의
의
의학
학
학 석
석
석사
사
사학
학
학위
위
위 논
논
논문
문
문
P
P
Pr
r
re
e
eo
o
op
p
pe
e
er
ra
r
a
at
t
ti
i
iv
v
ve
e
e C
C
Ch
h
he
e
em
m
mo
o
or
r
ra
a
ad
d
di
i
io
ot
o
t
th
h
he
e
er
r
ra
a
ap
p
py
y
y
o
o
of
f
fL
L
Lo
o
oc
c
ca
a
al
l
ll
l
ly
y
y A
A
Ad
d
dv
v
va
a
an
n
nc
c
ce
e
ed
d
d R
R
Re
e
ec
c
ct
t
ta
a
al
l
l
C
C
Ca
a
an
n
nc
c
ce
e
er
r
r:
:
:P
P
Pr
r
re
e
el
l
li
i
im
m
mi
i
in
n
na
a
ar
r
ry
y
y R
R
Re
e
es
s
su
u
ul
l
lt
t
ts
s
s o
o
of
f
f
B
B
BI
I
ID
D
D F
F
Fr
r
ra
a
ac
c
ct
ti
t
i
io
o
on
n
na
at
a
t
ti
i
io
o
on
n
n
아
아
아 주
주
주 대
대
대 학
학
학 교
교
교 대
대
대 학
학
학 원
원
원
의
의
의 학
학
학 과
과
과
이
이
이 선
선
선 영
영
영
이
이
이선
선
선영
영
영의
의 의
의
의
의학
학
학 석
석
석사
사
사학
학
학위
위
위 논
논
논문
문
문을
을 인
을
인
인준
준
준함
함
함.
.
.
심
심
심사
사
사위
위
위원
원
원장
장
장
전
전
전 미
미
미 선
선
선
인
인
인
심
심
심 사
사
사 위
위
위 원
원
원
오
오
오 영
영
영 택
택
택
인
인
인
심
심
심 사
사
사 위
위
위 원
원
원
강
강
강 승
승
승 희
희
희
인
인
인
아
아
아 주
주
주 대
대
대 학
학
학 교
교
교 대
대
대 학
학
학 원
원
원
2
2
20
0
00
0
08
8
8년
년
년 6
6
6월
월
월 2
2
23
3
3일
일
일
P
P
Pr
r
re
e
eo
o
op
p
pe
e
er
r
ra
a
at
t
ti
i
iv
v
ve
e
e C
C
Ch
h
he
e
em
m
mo
o
or
r
ra
a
ad
d
di
i
io
o
ot
t
th
h
he
e
er
r
ra
a
ap
p
py
y o
y
o
of
f
fL
L
Lo
o
oc
c
ca
a
al
l
ll
l
ly
y
y
A
A
Ad
d
dv
v
va
a
an
n
nc
c
ce
e
ed
d
d R
R
Re
e
ec
c
ct
t
ta
a
al
l
lC
C
Ca
a
an
n
nc
c
ce
e
er
r
r:
:
:P
P
Pr
r
re
e
el
l
li
i
im
m
mi
i
in
n
na
a
ar
r
ry
y
y R
R
Re
e
es
s
su
u
ul
l
lt
t
ts
s
s
o
o
of
f
fB
B
BI
I
ID
D
D F
F
Fr
r
ra
a
ac
c
ct
t
ti
i
io
o
on
n
na
at
a
t
ti
i
io
o
on
n
n
by
LeeSunYoung
A Di
ssertati
onSubmi
ttedtoTheGraduateSchoolofAj
ouUni
versi
ty
i
nParti
alFul
fi
l
l
mentoftheRequi
rementsfortheDegreeof
MASTEROFMEDICALSCIENCES
Supervi
sedby
Mi
sonChun,M.
D.
,Ph.
D.
D
D
De
e
ep
p
pa
a
ar
r
rt
t
tm
m
me
e
en
n
nt
t
to
o
of
f
fM
M
Me
e
ed
d
di
i
ic
c
ca
a
al
l
lS
S
Sc
c
ci
i
ie
e
en
n
nc
c
ce
e
es
s
s
T
T
Th
h
he
e
eG
G
Gr
r
ra
a
ad
d
du
u
ua
a
at
t
te
e
eS
S
Sc
c
ch
h
ho
o
oo
ol
o
l
l,
,
,A
A
Aj
j
jo
o
ou
u
uU
U
Un
ni
n
i
iv
v
ve
e
er
rs
r
s
si
i
it
t
ty
y
y
A
A
Au
u
ug
g
gu
u
us
s
st
t
t,
,
,2
2
20
0
00
0
08
8
8
- ABSTRACT -
Preoperative Chemoradiotherapy of Locally Advanced Rectal
Cancer: Preliminary Results of BID Fractionation
Introduction: Preoperative chemoradiotherapy is an effective modality for patients with
locally advanced rectal cancer. This study was designed to evaluate the efficacy, tolerance,
and toxicity of preoperative chemoradiotherapy (CRT) in patients with locally advanced
rectal cancer, using BID fractionation.
Patients and methods: Between January 2001 and November 2007, 35 patients were
treated with preoperative CRT and then received operation for locally advanced rectal cancer.
Three cycles of chemotherapy were delivered with 5-FU based regimen, mainly FOLFIRI
(n=25), every 3 weeks. Radiation treatment scheme was 1.5 Gy (n=31) or 1.6 Gy (n=4) of
radiation twice a day, and 1st course of radiotherapy of 21-24 Gy was delivered concurrently
with 1st cycle of chemotherapy followed by 10-12 days rest period and 2nd course of
radiotherapy of 21-24Gy was delivered concurrently with 2nd cycle of chemotherapy.
Results: The median follow up period was 19 months (5-36 months). All were T3
(n=24) or T4 (n=11) and the largest diameter of tumor mass was median 5cm (2.5-14cm).
Overall downstaging rate was 71%. Pathologic complete response (pCR) rate was 11% (n=4),
near CR rate (microscopically focal residual tumor, and less than 10% of viable cells) was
23% (n=8), and partial response rate was 60% (n=21). Upon operation, two patients were
found to have unresectable tumor. Sphincter-preserving procedure was performed in 43% of
Only 8 patients (23%) showed severe acute toxicity (grade 3 neutropenia in 4 patients,
grade 3 and 4 perineal skin reaction in each one patient, and grade 3 diarrhea in 1 patient).
Seven patients (20%) had treatment interrupted (1-8 days) because of following reasons; 3
for perineal skin reaction, 3 for chemotherapy-related problems, and 1 for anal abscess
control problems. Late toxicity was observed in 2 patients; perineal open wound in one
patients and rectovaginal fistula in the one patient.
Conclusion: Preoperative BID-fractionation CRT for locally advanced rectal cancer
achieved 34% of pCR or near CR rate. And this treatment protocol was feasible as a
preoperative treatment without compromising tumor response and with better tolerance in
locally advanced rectal cancer.
