Before PCI, the distal portion of the jailed group showed significantly smaller lumen and external elastic lamina (EEM) volume than the patent group (19.8±6.8 vs. 28.4±11.0 mm3, 43.8±11.1 vs. 53.6±13.4 mm3, respectively; p=0.006, 0.002), whereas plaque and media (P&M) volume did not differ between groups (24.0±11.8 vs. 25.1±11.2 mm3, p=0.73). All parameters related to the proximal portion were similar in both groups. After PCI, lumen volume of the distal portion increased significantly more in the jailed group than the patent group (+16.7±10.0 vs. +11.0±8.5 mm3, p=0.026). This was mainly derived from EEM volume expansion (49.5 to 60.4 mm3, p<0.001) than from P&M volume reduction (24.7 to 22.3 mm3, p=0.012). The proximal portion showed no significant differences in mean changes of EEM, lumen, and P&M volume between groups.
Conclusion: Instead of plaque shift, over-expansion of the distal relative to the proximal portion of a bifurcation lesion, which shifts the carina toward the SB, may be the main mechanism of SB jailing.
Key Words: Intravascular ultrasound, Percutaneous coronary intervention, Bifurcation
책임저자: 오성진
10444 경기도 고양시 일산동구 일산로 100 국민건강보험 일산병원 심장내과 전화 : (031)900-3164, 팩스 : (031)900-0639 E-mail : osjwsa@naver.com
INTRODUCTION
Percutaneous coronary intervention (PCI) of bifurcation lesions has always been challenging. Despite the initial expecta- tion that drug-eluting stents would finally address this longs- tanding problem, various techniques involving complex two- stent strategies have failed to prove their superiority over the single-stent strategy in terms of short- and long-term out-
comes.1,2 Thus, the single-stent strategy remains the standard treatment for these lesions despite its consistent association with a high incidence of procedural complications, such as side branch (SB) jailing and peri-procedural myocardial infarction.3,4 Also, Side branch predilatation before main vessel stenting may be associated with an increased risk of repeat revasculari- zation in patients with true nonleft main bifurcation.5 Several studies aimed at identifying the mechanism and predictors of SB jailing have been based solely on angiographic quantitative coronary analysis (QCA) despite the fact that intravascular ultrasound (IVUS) has already provided in-depth information in other various lesion subsets.6,7 Therefore, we investigated the underlying mechanism and potential predictors of SB jailing by means of volumetric IVUS analysis.
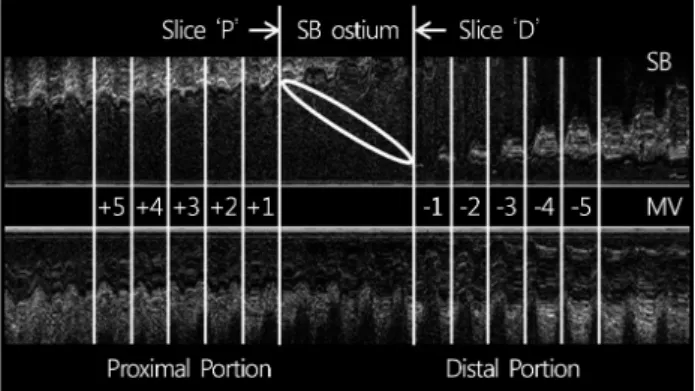
Fig. 1. Schematic representation of study segments within the proximal and distal portions in a bifurcation lesion. The proximal and distal slices of the side branch ostium (‘P’ and ‘D’) are shown.
MATERIALS AND METHODS
1. Patient populationWe identified in our institutional database a total of 98 con- secutive de novo bifurcation lesions that were treated with single-stent implantation in the main vessel across the SB and that underwent both pre- and post-stenting (before additional intervention, such as kissing balloon dilatation or SB stenting) IVUS imaging. We exclusively included lesions without SB ostial disease (reference diameter >2.5 mm and % diameter stenosis
<50% on QCA of SB) to rule out the influence of SB ostial plaque and to assess the pure effects of main vessel plaque movement. After reviewing IVUS images, lesions with inade- quate image quality secondary to severe calcification, insuffi- cient stented length to cover the study segments by protocol (5 mm proximal and distal to the SB ostium), or other side branch arising within the study segments were excluded. The remaining 55 lesions in 53 patients were included in this analy- sis. Prespecified clinical and procedural data were obtained from hospital charts. Written informed consent was obtained from all patients, and the study was conducted with the app- roval of the Institutional Review Board.
