INTRODUCTION
Recent changes in demographic characteristics in Korea include prolonged activity in the workforce and regular participation of the middle-aged to the elderly in active sport activities. This phenomenon contributes to the increase in the prevalence of rotator cuff tears in the shoulders of adults. Full-thickness tears of the rotator cuffs may be either small-sized or middle-sized, and is accompanied by symptoms such as pain and muscle strength insufficiency. Night pain is especially prominent in patients with rotator cuff tears, and if prolonged, is
accompanied by shoulder stiffness [1]. Controversies as to the best treatment modality of rotator cuff tears exist. Conservative management is one of the treatment modalities that can be performed for 3 to 6 months, after which if there is no improvement in symptoms, as usually is the case for full-thickness tears, then surgical suture of the rotator cuff tears are performed. Although both the open and arthroscopic suture techniques, and a number of others, can be used for the repair, recent developments in suture materials and arthroscopic techniques highlight the efficacy of the arthroscopic technique in rotator cuff repairs. The authors carried out a prospective study Background: To prospectively compare the outcomes of an arthroscopic mattress locking (ML) suture repair and a simple suture repair of small or medium-sized rotator cuff tears.
Methods: The 92 patients who had received an unsuccessful conservative treatment of small or medium-sized rotator cuff tears between April 2007 and October 2010 and who required an additional arthroscopic treatment were enrolled in the study. The patients were arbitrarily divided into the type of arthroscopic repair they received; 27 patients who received the arthroscopic ML suture were put into group 1, and 65 patients who received the simple suture were put into group 2. The mean age of patients at the time of surgery was 58 years, and the mean duration to final follow-up was 30 months. To measure the outcome of the treatment, visual analogue scale (VAS) for pain (clinical score), UCLA, American Shoulder and Elbow Surgeons (ASES) and Korean shoulder scoring (KSS) for the range of motion (functional scores) were measured for each patient. Lastly, the magnetic resonance imaging (MRI) scans of the patient’s shoulder were taken at the final follow-up.
Results: Although the mean scores for clinical and functional outcomes (VAS, KSS, UCLA, and ASES scores) had improved from after the operation in both groups (P < 0.001), we found no significant differences in these improvements between the two groups (P > 0.001). Through MRI scans at the follow-up, we found that the proportion of re-tears was significantly lower in group 1 (2 patients, 7.41%) than in group 2 (12 patients, 18.46%).
Conclusion: We found no significant difference in the clinical or functional outcomes of an arthroscopic ML suture repair and the simple suture repair of small-sized or medium-sized rotator cuff tears after a follow-up period of at least one year. However, the proportion of re-tears was significantly lower in patients who received ML sutures than in patients who received simple sutures.
Keywords: Shoulder; Rotator cuff; Partial-thickness tears; Mattress locking suture; Simple suture
Arthroscopic mattress locking suture technique for the repair of small- and medium-sized rotator cuff tears
Sang-Hun Ko, Yun Jae Cho, Chang-hyun Youn, Hye-yong Cho, Jae-Ryung Cha
Department of Orthopedic Surgery, Ulsan University Hospital, Ulsan, Korea
Copyright © 2015 Korean Arthroscopy Society and Korean Orthopedic Society for Sports Medicine. All rights reserved.
CC This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/
by-nc/3.0) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received August 1, 2013; Revised May 24, 2014; Accepted May 26, 2014
Correspondence to: Jae-Ryung Cha, Department of Orthopedic Surgery, Ulsan University Hospital, 877 Bangeojinsunhwan-doro, Dong-gu, Ulsan 682-714, Korea. Tel: +82-52-250-7129, Fax: +82-52-235-2823, E-mail: jrcha@uuh.ulsan.kr
Arthroscopy and Orthopedic Sports Medicine
AOSM
to compare the outcomes when either an arthroscopic mattress locking (ML) suture technique or the simple suture technique was used to treat patients with small-sized or medium-sized rotator cuff tears. Clinical, functional, and radiological outcomes were assessed.