K ey wor ds: r ect al can cer, ne oadj uvant , conc ur r ent che mor adi ot her apy, B ID
차
차
차
차 례
례
례
례
ABSTRACT ··· ⅰ TABLE OF CONTENTS ··· ⅲ LIST OF FIGURES ··· ⅴ LIST OF TABLES ··· ⅵ . INTRODUCTION Ⅰ ··· 1. MATERIALS AND METHODS Ⅱ ··· 3 A. PATIENTS ··· 3 B. TREATMENT ··· 4 1. PREOPERATIVE CHEMORADIOTHERAPY ··· 4 2. SURGERY··· 7 3. POSTOPERATIVE CHEMOTHERAPY··· 7
C. RESPONSE CLASSIFICATION AND TOXICITY CRITERIA ··· 7
D. PATHOLOGIC EVALUATION ··· 8 E. FOLLOW UP ··· 9 . RE Ⅲ SULTS ··· 10 A. SURGERY ··· 10 B. PATHOLOGIC RESPONSE ··· 12
C. TOXICITY AND TREATMENT INTERRUPTION ··· 14
. DISCUSSION Ⅳ ··· 18
. CONCLUSION Ⅴ ··· 26
LIST OF FIGURES
Fig. 1. The schedule of concurrent chemoradiation therapy··· 5
LIST OF TABLES
Table 1. Characteristics of patients and tumors ··· 11
Table 2. The pathologic response ··· 13
Table 3. Acute toxicities by RTOG criteria··· 15
I. INTRODUCTION
T he t her apeut i c choi c e of r ect al cancer r e mai ns t o be surger y. T he
out co me of surger y i s excel l ent i n pat i ent s w i t h ear l y st a ge r ect al c ancer,
howe ver, t he out co me of surger y al one i s p oor wi t h l on ger sur vi val r at e
of onl y 40 -50% , and l ocal f ai l ur e r at e of 25 % i n hi gh -r i s k gr oup . In hi gh
r i sk gr o up, post ope r at i ve adj uva nt r adi ot her apy wi t h or wi t hout
che mot her ap y coul d r educe l ocal f ai l ur e r a t es b y 10 -1 5% ( Rosen et al ,
2007) . Mor eo ver, t he i nt r oduct i on of t ot al mesor ect al exci si on ( T ME) i n
t he mana ge ment of r ec t al cancer has yi el ded t he l ocal f ai l ur e r at e o f l ess
t han 10% ( K api t ei j n et al , 2001) .
Recent l y, pr eoper at i ve r adi ot her ap y wi t h che mot her ap y has been
pr ef er r ed f or t he ma nage ment of l ocal l y ad vanced r ect al ca ncer t o
pr eser ve sphi nct er f u nct i on and i mpr o ve l ocal cont r ol and r ecur r ence
-f r ee sur vi val . And ma ny st udi es on t he pr e oper at i ve c he mor adi ot her apy
( CRT ) ha ve bee n go i ng on wi t h no vel a gent s. Var i ous sche m es of
pr eoper at i ve r adi ot her apy ha ve been used. M ost co mmon sche me c onsi st s
of conve nt i onal f r act i onat i on of f i ve t i mes per wee k, dai l y r adi at i on. In
addi t i on, shor t cour se or t wi ce dai l y f r act i o nat ed r adi ot her ap y ha s been
used i n so me . ( Couc ke et al , 199 5; Mohi uddi n et al , 20 06; Tsuj i naka et al ,
2008)
l at e t oxi ci t i es. We used B ID -f r act i onat i on pr ot ocol conc ur r ent l y wi t h
each cycl e of che mot her apy a nd enhanced t he r adi at i on dose wh i l e on
che mot her ap y.
Pr el i mi nar y r esul t s we r e anal yzed wi t h r e gar ds t o pat hol o gi c r espo nse,
t ol er ance, and t oxi ci t y i n l ocal l y ad va nced r ect al cancer pat i ent s who
II. MATERIALS AND METHODS
A. Pat i ent s
We anal yzed pat i ent s have hi st ol o gi cal l y co nf i r me d aden ocar ci no ma of
t he r ect u m, wi t hout e vi dence of di st ant met a st asi s.
Bet ween 2001 and 2 007, 2 58 pat i ent s wi t h pr i mar y r ect al ca ncer
r ecei ved r adi at i on t her apy wi t h/ wi t hout concur r ent che mot her apy.
Four t y-o ne pat i ent s w er e t r eat ed f or r ecur r ent r ect al cancer af t er surger y
and t he r e mai ni n g 217 pat i ent s f or newl y di a gn osed r ect al ca ncer. A mo n g
217 pat i ent s, 63 pat i en t s under went pr eo per at i ve r adi ot her ap y.
Of 63 pat i ent s t r eat ed wi t h pr eoper at i ve r adi ot her apy, 20 pat i ent s wer e
excl uded: 5 pat i ent s wer e r ef er r ed t o anot her hospi t al s dur i n g or af t er
co mpl et i on of che mor adi ot her apy ( C RT ) , 8 pat i ent s wer e l ost t o f ol l ow
-up or r ef used surger y af t er co mpl et i on of C RT, 2 pat i ent s ha d i nc o mpl et e
t r eat ment wi t h po or gener al condi t i on ( pne u moni a i n one and C OPD i n
t he ot her ) , 2 pat i ent s had si mul t aneous l i ver met ast asi s, 1 pat i e nt was
t echni cal l y i no per abl e because of hi p j oi nt r epl ace ment s urger y f or
t uber cul oses ar t hr i t i s, 1 pat i ent di ed f r o m neut r openi a r el at ed wi t h
che mot her ap y af t er 24 G y, an d 1 pat i ent devel ope d di st ant f ai l ur e
i mmedi at el y af t er C RT. Tot al 43 pat i ent s wi t h l ocal l y ad vanced r ect al
cancer ( pr et r eat ment cl i ni cal st age T 3 -4 Na nyM0) , i ncl udi n g cl i ni cal l y
wi t h subseque nt cur at i ve su rger y. Of 4 3 pa t i ent s, 35 pat i ent s r e cei ved
r adi ot her apy wi t h t wi ce -dai l y ( B ID ) r e gi me n and 8 pat i ent s wi t h once a
day ( Q D) r e gi men. We anal yzed t he 35 pat i ent s who wer e t r eat e d wi t h
B ID r e gi men.