2. IVUS Image Analysis and Measurements IVUS imaging was performed in a standard fashion with commercially available equipment (Galaxy, Boston Scientific Inc., USA) and 3.0 Fr Atlantis imaging catheters (40 MHz).
Pre- and post-PCI IVUS analysis was performed using images acquired before pre-dilation and after high-pressure adjuvant ballooning (before final kissing balloon dilation, if conducted), respectively. Quantitative IVUS analysis was performed using computerized planimetry (Echo Plaque, Indec Systems, USA)
as follows. First, the pre-PCI image was reviewed to select the SB ostium of interest on the longitudinal view. The proximal and distal ends of the ostium were designated as slice ‘P’ and
‘D’, respectively. Then, the longitudinal view of the post-PCI image was reviewed side-by-side with the pre-PCI image to identify the corresponding slice ‘P’ and ‘D’. Finally, the study segment (from 5 mm proximal to the slice ‘P’ through 5mm distal to the slice ‘D’) was divided into 1mm intervals in both pre- and post-PCI images. Five proximal slices were numbered from the closest to slice ‘P’ as ‘+1’ to ‘+5’ and designated as the ‘proximal portion’ as a whole. Five distal slices were numbered from the closest to slice ‘D’ as ‘-1’ to ‘-5’ and designated as the ‘distal portion’ (Fig. 1). In each slice, the external elastic membrane (EEM) and lumen area were mea- sured and plaque and media (P&M) area, defined as EEM area minus lumen area, was calculated. Changes in EEM, lumen, and P&M areas before and after PCI were also calculated.
Volumetric analysis of these measurements was performed in the proximal and distal portions separately using Simpson’s rule according to recent AHA/ACC guidelines.8 IVUS studies were reviewed separately by the independent personnel (Y.S.M.), who had no knowledge of the occurrence of SB jailing.
3. Statistical Analysis
Statistical analysis was performed using SPSS, version 18.0.
(SPSS Inc., USA). Continuous variables are presented as mean values±SD and compared using paired or unpaired student t- tests, and Categorical variables are presented as frequency (%) and compared with Fisher’s exact test. Correlations between parameters were evaluated using the Pearson’s correlation analy- sis. A p<0.05 was accepted as significant.
RESULTS
A total of 55 lesions in 53 patients were included in this study. SB jailing after stent implantation occurred in 23 lesions, which comprised the jailed group, and they were compared with 32 lesions in the patent group. The clinical characteristics of the patients are shown in Table 1. Overall, mean age of patients was 65.5±10.7 years and most were male (72%). The target lesions were mainly located at the left anterior descen- ding/diagonal branch (92%). In two patients, more than one bifurcation lesion were treated in the same patient and analy- zed separately. The two groups were comparable in terms of clinical characteristics statistically. Results of Volumetric IVUS analysis are summarized in Table 2. Before PCI, the jailed group showed significantly smaller lumen and EEM volume at the distal portion than the patent group (19.8±6.8 vs. 28.4