METHODS
Subjects of study
Patients with either a small- or medium-sized rotator cuff tear who had first been unsuccessfully treated by con- servative management between April 2007 and October 2010 and then required an additional arthroscopic treatment were selected for the study at Department of Orthopedic Surgery of Ulsan University Hospital. In all the patients, a probe needle was used to measure the depth of the tear and only the patients with tear size of 5 to 25 mm were considered for the study. A total of 92 patients, who were able to come to the final postoperative follow-up of at least one year, were enrolled in the study. The patients were arbitrarily divided into the type of arthroscopic treatment they received. Group 1 included 27 patients who received arthroscopic ML suture, and group 2 included 65 patients who received arthroscopic simple suture.
The mean age of patients was 58 years (range, 37–70 years) and the mean follow-up period was 30 months (range, 12–48 months). The study comprised of 39 male patients and 53 female patients. The rotator cuff tear occurred in the right shoulder for 52 patients and in the left for 40 patients; on the dominant side in 51 patients and on the non-dominant side in 41 patients.
Exclusion criteria
The exclusion criteria for this study were as follows;
patients with rotator cuff tears larger than 25 mm, patients with partial tears of the rotator cuff, patients who had a medical history of distal clavicle resection for acromioclavicular arthritis, patients who had labral reconstruction, patients who had resection or fixation of the long head of the biceps tendon, and lastly, patients who had a combined subscapsular muscle rupture that also needed suturing were all excluded from the study.
Assessment of treatment outcomes
Physical examination of each patient was performed at least 6 times over a period of a minimum 2 years; pre- operation, 4, 7, 10, 12, and 24 months postoperation. The shoulder range of motions (ROMs), forward elevation,
lateral external rotation, and posterior internal rotation, were also assessed. To measure the clinical outcome, the subjective visual analogue scale (VAS) for pain was taken, and to measure the functional outcome, UCLA, American Shoulder and Elbow Surgeons (ASES), and Korean shoulder scoring (KSS) were taken. These scores for were also taken at the time of physical exami nation. To measure the extent of tendon repair, magnetic resonance imaging (MRI) scans were taken of all the patients between the 4th and 6th postoperative month.
Surgical methods
A single surgeon performed the arthroscopic treatment in all the study subjects. Under general anesthesia, the affected shoulder joint was exposed and then an arthroscopic suture of the rotator cuff tear was performed.
The patient was beach-chair position throughout the surgery. To minimize loss of blood, we used hypotensive anesthesia using a pump to keep the pressure constant and 3,000 mL saline solution that was diluted to 1 : 1,000 with 1 mL of epinephrine (up to the first 5 solutions) were used. A 5 mm posterior portal was made at a position 2 cm posterior and 1.5 cm lateral to the acromion, through which an arthroscope was inserted towards the gle no- humeral joint. Then, this posterior portal was used to make the anterior portal. First, a blunt obturator was in- serted through the posterior portal. This obturator could be seen pushing against the subcutaneous layer on the opposite side, and a 5 mm excision was made around this bump. Then, a 4.5 mm gray cannula (Linvatec, Largo, FL, USA) was inserted following this obturator. Through these portals, the upper subscapular muscles, upper long head of the biceps, upper labral muscles, and the rotator cuffs were arthroscopically examined. Then, the obturator was directed towards the subacromial bursitis, and the hypertrophied bursitis was removed to arthroscopically examine the rotator cuffs again. Once the lesion of the rotator cuff was arthroscopically diagnosed, a portion for tissue biopsy was taken and then a reparative suture was made. To aid healing of the tear, a 2 to 2.5 mm debride- ment was also made in the center.
The ML suture was performed on group 1 patients. First, a suture lasso (SutureLasso; Arthrex, Naples, FL, USA) was inserted through the anteroportal, then a suture was made from the 1 to 1.5 cm medial edge of the rotator cuff tear to 0.5 to 1 cm distal to the tear. Then, a No. 1 polydioxanone suture (PDS; Ethicon, Somerville, NJ, USA) was inserted, and using this as a pincer, the PDS itself and the suture
lasso were pulled out through the anterosuperior portal.
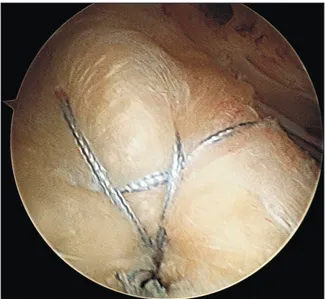
The PDS that was taken out was used to make a shuttle- relay with a strong wire (FiberWire or TigerWire; Arthrex), then it is reverse-inserted towards the rotator cuff (Fig. 1A).