Al t hou gh not t he sa me f or al l pat i ent s, t he pr et r eat ment e val u at i on
i ncl uded co mpl et e bl ood count , che mi cal t est wi t h r enal an d l i ver
f unct i on, car ci noe mbr yo ni c ant i ge n ( C EA) l e vel , di gi t al r ect al
exa mi nat i on, col onosc op y wi t h/ wi t hout bar i u m e ne ma, chest r adi o gr aph y,
and co mput ed t o mo gr a ph y ( CT ) scan of abd o men and pel vi s wi t h/ w i t hout
endoscopi c ul t r asoun d. Pr et r eat ment cl i ni cal st age was car r i e d out
accor di ng t o T NM st a ge ( AJ CC/ U IC C, 2002 )
B. Tr eat ment
1. Pr eoper at i ve Che mo r adi ot her apy
T he t r eat ment sche ma i s shown i n Fi g. 1.
Radi at i on vol u me enc o mpassed t he r ect al mass t he i n vol ve d pe l vi c
l ymph -node( s) wi t h a margi n of 2 -3c m i n al l di r ect i on. T he i nf er i or
bor der excl uded t he pe r i neal ski n whe n f easi bl e, on t he except i ona l cases
wher e t he t u mor e xt ended cl ose t o t he anal verge. T he post er i or bor der
of l at er al f i el ds i ncl uded t he sacr u m and co c cyx .
Radi at i on t her apy of B ID -f r act i onat i on r egi me n wi t h spl i t cour se i s
Fr act i on si ze; 1.5 G y or 1.6 G y, Tot al dose; 45 G y ( 39~57.6 G y)
2nd cycle of CTx 1st cycle of CTx
Planned rest (10-12 day)
1st course treatment 2nd course treatment
Radiotherapy
Chemotherapy Day
Fig. 1. The schedule of concurrent chemoradiation therapy. Radiation therapy was
planned to start concurrently with 1st cycle of chemotherapy and delivered as
BID-fractionation regimen with split course. The fraction size of radiation therapy was 1.5 Gy
(n=31) or 1.6 Gy (n=4). After the radiotherapy of 7 or 8 days (1st course treatment, 21 Gy ~
24 Gy), the planned rest period was median 11 days (range, 6-18 days). After then, another
7-8 days of radiotherapy (2nd course treatment) was started with 2nd cycle of chemotherapy and
total dose was median 45 Gy. After the completion of radiotherapy, additional cycle of
chemotherapy was delivered according to surgeons’ judgment, based on tumor respectability
G y ( n=4) , 5 da ys per wee k f or 7 -8 d a ys ( 1s t cour se t r eat ment ) , f o l l owed
by an ot her 7 -8 da ys ( 2n d cour se t r eat ment ) wi t h t he sa me sche me . Most
co mmonl y used t ot al dose was 45 G y i n 14 pat i ent s ( l ess t han 45 G y i n
11, bet ween 40 G y an d 50 G y i n 10 , and mo r e t han 50 G y i n 7) . B et ween
1s t an d 2n d cour ses t r e at me nt , t he pl anned r e st per i od w as medi an 11 da ys
( 6 -18 da ys) . O ver al l t r eat me nt t i me, i ncl udi ng wee ke nd an d r est per i od,
was me di an 32 da ys ( 2 7 -41 da ys) .
Radi at i on t her ap y w a s del i ver ed wi t h 1 0 - MV or 15 -MV phot on s and
t hr ough t hr ee -f i el d ( PA/ bi l at er al ) or f our-f i el d ( A P/ PA / bi l at er al)
t echni que. Pat i ent s w er e t r eat ed i n t he pr one posi t i on usi ng bel l y boar d
devi ce t o excl ude t he s mal l bo wel o ut of r adi at i on t her ap y f i el d,
whene ver possi bl e. Bef or e 2n d cour se t r eat me nt , al l pat i ent s wer e
eval uat ed wi t h t he C T scan of abdo men a nd pel vi s, and t r eat e d wi t h
r educed f i el d d ependi ng on t he r educt i on of t u mor si ze. At t hi s t i me,
t hr ee -di me nsi onal co nf or mal r adi ot her ap y pl anni ng was ut i l i zed,
whene ver p ossi bl e.
Al l pat i ent s r ecei ved 5 -F U based c he mot her apy. T he 1s t c ycl e of
che mot her ap y was st a r t ed wi t h t he 1s t c ou r se of r adi ot her ap y a nd 2n d
cycl e of che mot her ap y wi t h 2n d c our se of r adi ot her apy. T he maj or i t y of
pat i ent s r ecei ve d 3 c ycl es of c he mot her ap y bef or e surger y, an d so me
r ecei ved addi t i onal che mot her ap y accor di ng t o cl i ni ci an’s j udgment
ot her r egi men s i ncl uded FPL ( n=3) , FL ( n= 2) , and or al che mot he r apeut i c
agent ( ca peci t abi ne i n 3 and do xi f l ur i di ne i n 1) .
T he FOLF IR I r e gi me n was ad mi ni st er ed a s f ol l ows; i r r i not ecan 180
mg/ m2 as a 90 mi nut es i nf usi on on da y 1 , l euco vor i n ( LV ) 200 mg/ m2
dur i ng i r r i not ecan f o l l owed b y 5 -F U bol u s 400 mg/ m2 and 22 hour s
cont i nuous i nf usi on of 600 mg/ m2 o n da y 1 a nd 2 e ver y 2 wee ks. T he FL
r egi men consi st ed of 5 -F U 400 mg/ m2 i . v. bol us and LV 20 mg/ m2 i . v.
bol us f or 4 da ys.
2. Surger y
Surger y was pl an ned 3 4 wee ks af t er t h e co mpl et i on of che mo
-r adi ot he-r apy. Tot al me so-r ect al exci si on ( T ME) was -r eco m mended.
3. Post oper at i ve ch e mot her apy
Al l pat i ent s r ecei ve d 5 -F U base d post oper at i ve che mot her apy,
i r r espect i ve of pat hol ogi c r esp onse. T he maj or it y of pat i ent s r ec ei ved 3
cycl es of F OLF IR I r e gi men ( n=2 8) and ot h er s r ecei ved FPL ( n= 1) , FP
( n=1) , and or al che mo t her apeut i c age nt ( dox i f l ur i di ne i n 3 and t e gaf ur i n
1) .
C. Res ponse cl assi f i ca t i on and t oxi ci t y cr i t er i a
car ci no ma on pat hol o gi c s peci men. It was def i ned as near co mpl et e
r esponse ( near p CR) when t her e was on l y mi cr oscopi cal l y r esi dual
di sease wi t h l ess t han 10% of vi abl e cancer ( Roof et al , 2006) .
Downst a gi n g was doc u ment ed b y a decr eas e of p ost -C RT pat hol ogi c
st age co mpar ed wi t h pr et r eat ment cl i ni cal st age. Tdo wnst a gi n g and N
-downst a gi n g wer e r es pect i vel y e val uat ed a nd o ver al l dow nst a gi ng was
docu ment ed b y mor e t han one of T or N -dow nst agi n g.