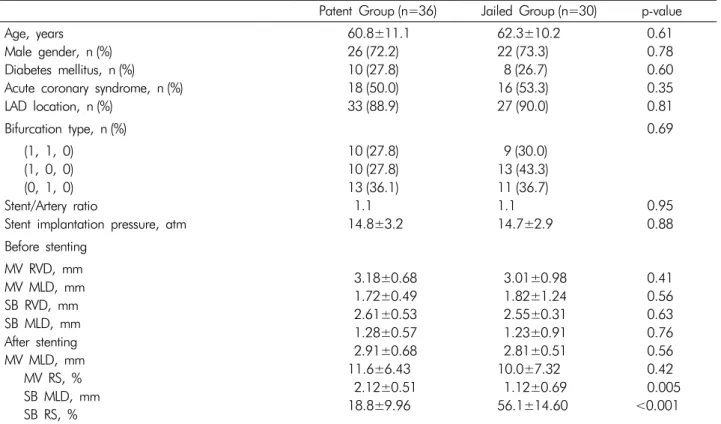
Table 1. Clinical and angiographic characteristics
Patent Group (n=36) Jailed Group (n=30) p-value Age, years
Male gender, n (%) Diabetes mellitus, n (%) Acute coronary syndrome, n (%) LAD location, n (%)
60.8±11.1 26 (72.2) 10 (27.8) 18 (50.0) 33 (88.9)
62.3±10.2 22 (73.3) 8 (26.7) 16 (53.3) 27 (90.0)
0.61 0.78 0.60 0.35 0.81
Bifurcation type, n (%) 0.69
(1, 1, 0) (1, 0, 0) (0, 1, 0) Stent/Artery ratio
Stent implantation pressure, atm
10 (27.8) 10 (27.8) 13 (36.1) 1.1 14.8±3.2
9 (30.0) 13 (43.3) 11 (36.7) 1.1 14.7±2.9
0.95 0.88 Before stenting
MV RVD, mm MV MLD, mm SB RVD, mm SB MLD, mm After stenting MV MLD, mm MV RS, % SB MLD, mm SB RS, %
3.18±0.68 1.72±0.49 2.61±0.53 1.28±0.57 2.91±0.68 11.6±6.43 2.12±0.51 18.8±9.96
3.01±0.98 1.82±1.24 2.55±0.31 1.23±0.91 2.81±0.51 10.0±7.32 1.12±0.69 56.1±14.60
0.41 0.56 0.63 0.76 0.56 0.42 0.005 <0.001 Values are presented as n (%) or mean±SD.
LAD, left anterior descending; MV, main vessel; SB, side branch; RVD, reference vessel diameter; MLD, minimal luminal diameter;
RS, residual stenosis.
Table 2. Results of Volumetric IVUS analysis
Volume, mm3 Patent Group (n=32) Jailed Group (n=23) p-value
Before stenting
Proximal EEM Proximal L Proximal P&M Distal EEM Distal L Distal P&M
69.13±15.43 34.02±11.11 35.12±14.42 53.55±13.35 28.42±10.96 25.13±11.15
63.03±15.05 28.39±12.58 34.64±9.76 43.83±11.06 19.80±6.78 24.04±11.76
0.15 0.09 0.89 0.006 0.002 0.73
After stenting
Proximal EEM Proximal L Proximal P&M Distal EEM Distal L Distal P&M
77.47±14.57 43.85±8.66 33.62±11.50 62.52±12.23 39.37±8.14 23.14±8.88
73.23±12.29 39.71±7.77 33.52±8.90 57.51±14.58 36.45±8.58 21.06±7.77
0.26 0.07 0.97 0.17 0.20 0.37
Volume change
Proximal EEM Proximal L Proximal P&M Distal EEM Distal L Distal P&M
+8.34±7.34 +9.83±12.21 -1.49±9.27 +8.97±7.31 +10.95±8.45 -1.99±7.46
+10.20±7.55 +11.32±12.18 -1.12±7.80 +13.68±6.76 +16.65±10.00 -2.97±6.11
0.36 0.66 0.88 0.019 0.026 0.61 Values are presented as mean ± SD.
EEM, external elastic lamina; L, lumen; P&M, plaque and media.
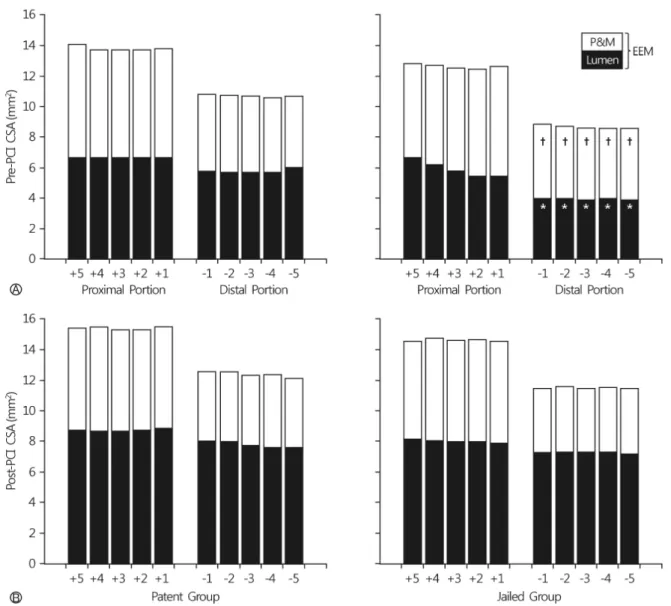
Fig. 2. The results of sub-segmental IVUS analysis. Panel A shows the pre-PCI measurements of EEM, lumen, and P&M CSA in the proximal and distal portions. In each stacked column, lumen is shown in black and P&M in white. EEM is represented by the total column. Panel B shows post-PCI measurements (*p<0.01 vs. Patent group; †p<0.05 vs. Patent group).