To make a shuttle relay using the PDS, first a suture material was inserted using a separate suture hook from the posterior portal to the anterior side of the rotator cuffs.
Through this, the PDS that was already inside was passed out through the anterosuperior portal. The shuttle-relay was made by connecting the PDS with a premade strong wire. The shuttle relay was then pulled from the opposite side. Thus, a horizontal mattress was made as the PDS went across the anterior side of the rotator cuff (Fig. 1B, C) and when each ends of the FiberWire were pulled
out through the anterosuperior portals. The two vertical hooks on the horizontal mattress helped the tissues of the rotator cuff tendon to remain intact. In the completed suture, the horizontal mattress acted like a checkrein. If needed, interference screws were fixed to the suture from the lateral side (around 0.5 cm away) of the rotator cuff tendon (Fig. 2). In this study, either a PushLock (Arthrex) or a PopLock (Linvatec) was used, and the average number used was 1 to 2 (average 1.9).
The simple suture technique was performed on group 2 patients. First, a suture screw (Bio-FASTak; Arthrex) was inserted into the greater tuberosity. A single bundle of the strong wire (FiberWire or TigerWire), which was connected to the suture screw, was pulled out through the anterosuperior portal. A suture was made at a region 1 cm from the edge of the rotator cuff tear when the PDS, which was connected to the strong wire, was pulled out through the anterosuperior portal and the strong wire was pulled out from the opposite end. To finish the suture, a Samsung Medical Center knot or Revo knot was made to tie it up.
Rehabilitation
An abduction brace was administered for 6 weeks post- operation to promote slight abduction of the humeral bone.
Immediately after the operation, active movement of the wrist and elbow joints was promoted. On the subsequent day, the patients began their rehabilitation exercises of pendulum-like motion and active forward elevation motion. To restore normal shoulder ROM, the patients did active assisted ROM exercises for 8 weeks and active ROM exercises thereafter. After 10 to 12 weeks of the operation, the patient began muscle strengthening exercises.
Fig. 1. (A) Suture material is passed through the rotator cuff using the first polydioxanone suture (PDS). (B) The opposite end of the suture material is passed through the rotator cuff using the second PDS. (C) A horizontal mattress loop is made.
A B C
Anterior portal
Anterosuperior portal
Posterior portal
Anterosuperior portal
Anterior portal Posterior portal Anterior portal
Fig. 2. An arthroscopic subacromial view shows the mattress locking suture configuration after inserting an anchor.
Statistical analysis
All statistical analysis was performed using SPSS for Windows 12.0 (SPSS Inc., Chicago, IL, USA). Physical examination and assessment of patients’ shoulder ROM were performed preoperation, and at 4, 7, 10, 12, and 24 months postoperation. The VAS, UCLA, KSS and ASES scores of the patients were also taken at these time points but an observer who did not take part in the surgery took the measurements. The Student’s t-test was used to compare the means of the clinical and functional results of the two groups and statistical significance was determined using the 95% confidence interval.
RESULTS
Clinical outcomes
Demographic comparisons of the two groups showed that there were no significance differences between the groups in terms of sex, age, symptom duration, and of fatty degeneration in muscles (P > 0.001). In group 1, the VAS score improved from a preoperative mean ± standard deviation value of 7.23 ± 1.49 to a postoperative mean value of 2.00 ± 2.75. Likewise, group 2 showed an improved VAS score from a preoperative mean value of 7.74 ± 1.73 to a postoperative mean value of 3.00 ± 1.65 (P < 0.001).
However, the difference between the change in VAS scores of the two groups was insignificant (P > 0.001). As for the VAS score, the KSS score improved from 47.37 ± 5.65 to 87.81 ± 6.73 in group 1, and from 46.79 ± 6.45 to 86.28 ± 6.13 in group 2 (P < 0.001). Again, the difference between the change in KSS scores of the two groups was insignificant (P > 0.001). Similarly, the UCLA score improved from 17.29
± 2.44 to 32.65 ± 2.35 in group 1, and from 19.14 ± 3.13 to 31.42 ± 3.58 in group 2 (P < 0.001). And the ASES score improved form 36.26 ± 11.38 to 82.27 ± 10.69 in group 1 (P
< 0.001), and from 38.46 ± 11.45 to 80.57 ± 11.92 in group 2 (P < 0.001). The differences between the improvements in both UCLA and ASES scores in the two groups were insignificant (P > 0.001).