Acut e t oxi ci t y was gr aded i n accor danc e wi t h Acut e Radi a t i on
Mor bi di t y Sc or i n g Cr i t er i a pr oposed b y R adi at i on T her apy On col ogy
Gr oup ( RTO G) and l a t e t oxi ci t y wi t h Lat e Radi at i on Mor bi di t y Scor i n g
Sche ma pr oposed b y RTOG/ EO RT C.
D. Pat h ol o gi c e val uat i on
T he pat hol o gi c st a ge f or each t u mor was r ecor ded acc or di n g t o 6t h
edi t i on of AJ CC/ U IC C T NM cl assi f i cat i on ( Sobi n et al , 20 02) . T he R
st age was r ecor ded as f ol l ows: mi cr oscopi ca l l y f r ee ma rgi n was r e cor ded
as R0 , mi cr oscopi cal l y i n vol ved margi n as R1, and macr osco pi c r esi dual
di sease or no r esect i on as R2. Pat hol o gi c speci me ns wer e gr ossl y
r evi ewe d i n t er ms of gener al appear ance of speci men, t he gr os s shape
( e.i . ul cer at i on or f ungat i n g) and si ze of pr i mar y t u mo r, and t he d i st ance
bet ween r esect i on margi ns and pr i mar y t u mor. In det ai l , hi st opat hol ogi c
pr esence or absence o f l ymphat i c and per i n eur al i n vasi on, t he nu mber of
l ymph node exa mi ne d , t he n u mber of l ymp h node i n vol ved, and ot her
abnor mal i t i es wer e e val uat ed b y pat hol o gi st .
E. Fol l o w -up
Pat i ent s wer e cl i ni cal l y wee kl y assessed dur i ng t r eat ment f or t he
co mpl i ance, ge ner al c ondi t i on, and t oxi ci t y. Co mpl et e bl ood c ou nt and
bod y wei ght wer e al so chec ked. Af t er t h e co mpl et i on of t r ea t me nt ,
pat i ent s wer e assessed ever y 3 mont hs f or t h e f i r st 2 year s, e ver y 6 year s
f or t he next 2 year s and annual l y t her eaf t er, wi t h CT scan of abdo men
and pel vi s, chest r adi ogr ap h y, col onosc op y, and l ab st udy ( C EA ser u m
III. RESULTS
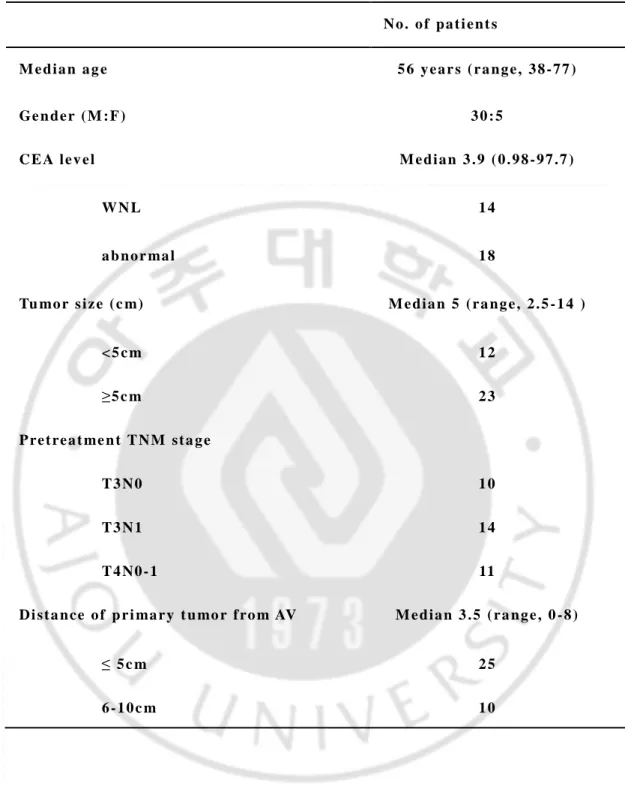
Char act er i st i cs of pat i ent s and t u mor s ar e shown i n Tabl e 1. Medi an
age was 56 year s ( r a nge , 38 -7 7 year s) . T he pr et r eat ment cl i ni ca l st age
was T 3 i n 24 pat i ent s, T 4 i n 11 pat i ent s ( 31% ) , and posi t i ve l ymp h -no de
i n 23 pat i ent s ( 66% ) . T he maj or i t y of t u mor s wer e l ocat ed i n di st al
r ect u m. T he l ower ma rgi n of pr i mar y t u mor was wi t hi n medi an 3c m f r o m
anal ve rge ( 25 pat i en t s wi t hi n 5 c m an d a l l wi t hi n 8 c m) . T he l argest
di a met er of pr i mar y t u mor was me di an 5c m ( r ange , 2.5 -1 4 c m) .
T he f ol l ow up per i od was me di an 19 mont hs ( r ange , 5 -39 mont hs) .
A. S urger y
T he me di an per i od f r o m t he co mpl et i on of r adi ot her apy t o surger y was
41 da ys an d f r o m t he c o mpl et i on of ch e mot h er apy was 3 2 da ys .
Surger y was per f or me d i n al l pat i ent s. Two pat i ent s wer e consi der ed
unr esect abl e at t he t i me of surger y af t er C RT and under went op en and
cl osur e ( O &C) wi t h p al l i at i ve i l eost o my be cause of l at er al ext en si on t o
t he pel vi c si de wal l a n d bl adder i n vasi on. T h i r t y-t hr ee pat i ent s und er went
cur at i ve surger y wi t h abdo mi nop er i neal r ese ct i on ( AP R) i n 16 pat i ent s,
l ow ant er i or r esect i on ( LAR) i n 10 pat i ent s, and Har t mann’s oper at i on i n
7 p a t i e n t s . T h e s p h i n c t e r p r e s e r v a t i o n w a s p o s s i b l e i n 1 7 o f a l l 3 5
Tabl e 1. Char act eri st i cs of pat i ent and t u m or. N o . o f p a t i e n t s M e d i a n a g e 5 6 y e a r s ( r a n g e , 3 8 - 7 7 ) Ge n d e r ( M : F ) 3 0 : 5 C E A l e v e l M e d i a n 3 . 9 ( 0 . 9 8 - 9 7 . 7 ) W N L 1 4 a b n o r ma l 1 8 Tu mo r s i z e ( c m) M e d i a n 5 ( r a n g e , 2 . 5 - 1 4 ) < 5 c m 1 2 ≥ 5 c m 2 3 P re t re a t me n t T N M s t a g e T 3 N 0 1 0 T 3 N 1 1 4 T 4 N 0 - 1 11 D i s t a n c e o f p r i ma r y t u mo r f ro m AV M e d i a n 3 . 5 ( r a n g e , 0 - 8 ) ≤ 5 c m 2 5 6 - 1 0 c m 1 0
wi t hout pr eoper at i ve CRT.