±11.0 mm3, 43.8±11.1 vs. 53.6±13.4 mm3, respectively; p=
0.006, 0.002). All parameters related to the proximal portion did not differ between groups and had no predictive value for SB jailing. After PCI, lumen and EEM volume of the distal portion increased significantly (24.8±10.3 to 38.1±8.4 mm3, 49.5±13.2 to 60.4±13.4 mm3, respectively; p<0.001) to a significantly greater extent in the jailed group compared with the patent group (+16.7±10.0 vs. +11.0±8.5 mm3, +13.7±
6.8 vs. +9.0±7.3 mm3, respectively; p=0.019). P&M volume of the distal portion was reduced (24.7±11.3 to 22.3±8.4 mm3, p=0.012), but the extent was not significantly different between groups (-2.97±6.11 vs. -1.99±7.46, p=0.61). The relative contribution of vessel expansion to lumen enlarge-
ment was 82.2%, and plaque reduction only accounted for 17.8% of luminal gain in the jailed group. Although lumen and EEM volume of the proximal portion were also increased (31.7±12.0 mm3 to 42.1±8.5 mm3, 66.6±15.4 mm3 to 75.7
±13.7 mm3, respectively; p<0.0001), P&M volume did not change and there were no significant differences in mean chan- ges of EEM, lumen, and P&M volume between groups. The sub-segmental IVUS analysis results are shown in Fig. 2. When pre-PCI IVUS images were analyzed by 1-mm intervals, signifi- cantly smaller lumen and EEM CSA were noted uniformly over the entire distal portion segments of the jailed group (p=0.98 by ANOVA). P&M CSA did not significantly differ between groups and it did not vary over the proximal through distal
portion. The changes in lumen, EEM and P&M volume after PCI were uniform over the length of the study segments in the patent group. In the jailed group, the increase in lumen volume was greatest in the 2 segments nearest from the SB ostium in the proximal portion and did not vary in the distal portion.
DISCUSSION
The present study demonstrates that vessel stretch at the distal portion of bifurcation is the major determinant of SB jailing after stenting in the false bifurcation lesions. Previous IVUS studies have reported that stent implantation expands coronary lumen not only by vessel stretch but also by plaque redistribution leading to plaque reduction at the center of lesion.9,10,11 This plaque moves longitudinally toward both ends of the lesion(plaque shift.12 However, conclusive data to con- firm the presence of plaque shift have not been reported. Most of the luminal gain was attributable to vessel stretch after sten- ting, and its extent at distal portion was related to occurrence of SB jailing. The discrepancy is most likely derived from seve- ral morphological differences unique to bifurcation lesions.
Unlike the non-bifurcation lesions, which usually have maxi- mum plaque at the center of lesion, atheroma usually exists at the opposite side of SB and spares the carina.13-15 In addi- tion, vessel dimension decreases abruptly after SB comes out, and “stepping down” of the luminal border exclusively locates at the side of carina.16 Consequently, as shown by the present data, stenting expands the lumen unequally and relatively over- expands the distal portion of the lesion. Another compelling source of evidence stems from the observation that small pre- PCI vessel and lumen dimension at the distal portion of the bifurcation lesion were the only identifiable predictors for SB jailing in the present study. On the other hand, the amount of plaque, either at the proximal or distal portion, was not predictive for SB jailing. Therefore, it is not surprising that stenting shifts the carina towards the SB ostium without any notable redistribution of plaque. Recently, a consensus docu- ment from the expert meeting focused on bifurcation lesion has proposed a tentative theory involving carina displacement as the main mechanism of SB jailing.17 This is based on several observational data including an angiographic study showing that carina displacement from stent struts is a major mecha- nism governing changes in coronary bifurcations after main vessel stenting.18 IVUS and fractional flow reserve measure- ments done by Koo et al also reported that lumen increase in the distal MB is primarily due to enlargement of the vessel and not plaque shift, supporting carina shift.19 However, these studies did not compare changes according to the presence of SB jailing so that it remained unclear whether carina shift
was an immediate cause of SB jail. Our IVUS analysis supports this theory by exclusively enrolling false bifurcation lesions and showing that the main component which compromises the SB ostium may be the outer margin of the distal portion, that is, the carina itself. The results from the present study have several clinical implications. Because lesions with smaller lumen on the distal portion of the bifurcation tend to be over- expanded with stenting and are vulnerable to SB jailing, side branch protection with another guide wire will be helpful as further intervention. Also, stent size determination according to the distal reference diameter may be reasonable to avoid SB jailing in those cases. Considering that the carina shift may be the main mechanism of SB jailing, expansion of the proxi- mal portion with the kissing balloon technique or POT (proxi- mal optimization technique)20 may be the best way to restore SB patency and maintain the stent dimension of the main vessel in case of SB jailing.