Patient satisfaction
In group 1, 26 out of 27 patients were satisfied with the treatment outcome and 1 patient was dissatisfied because of a slight unresolved pain. In group 2, 55 out of 65 patients were satisfied and 10 were dissatisfied.
The difference in the patients’ satisfaction levels was significant between the two groups (P < 0.001).
Range of motion
The active ROM for group 1 at preoperation and at final follow-up were as follows; mean preoperative and final follow-up forward elevation were 150.20 ± 6.67 and 172.00 ± 6.61, respectively, these values for abduction were 149.50 ± 6.71 and 165.10 ± 5.58, respectively, for external rotation during abduction were 65.50 ± 11.49 and 89.60 ± 13.15, respectively (P < 0.001), for internal rotation during abduction were 43.25 ± 11.24 and 67.18 ± 11.25, respectively (P < 0.001). The active ROM for group 2 at preoperation and at final follow-up were as follows;
mean preoperative and final follow-up forward elevation were 152.10 ± 7.43 and 170.00 ± 6.49, respectively, these values for abduction were 152.70 ± 7.48 and 162.60 ± 6.59, respectively, for external rotation during abduction were 66.40 ± 12.28 and 86.90 ± 12.26, respectively (P <
0.001), and for internal rotation during abduction were 44.15 ± 10.45 and 66.26 ± 10.78, respectively (P < 0.001).
The differences between the means of the ROM between groups 1 and 2 were not statistically significant (P > 0.001).
Anatomical results
Although none of the patients showed indications for MRI, MRI scans were taken of all patients between the 4th and 6th postoperative months. Those that gave intent of refusal of the radiological test were excluded from the data set. The MRI scans of each patient were analyzed and classified into the Sugaya classification system [2]. In the Sugaya classification, type I rotator cuff tendons shows a homogenous low-intensity signal in full-thickness tendons on MRI scans. Type II rotator cuff tendons show a partial high-intensity signal in full-thickness tendons.
Type III rotator cuff tendons do not show discontinuity in the signal intensity but have tendons with an incomplete thickness. Type IV rotator cuff tendons are like type III tendons but with slight discontinuity in signal intensity, and type V are with prominent discontinuity. Those classified with type IV and V rotator cuff tendons are considered to have a re-tear of the rotator cuffs. At the final follow-up, 27 patients from group 1 and 65 patients from group 2 were radiological examined, and the classification diagnosis was made by 2 radiologists specializing in musculoskeleton. We found that in group 1, 25 patients (92.59%) were negative for a re-tear and 2 patients (7.41%) were positive. In group 2, 53 patients (81.54%) were negative for a re-tear and 12 patients (18.46%) were positive). Group 1 had a significantly lower percentage of re-tears than group 2 (P < 0.001).
DISCUSSION
Arthroscopic suture technique is preferred over the open suture technique for the repair of rotator cuff tears, despite a higher incidence of re-tears associated with the former technique. The reason behind the higher incidence of re-tears in patients with arthroscopic sutures is thought to be because of the contact between the suture and the rotator cuff is weak [3–5]. An improved technique that can increase the binding between the suture and the tear of the rotator cuff [6] is needed. One suggestion that is being made is to make a stronger suture around the lesion of the attenuated tendon tissue [7,8].
The modified Mason-Allen (MA) is the gold standard technique for open sutures for its strong biomechanical strength compared to other types of suture techniques, but its demand for high technicality limits use in an arthroscopic setting [4,9]. For these reasons, the authors had previously recommended an arthroscopic approach of a modified ML suture technique to repair rotator cuffs [10]. However, the complex procedure of this modified ML suture technique meant it was an unrealistic option to many surgeons. Therefore, we devised a simplified procedure for the modified ML suture technique that could readily be performed in an arthroscopic setting.
Our simplified ML suture technique first, uses a suture hook to make two sutures around the rotator cuff tear, second, they are pulled out through the cannula of the anterosuperior portal, third, they are connected from the outside to make a horizontal mattress relay-shuttle, and lastly, two vertical loops are placed around the greater tuberosity bone, which completes the suture. The purpose of the transverse mattress loop is so that it acts as a checkrein to sustain the tear in the repair position.