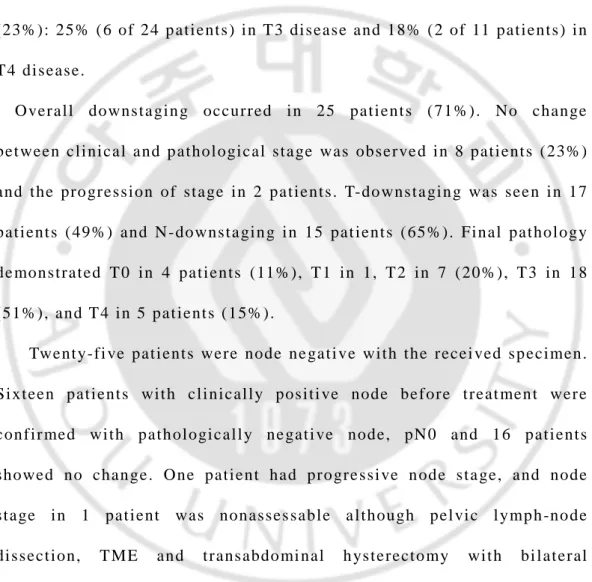
B. Pat hol o gi c r espons e
T her e wer e 4 pat i ent s who achi e ved pC R, a ccount i n g f or pC R r at e of
11% f or al l 35 pat i ent s. T he pCR r at e was 25% ( 6 of 24 pat i ent s ) i n T 3
di sease and 0% i n T 4 di sease. Near p CR was obser ve d i n 8 pat i ent s
( 23% ) : 25% ( 6 of 24 p at i ent s) i n T 3 di sease and 18% ( 2 of 11 pat i ent s) i n
T 4 di sease.
O ver al l downst a gi n g occur r ed i n 25 pat i ent s ( 71% ) . No change
bet ween cl i ni cal and p at hol ogi cal st a ge was obser ve d i n 8 pat i ent s ( 23%)
and t he pr o gr essi on of st age i n 2 pat i ent s. T-do wnst a gi n g was see n i n 17
pat i ent s ( 49% ) and N - downst a gi n g i n 15 pat i ent s ( 65% ) . Fi nal pat hol ogy
de monst r at ed T 0 i n 4 pat i ent s ( 11% ) , T 1 i n 1, T 2 i n 7 ( 20% ) , T 3 i n 18
( 51% ) , and T 4 i n 5 pat i ent s ( 15% ) .
Twent y-f i ve pat i ent s wer e node ne gat i ve wi t h t he r ecei ved sp eci men.
Si xt een pat i ent s wi t h cl i ni cal l y posi t i ve node bef or e t r eat men t wer e
conf i r med wi t h pat h ol ogi cal l y ne gat i ve node, pN 0 and 16 pat i ent s
showed no chan ge. O ne pat i ent had pr o gr e ssi ve n ode st a ge, and node
st age i n 1 pat i ent was nonasses sabl e a l t hough pel vi c l ymp h -no de
di ssect i on, T ME an d t r ansabdo mi nal h yst er ect o my wi t h bi l at er al
sal phi ngo ophor ect o my ( TAH c BS O) wer e per f or med due t o vagi nal
i nvasi on of pr i mar y t u mor.
Tabl e 2. The pat h ol og i c response .
No.of pat i ent s ( %) Com pl et e rem i ssi on ( pCR) 4 11 Near c om pl et e rem i ssi on ( near pC R) 8 23 P at hol ogi c T- st age
y pT0 4 11 y pT1 1 3 y pT2 7 20 y pT3 18 51 y pT4 5 15 P at hol ogi c N- st age
y pN0 25 71 y pN1 3 9 y pN2 3 18 y pN3 1 3 y pN x 1 3 Resect i on m argi n st a t us R0 29 83 R1 4 11 R2 2 6
In 33 pat i ent s who under went t u mor r esect i on, no pat i ent had no R2
r esect i on and 4 pat i en t s ( 11% ) had an R1 r esect i on wi t h cl osed r e sect i on
margi n at f i nal pat h ol ogy. Of t he 4 pat i ent s, 2 had posi t i ve deep
r esect i on margi n a nd 2 wi t h ci r cu mf er en t i al r esect i on margi n . Two
pat i ent s each i n T 3 an d T 4 di sease had a n R 1 r esect i on, r espect i ve l y.
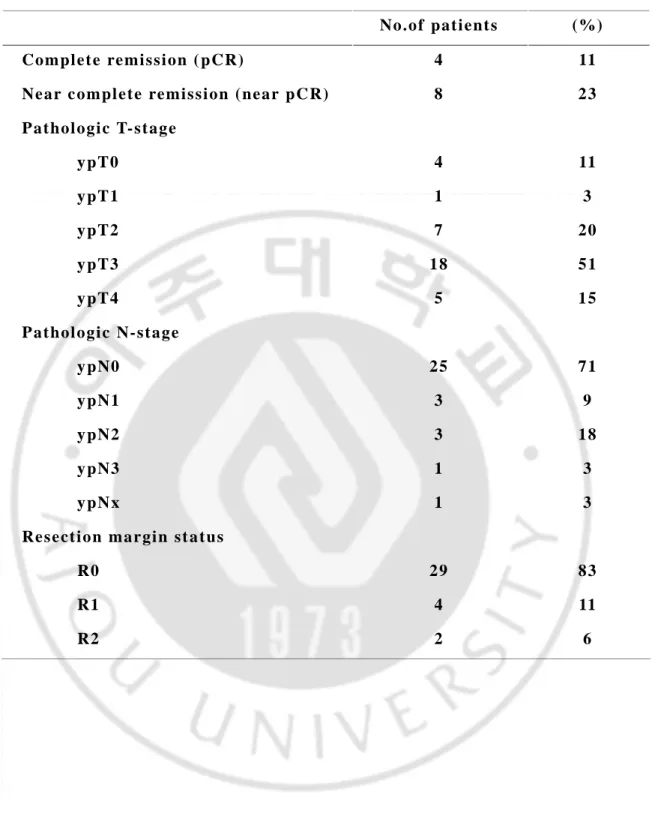
C. Toxi ci t y a nd t r eat ment i nt er r upt i on
Acut e t oxi ci t i es dur i n g C RT ar e s u mmar i zed i n Tabl e 3. O ver al l se ver e
( gr ade 3 or hi gh er ) t oxi ci t y wer e 20% . Neut r openi a was t h e most
co mmon se ver e t o xi ci t y; 4 pat i ent s ( 11% ) exper i enced gr ade 3
neut r openi a. No gr ade 4 he mat ol o gi c t oxi ci t y oc cur r ed. Gr ade 2 p er i neal
ski n r eact i on occur r ed i n 5 pat i ent s ( 14% ) a nd gr ade 3 an d 4 i n ea ch one.
Gr ade 2 acut e di ar r he a occur r ed i n 6 pat i en t s and gr ade 3 i n 1 pa t i ent s.