REFERENCES
1. Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, Gunnes P, Mannsverk J, Meyerdierks O, Rotevatn S, Nie- melä M, Kervinen K, Jensen JS, Galløe A, Nikus K, Vikman S, Ravkilde J, James S, Aarøe J, Ylitalo A, Helqvist S, Sjögren I, Thayssen P, Virtanen K, Puhakka M, Airaksinen J, Lassen JF, Thuesen L.; Nordic PCI Study Group. Randomized study on simple versus complex stenting of coronary artery bifurca- tion lesions: the Nordic bifurcation study. Circulation 2006;
114:1955-61.
2. Colombo A, Bramucci E, Saccà S, Violini R, Lettieri C, Zanini R, Sheiban I, Paloscia L, Grube E, Schofer J, Bolognese L, Orlandi M, Niccoli G, Latib A, Airoldi F. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurca- tions: Application of the Crushing Technique Using Sirolimus- Eluting Stents) Study. Circulation 2009;119:71-8.
3. George BS, Myler RK, Stertzer SH, Clark DA, Cote G, Shaw RE, Fishman-Rosen J, Murphy M. Balloon angioplasty of bifur- cation lesions: the kissing balloon technique. Cathet Cardio- vasc Diagn 1986;12:124-38.
4. Louvard Y, Lefèvre T, Morice MC. Percutaneous coronary intervention for bifurcation coronary disease. Heart 2004;90:
713-22.
5. Song PS, Song YB, Yang JH, Hahn JY, Choi SH, Choi JH, et al. Efecto en los resultados de la intervencio´n y los resultados clı´nicos a largo plazo de la predilatacio´n de la rama lateral para lesiones coronarias en bifurcacio´n tratadas con la te´
cnica de stent condicional. Rev Esp Cardiol. 2014;67:804-12.
6. Pilar Jiménez-Quevedo, Manel Sabaté, Dominick J. Angiolillo, Marco A. Costa, Fernando Alfonso, Joan Antoni Gómez-Hos- pital, Rosana Hernández-Antolín, Camino Bañuelos, Javier Goi- colea, Francisco Fernández-Avilés, Theodore Bass, Javier Esca- ned, Raul Moreno, Cristina Fernández, Carlos Macaya and
DIABETES Investigators. Vascular Effects of Sirolimus-Eluting Versus Bare-Metal Stents in Diabetic Patients: Three-Dimen- sional Ultrasound Results of the Diabetes and Sirolimus-Elu- ting Stent (DIABETES) Trial. J Am Coll Cardiol 2006;47:2172-9.
7. Oemrawsingh PV, Mintz GS, Schalij MJ, Zwinderman AH, Jukema JW, van der Wall EE Intravascular ultrasound gui- dance improves angiographic and clinical outcome of stent im- plantation for long coronary artery stenoses: final results of a randomized comparison with angiographic guidance (TULIP Study). Circulation 2003;107:62-7.
8. Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, Pinto FJ, Rosenfield K, Siegel RJ, Tuzcu EM, Yock PG. American College of Cardiology Clinical Expert Con- sensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol 2001;
37:1478-92.
9. Maehara A, Takagi A, Okura H, Hassan AH, Bonneau HN, Honda Y, Yock PG, Fitzgerald PJ. Longitudinal plaque redistri- bution during stent expansion. Am J Cardiol 2000;86:1069- 72.
10. Mintz GS, Pichard AD, Kent KM, Satler LF, Popma JJ, Leon MB. Axial plaque redistribution as a mechanism of percuta- neous transluminal coronary angioplasty. Am J Cardiol 1996;
77:427-430.
