276
J Korean Assoc Maxillofac Plast Reconstr Surg 2012;34(4):276-279 pISSN:1225-4207 eISSN: 2233-7296
Case Report
RECEIVED May 5, 2012, REVISED June 1, 2012, ACCEPTED June 27, 2012 Correspondence to Jwa-Young Kim
Department of Oral and Maxillofacial Surgery, Hallym University Sacred Heart Hospital 22, Gwanpyeong-ro 170-gil, Dongan-gu, Anyang 431-070, Korea
Tel: 82-31-380-3875, Fax: 82-31-380-3872, E-mail: jwayoung@hanmail.net
CC
This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/
by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
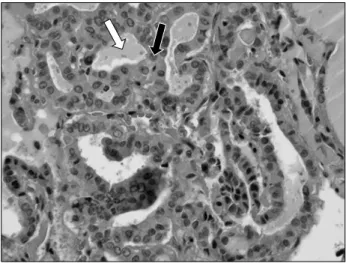
Gingival Squamous Carcinoma with Metastatic Lymph Node Involvement of Papillary Thyroid Carcinoma
Ju-Won Kim, Chang-Youn Lee, Seung-Min Oh, Byung-Eun Yang, Jwa-Young Kim, Yun-Jung Song 1 , Kang-Min Ahn 2 , Joo-Yong Park 3
Departments of Oral and Maxillofacial Surgery,
1Conservative Dentistry, Hallym University College of Medicine,
2
Department of Oral and Maxillofacial Surgery, Seoul Asan Medical Center, College of Medicine, University of Ulsan,
3