Gr ade 2 c yst i t i s occu r r ed i n 2 pat i ent s, a nd no gr ade 3 or 4 cyst i t i s
occur r ed.
T he causes and dur at i ons of i nt er r upt i on ar e show n i n Tabl e 4. S even
pat i ent s r equi r ed t he i nt er r upt i on of r adi at i o n t her ap y due t o se ver e acut e
t oxi ci t y: per i neal ski n r eact i on wi t h/ wi t hout per si st ent pr oct i t i s ( 3
pat i ent s) , che mot her a py-r el at ed pr obl e ms ( 3 pat i ent s) , and unco nt r ol l ed
anal abscess ( 1 pat i ent ) .
Gr ade
2 3 4 5
He mat ol o gi c
neut r openi a 4
t hr o mboc yt ope ni a 1 0
Lower gast r oi nt est i nal
di ar r hea 6 1
Geni t our i nar y
c yst i t i s 2
Ski n 5 1 1
n o d e a t h
Cause n Da ys
Per i neal ski n r eact i on 2 6/ 1
Per i neal ski n r eact i on + per si st ent pr oct i t i s 1 3
Che mot her a p y-r el at ed pr obl e ms 3 8/ 1/ 3
Anal abscess c ont r ol p r obl e m 1 7
occur r ed wi t hi n 30 d ays af t er t he i ni t i al oper at i on and al so unt i l l ast
f ol l ow up.
Lat e t oxi ci t i es wer e devel op ed i n 2 pat i e nt s: open per i neal wo und
and f i st ul a i n one each pat i ent . No pat i ent s devel ope d sof t t i ssue
necr osi s, ul cer at i on, o r bon y f r act ur e.
Post oper at i ve mor t al i t y was 3 % ( 1 pat i en t ) . One di ed f r o m ac ut e
myocar di ac i nf ar ct i on on t he next day af t er cur at i ve surger y: he had
pr i mar y t u mor wi t hi n 4 c m f r o m t he anal verge a nd was t r eat ed wi t h
r adi ot her apy ( 45 G y/ 3 0 f r act i ons) and che m ot her apy ( F Ol F IR I r e gi men,
3cycl e) , f ol l owed b y l ow ant er i or r esect i on.
Dur i n g t he past t hr ee decades, t he r e mar kab l e ad vance has been made
i n t he mana ge ment of r ect al cancer. Based on t he r esul t s of l arge
pr ospect i ve r ando mi zed st udi es ( Gast r oi nt est i nal Tumor St ud y Gr oup;
1985, Fi sher et al , 1988; K r oo k et al , 1991; Wol mar k et al , 2000;
Col or ect al Cancer C ol l abor at i ve Gr ou p, 2001) , t he co mbi ned use of
r adi ot her apy a nd che mot her ap y has been r eco mmended as an a dj uvant
t r eat ment beca use i t i s mor e eff ect i ve i n t he r educt i on of l ocal
r ecur r ence and a gr eat er pot ent i al f o r i mpr o ved sur vi val t han
post oper at i ve r a di ot her apy al one ( N IH conse nsus conf er ence, 1990 ) .
In addi t i on, r ece n t l y, pr eoper at i ve r adi at i on t her ap y wi t h
che mot her ap y has r e cent l y been a pr ef e r r ed appr oach f or l ocal l y
adva nced r ect al ca nce r i n man y i nst i t ut es and t r i al s. Se ver al po t ent i al
adva nt a ges of pr eop er at i ve r adi ot her ap y have been i dent i f i ed: 1)
downsi zi n g an d do w nst agi n g eff ect s, con sequent l y r esul t i ng i n t he
i mpr o ve ment of p CR, cl ear r esect i on margi n ( R0) , and l ocal cont r ol , 2)
t he possi bi l i t y of sphi nct er pr eser vi n g surge r y i n di st al r ect al can cer, 3)
mor e r adi osensi t i ve, pr obabl y due t o hi gh er oxygen t ensi on pr i or t o
surgi cal co mpr o mi se o f t he r e gi onal bl o od vessel s, 4) l ess ac ut e a nd l at e
t oxi ci t y r at es due t o mor e mobi l e of s mal l bowel and l ess l i kel y
i ncl usi on of s mal l bo wel wi t hi n t he r adi at i on f i el d pr i or t o surge r y, and
of t u mor cel l s bef or e surger y. Abo ve ment i oned, i deal r at i onal e s ma ke
pr eoper at i ve ap pr oach mor e pop ul ar, and cl i ni cal r esul t s al so suppor t and
accel er at e t he use of pr eoper at i ve a ppr oach f or l ocal l y a d vanced r ect al
cancer.
Swedi sh r ect al canc er t r i al made go od f i r st st ep f or war d f or
pr eoper at i ve r adi ot her apy of r esect abl e r ec t al cancer ( Mi nsky, 1997) .
Swedi sh r ect al cancer t r i al co mpar ed sh or t -t er m pr eoper at i ve r adi at i on
t her apy ( 25 G y del i ver ed i n f i ve f r act i ons i n one wee k) f ol l ow ed by
surger y wi t hi n 1 wee k ( n=553) wi t h surger y al one ( n=557) i n r esect abl e
r ect al cancer pat i ent s ( Swe di sh r ect al ca n cer t r i al , 1997) . Af t e r f i ve
year s of f ol l o w -up, t h e r at e of l ocal r ecur r ence was 11 % i n co mbi ned
r adi ot her apy gr oup a nd 27% i n surger y al one gr oup ( P< 0.00 1) and
over al l f i ve -year sur vi val r at e was 58 % and 48% ( P<0.0 04) , r espec t i vel y.
Because of shor t o ve r al l t r eat ment t i me a nd t he opt i on of i mmedi at e
surger y, t hi s concept has now bee n used f r equent l y i n pat i en t s wi t h
oper abl e car ci no ma of t he r ect u m t hr ou gh out Eur ope . Ne ver t hel ess,
maj or r adi o- a nd t u mor bi ol ogi cal shor t co mi n gs a mon g ot her s a r e shor t
i nt er val bet ween r adi at i on t her ap y an d su rge r y, w hi ch doe s not al l ow f or
si gni f i cant t u mor shr i nka ge a nd sphi nct er pr eser vat i on i n l o w l yi n g
t u mor s, and t he hi gh si ngl e dose whi ch ma y i nd uce mor e acut e a nd l at e
t oxi ci t y has al so pr o m pt ed cr i t i ci sm ( Mi ns ky, 1997) .
showed i mpr o ved l oc al cont r ol and sphi nc t er-pr eser vat i on and r educed
t oxi ci t y i n pr eo per at i ve C RT gr oup , co mpa r ed wi t h post oper at i ve C RT
gr ou p ( Sa uer et al , 2 004) . Af t er t hi s enco ur agi n g r esul t , pr eop er at i ve
CRT has been est abl i shed as t he st an dar d t r eat ment i n r esect abl e, l ocal l y
adva nced r ect al cance r. And man y i n vest i gat i ons on pr eoper at i ve C RT
have bee n done and a r e st i l l ongoi n g wi t h no vel age nt s. T her e h as been
used var i ous sche mes of pr eoper at i ve r adi ot her apy wi t h che mot her apy
have been use d i n eac h i nst i t ut es and pol i t i es. Gener al l y, t her e ar e shor t
cour se sche me ( 25G y i n 5 f r act i ons) a nd con vent i onal sch e me i n
r adi at i on t her apy. Pr eoper at i ve cl i ni cal t r i al s based on T ME have
r ecent l y bee n r epor t ed .