Our logic behind this was that this method increases the resistance to the pull-out strength, which comes from the biomechanical properties of the suture. This increase in resistance would increase the strength of the binding power of the suture itself. We believed that this technique could decrease the incidence of re-tears, and indeed this was confirmed by the results of the follow-up MRI. We found that group 1 had a significantly lower incidence of re-tears than group 2 when MRI scans were taken between the 4th and 6th postoperative month. Therefore, we conclude that anatomical stability can be achieved by using our simplified method of modified ML suture technique.
The advantages of arthroscopic ML suture techniques
are that it is easier to perform in the arthroscopic setting than the modified MA technique, and that it is a simplified version than our initial design of the protocol. Further, a substantial fixative power can be achieved on the medial side of the suture than the simple suture technique.
When comparing with the double-row repair technique, our technique puts less tension on the medial side of the suture, is not associated with holes that are formed by retrograde passage, does not require knots, which means the procedure takes less time and it avoids knot collision, and finally uses less fixation screws that means costs are minimized. The disadvantages of the arthroscopic ML suture technique are that compared to the simple suture technique, it takes longer, no biomechanical studies yet exist, it cannot reconstruct the tendon foot print, and that strangulation may occur.
The limitations of this current study are that the number of study subjects was few in group 1, so we could not apply standard statistical analyses, and that the follow-up MRI was only taken between the 4th and 6th postoperative month, which meant that re-tears that may have occurred after 6 months were not accounted for. A different study had shown that after rotator cuff repairs in lambs, at 3 months postoperation, the MRI scans showed the repaired tendon had 52% signal intensity of that of a complete tendon, and at 6 months postoperation, this improved to 82% [4]. Their results suggest that to use MRI to discern restoration of the rotator cuff, the MRI scans should be performed at least 6 months after the operation [11], but in our study, MRI scans were taken at 4 months, which may not have given enough time for the tendon to heal. Further, although the current study was prospective, the number of patients between the two groups could not be controlled. Lastly, the effect of factors, such as tear shape and tendon intrasubstance quality, on re-tears could be looked at to improve this study.
We found that treating patients with small-sized or medium-sized rotator cuff tears using arthroscopic ML suture technique showed improved levels of pain and function, and at final follow-up the incidence of re-tear were significantly lower than when patients received simple sutures.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
1. Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg Br 2003;85:3-11.
2. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am 2007;89:953-60.
3. Cummins CA, Murrell GA. Mode of failure for rotator cuff repair with suture anchors identified at revision surgery. J Shoulder Elbow Surg 2003;12:128-33.
4. Gerber C, Schneeberger AG, Perren SM, Nyffeler RW. Experi- mental rotator cuff repair. A preliminary study. J Bone Joint Surg Am 1999;81:1281-90.
5. Ko SH, Cho SD, Gwak CY, Eo J, Yoo CH, Choe SW. Use of massive cuff stitch in arthroscopic repair of rotator cuff tears. J Korean Shoulder Elbow Soc 2006;9:181-8.
6. Ko SH, Cho SD, Park MS, et al. The use of bio suture anchor in the arthroscopic repair of medium sized full thickness rotator
cuff tear in sports injury. J Korean Sports Med 2005;23:180-5.
7. Ma CB, MacGillivray JD, Clabeaux J, Lee S, Otis JC. Biomechanical evaluation of arthroscopic rotator cuff stitches. J Bone Joint Surg Am 2004;86:1211-6.
8. Scheibel MT, Habermeyer P. A modified Mason-Allen technique for rotator cuff repair using suture anchors. Arthroscopy 2003;19:330-3.
9. Gerber C, Schneeberger AG, Beck M, Schlegel U. Mechanical strength of repairs of the rotator cuff. J Bone Joint Surg Br 1994;
76:371-80.
10. Ko SH, Rhee YG, Jeon HM, Lee CC. The usefulness of all arthro- scopic repair with biceps incorporation in massive sized fullthic- kness rotator cuff tears. J Korean Shoulder Elbow Soc 2007;10:
106-11.
11. Tae SK, Kim YS, Lee HM, Park PK. Patterns of retear after repair of the rotator cuff: MRI analysis of 109 cases. Clin Should Elbow 2012;15:16-24.