11. Ahmed JM, Mintz GS, Weissman NJ, Lansky AJ, Pichard AD, Satler LF, Kent KM. Mechanism of lumen enlargement during intracoronary stent implantation: an intravascular ultrasound study. Circulation 2000;102:7-10.
12. Choi SY, Tahk SJ, Kim HS, Lian ZX, Yoon MH, Yoo SY, Ahn SG, Chang HJ, Hwang GS, Shin JH, Choi BI. Predictors of Side Branch Occlusion Immediately after Coronary Sten- ting: an Intravascular Ultrasound Study. Korean Circ J 2002 Aug;32(8):655-65.
13. Ozer Badaka, Paul Schoenhagena, Taro Tsunodaa, William A.
Magyara, Jennifer Coughlina, Samir Kapadiab, Steven E. Ni- ssena and E. Murat Tuzcua. Characteristics of atherosclerotic plaque distribution in coronary artery bifurcations: an intra- vascular ultrasound analysis. Coronary Artery Disease 2003;
14:309-16.
14. Per Grøttum, Aud Svindland, Lars Walløe. Localization of Athe- rosclerotic Lesions in the Bifurcation of the Main Left Coro- nary Artery. Atherosclerosis 1983;47:55-62.
15. Frank J.H. Gijsen, Jolanda J. Wentzel, Attila Thury, Bram La- mers, Johan C.H. Schuurbiers, Patrick W. Serruys, Antonius F. van der Steen. A new imaging technique to study 3-D plaque and shear stress distribution in human coronary artery bifur- cations in vivo. Journal of Biomechanics 2007;40:2349-57.
16. Lansky A, Tuinenburg J, Costa M, Maeng M, Koning G, Popma J, Cristea E, Gavit L, Costa R, Rares A, Van Es GA, Lefevre T, Reiber H, Louvard Y, Morice MC. Quantitative angiographic methods for bifurcation lesions: a consensus sta- tement from the European Bifurcation Group; European Bifur- cation Angiographic Sub-Committee. Catheter Cardiovasc In- terv 2009;73:258-66.
17. Stankovic G, Darremont O, Ferenc M, Hildick-Smith D, La- ssen JF, Louvard Y, Albiero R, Pan M, Lefèvre T. Percutaneous coronary intervention for bifurcation lesions: 2008 consensus document from the fourth meeting of the European Bifurca- tion Club. EuroIntervention 2009;5:39-49.
18. Vassilev D, Gil R. Clinical verification of a theory for predi- cting side branch stenosis after main vessel stenting in coro- nary bifurcation lesions. J Interv Cardiol 2008;21:493-503.
19. Koo BK, Waseda K, Kang HJ, Kim HS, Nam CW, Hur SH, Kim JS, Choi D, Jang Y, Hahn JY, Gwon HC, Yoon MH, Tahk SJ, Chung WY, Cho YS, Choi DJ, Hasegawa T, Kataoka T, Oh SJ, Honda Y, Fitzgerald PJ, Fearon WF. Anatomic and functional evaluation of bifurcation lesions undergoing percu- taneous coronary intervention. Circ Cardiovasc Interv. 2010;
3:113-119
20. Legrand V, Thomas M, Zelisko M, De Bruyne B, Reifart N, Steigen T, Hildick-Smith D, Albiero R, Darremont O, Stan- kovic G, Pan M, Lassen JF, Louvard Y, Lefèvre T. Percuta- neous coronary intervention of bifurcation lesions: state-of- the-art. Insights from the second meeting of the European B-i furcation Club. EuroIntervention 2007;3:44-9.
21. Koo BK, Park KW, Kang HJ, Cho YS, Chung WY, Youn TJ, Chae IH, Choi DJ, Tahk SJ, Oh BH, Park YB, Kim HS. Phy- siological evaluation of the provisional side-branch interven- tion strategy for bifurcation lesions using fractional flow reserve.
Eur Heart J 2008;29:726-32.
22. Tyczynski P, Ferrante G, Moreno-Ambroj C, Kukreja N, Barlis P, Pieri E, De Silva R, Beatt K, Di Mario C. Simple versus com- plex approaches to treating coronary bifurcation lesions: direct assessment of stent strut apposition by optical coherence tomo- graphy. Rev Esp Cardiol 2010 Aug;63(8):904-14.