A mo n g shor t co ur se sche mes, one i s t he abo ve me nt i oned S we di sh
r ect al cancer t r i al an d t he ot her i s D ut ch t r i al ( K api t eij n et al , 2001) .
Di ff er i ng f r o m t he S wedi sh t r i al , T ME i n Dut ch t r i al was st and ar di zed
and al l under went T ME. Pat i ent s wi t h r e sect abl e r ect al cancer wer e
r ando ml y assi gned ei t her t o pr eoper at i ve r a di ot her apy wi t h T ME ( n=924)
or T ME al one ( n=93 7) . T he o ver al l sur vi val r at e at t wo year s was si mi l ar
i n t wo gr oups ( 82% vs 8 1.8% , p=0.84) , wher eas t he r at e o f l ocal
r ecur r ence at t wo yea r s was 2.4% i n co mbi ned gr oup and 8.2% i n T ME
al one ( P<0.001) . Pat i ent s i n co mbi ned gr o up l ost sl i ght l y mor e bl ood
dur i ng o per at i on ( p<0. 001) and had mor e pe r i neal compl i cat i on ( p=0.05)
T he Eur opean Organi zat i on f or Resear ch and Tr eat ment of Ca ncer
( EOR CT ) 22921 t r i al ( Bosset et al , 2006) c o mpar ed pr eoper at i ve RT ( 45
G y i n 25 f r act i ons wi t h 5.4 G y boost ) wi t h pr eoper at i ve C RT ( 45 G y i n
25 f r act i ons) . Wi t h m edi an 5.4 year s of f o l l ow up per i od, t he r at e of
l ocal r ecur r ence at 5 year s wer e 8% i n pr eo per at i ve C RT gr oup ( n =506) ,
wher eas 13% i n pr eo p er at i ve RT gr oup ( n= 5 05) . T her e was no si gni f i cant
di ff er ence bet ween t wo gr oups on 5 year s o ver al l sur vi val r at e wi t h
64.8% i n pr eoper at i ve RT gr oup and 65 .8 % i n pr eoper at i ve C RT gr oup
( p=0.84) . In E O RT C 22921 t r i al usi ng l i mi t ed r adi at i on f i el d, pCR r at e
was 13 .7% ( Bosset et al , 2005) . T hi s r at e i s not di ff er ent c o mpar e d wi t h
CRT wi t h st andar d f i el d.
T he appl i cat i on of l i mi t ed f i el d i n pr eoper at i ve t r eat ment see ms t o be
r easonabl e si nce t he 5 year s l ocal f ai l ur e r a t e was r educe d f r o m 3 0% t o
4% af t er T ME was d one ( Bosset et al , 2 005) . Pr eo per at i ve r adi at i on
t her apy usi n g l i mi t ed vol u me sho wed co mpar abl e r esponse r a t e and
l esser t oxi ci t i es. Al t hou gh l on ger f ol l o w -u p i s needed t o co nf i r m t he
i mpact on t he l ocal c ont r ol and sur vi val , many i nst i t ut es i ncl udi n g our s
have used l i mi t ed vo l u me si nce f a vor abl e r esul t s of T ME ha ve been
r epor t ed. It i s qui t e p ossi bl e t hat hi gh dose coul d be del i ver ed t o l i mi t ed
vol u me b y t echni que wi t h i nt ensi t y mo dul at ed r adi ot her ap y ( IMRT ) .
Because l oc or e gi onal f ai l ur es co mmo nl y o ccur r ed i n t he l o w p el vi c
gi ven t o t hat l esi on, especi al l y i n pat i ent s at hi gh r i s k of l ocor egi onal
f ai l ur e ( Yu et al , 2008) . Recent l y, mol ecul ar i ma gi n g usi n g t r ac er ( e.i .,
1 8
F -f l uor o mi soni da zol e (1 8F -FM IS O) ) has been used i n assess ment of
hypoxi c or r adi or esi s t ant r egi ons . 1 8F -FM I SO P ET scanni n g ma y hel p
l ocal i ze t he boost f i el d, wh er e pr oba bl y b enef i t f r o m mor e i nt ense or
hi gher doses of r adi at i on i n hi gh r i s k p at i ent s. Wi t h co mbi nat i on of
hypoxi c i ma ge, IM RT coul d possi bl y gi ve hi gher dose t o t he b oost f i el d
and i mpr o ve t he l ocal cont r ol wi t hout i ncr e ment of si de eff ect s.
Hi gh r adi at i on dose i s an i ndependent f act o r t o aff ect pCR . San g her a
et al . updat ed f act or s aff ect i ng pat hol o gi c r esponse, based on 4732
pat i ent s t r eat ed wi t h p r eoper at i ve C RT i n pr ospect i ve phase I I and phase
I I I t r i al s ( Sangher a et al , 2008) . Si gni f i cant f act or s associ at ed wi t h pCR
wer e t he use of t w o dr ugs , i nf usi onal ad mi ni st r at i on of 5 -f l ur our ac i l , and
r adi ot her apy dose of 45 G y and abo ve . T h e adj ust ed mean pC R r at e i n
l esser t han 45G y was 0.09 co mpar ed wi t h 0. 20 ( 95% conf i dence i nt er val ,
0.10 -0.31) i n mor e t h an 55 G y ( P=0 .02) . Mohi uddi n et al . r epo r t ed t he
cor r el at i on bet ween hi gher dose of r adi a t i on and t he l i kel i h ood of
achi evi n g pC R. p CR r at e was obser ved i n 4 4% of pat i ent s who r e cei ved
r adi at i on dose ≥55 G y as co mpar ed t o 1 3 % of pat i ent s t r eat ed wi t h a
dose ≤50 G y ( p=0.0 5) ( Mohi uddi n et al , 20 0 0)
Se ver al st udi es r epor t ed si gni f i cant cor r el at i ons bet ween dow nst agi n g
sur vi val . Mohi uddi n e t al r epor t ed t hat 5 ye ar o ver al l sur vi val wa s 100%
f or ypT 0–2 N0 co mpar ed wi t h 80% f or ypT 3–4N0 and 73% f or pT xN1–2
( Mohi uddi n et al , 2000) . Tsuj i naka et al showed t hat t her e wer e b enef i t s
of 5 year sur vi val r at e ( 79.5% , p=0.01 5) and 5 year l ocal r ecur r enc e -f r ee
r at e ( 100% , p= 0.034) i n r espon der s af t er p r eoper at i ve r a di ot her apy f or
l ocal l y ad vanced l o w r ect al cancer (Tsuj i naka et al , 2008) . Lon ger f ol l ow
up i s needed t o de mo nst r at e whet her pat i ent wi t h pat hol o gi c c o mpl et e
r esponse had f a vor abl e out co me .
In ad di t i on t o shor t c our se and con ve nt i on al sche mes as modal i t y of
pr eoper at i ve r adi ot her apy i n l ocal l y ad va nce d r ect al cancer, pr e op er at i ve
hyper f r act i onat ed accel er at ed r adi ot her apy ( HA RT ) has been pr o p osed t o
i mpr o ve t he l ocal c ont r ol b y a voi da nce of del a yi n g bet wee n t wo
modal i t i es, based on t he f easi bi l i t y of t r i al 89 -0 1 ( post -op H A RT; 48 G y
i n 3 wee ks) ( Couc ke et al , 19 93) . In 91 -0 1 t r i al ( Couc ke et al , 1995) ,
pr eoper at i ve HA RT ( 41.6 G y i n 2 .5 wee ks) f ol l o wed b y i mmedi at e
surger y was f easi bl e wi t h l ower acut e t oxi ci t y, co mpar e d t o
post oper at i ve H A RT.
Accel er at ed r epop ul at i on r educes l ocal co nt r ol , especi al l y i n r api d
pr ol i f er at i ng t u mor s, a nd t he pr ol on gat i on of over al l t r eat ment t i me ( OT )
i s r el at ed wi t h poor out co me. T her ef or e, accel er at ed hyper f r act i o nat i on
sche me co ul d i mpr o ve l ocal cont r ol b y t he c o mpensat i on of r epop ul at i ng
r adi ot her apy i n t hi s st ud y was del i ver ed i n s pl i t cour se wi t h pl anned r est
per i od of about 10 -12 days . Fo wl er su ggest ed t hat t r eat ment out c o me i s
bet t er when l arger nu mber s of s mal l er f r act i ons ar e used wi t h a s el ect ed
OT ( Fowl er, 1990) . In t hi s st udy, we suggest that because larger numbers of s mal l er f r act i ons wer e del i ver ed wi t ho ut t he pr ol on gat i on of OT
co mpar ed wi t h co n ven t i onal sche me, l ocal c ont r ol i n t hi s sche me ma y be
not bad t han c on vent i o nal sche me.
In t hi s st ud y, t her e w er e 4 pat i ent s ( 11.4% ) who achi e ved p CR. pCR
r at e i n t hi s st ud y i s s mal l er t han 10 -30% i n ot her st u di es. T hi s ma y be
due t o t u mor vol u me . St udi es on pr et r eat me nt T 4 t u mor i n l ess t han 20%
showed o ver 20% of pCR r at es. In Radi at i on T her ap y Oncol o gy Gr ou p
( RTO G) Tr i al 0012 ( Mohi uddi n et al , 2006 ) , p CR r at e af t er pr eo per at i ve
CRT was 33% i n pr et r eat ment T 3 t u mor, wh er eas 18% i n pr et r eat ment T 4
t u mor. If concer ni n g t hat i n t hi s st ud y so me had f i xed or t et her ed r ect al
mass, pr et r eat me nt T 4 t u mor wer e 31% , or or al che mot her apeut i c agent
occupi ed hi gh pr op o r t i on ( 20% ) , our r es ul t s ma y be consi de r ed t o
co mpar abl e.
In spi t e of ac ut e t oxi ci t y, B ID pr ot ocol wi t h spl i t cour se i n our pr e sent
st udy ha d a f ew i nt er r upt i ons of RT, no r ed uct i on of r adi at i on dose, and
no di scont i nuat i on. Fu r t her mor e se ver e l at e t oxi ci t i es wer e f ound i n onl y
t wo pat i ent s; del a yed per i neal wound heal i n g a nd f i st ul a, r espect i vel y.
st age t u mor s. T her ef or e, accur at e pr et r eat me nt st a gi n g i s not onl y
i ndi spensabl e t o a voi d unnecessar y pr eo per a t i ve mul t i modal t r eat ment i n
ear l y st a ge r ect al cancer, but al so t o i dent if y l ocal l y ad vanced d i sease.
Al t hou gh j udi ci ous a ppl i cat i on of t echnol ogi es, i ncl udi n g CT / MR I and
EUS, a nd t he ad va nce of i nno vat i ve t echni ques, i ncl udi n g 3D
-endosonoscop h y, ma y f ur t her i mpr o ve accur acy of st a gi n g, caut i o ns ar e
needed t o deci de whe t her pat i ent s shoul d be t r eat ed wi t h pr eoper at i ve
modal i t y.
B ID r adi at i on t her ap y wi t h concur r ent 5 -F U bas ed c he mot her ap y had
co mpar abl e t r eat ment out co me and l ess ac ut e t oxi ci t i es and t ol er abl e.
T her ef or e, t hi s t r eat ment pr ot ocol coul d be consi der ed t o be a t ol er abl e
al t er nat i ve i n pat i ent s wi t h l ocal l y ad vanced r ect al cancer.
St udi es wi t h l arge nu mber of pat i ent s ar e war r ant ed t o conf i r m t he
i ncr easi ng of t ol er abi l i t y wi t hout t he i nt er r upt i on of r adi ot her apy, and
possi bl y t o enhance t h e t u mor shr i n ka ge i n a dva nced r ect al cancer.
1. Bosset JF, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, Daban A, Bardet E,
Beny A, Briffaux A, Collette L: Enhanced tumorocidal effect of chemotherapy with preoperative radiotherapy for rectal cancer: preliminary results--EORTC 22921. J
Clin Oncol 23:5620-5627, 2005
2. Bosset JF, Related Articles, LinksBosset JF, Collette L, Calais G, Mineur L,
Maingon P, Radosevic-Jelic L, Daban A, Bardet E, Beny A, Ollier JC:
Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med
355:1114-1123, 2006
3. Colorectal Cancer Collaborative Group: Adjuvant radiotherapy for rectal cancer: a
systematic overview of 8,507 patients from 22 randomised trials. Lancet
358:1291-1304, 2001
4. Coucke PA, Cuttat JF, Mirimanoff RO: Adjuvant postoperative accelerated
hyperfractionated radiotherapy in rectal cancer: a feasibility study. Int J Radiat
5. Coucke PA, Sartorelli B, Cuttat JF, Jeanneret W, Gillet M, Mirimanoff RO: The rationale to switch from postoperative hyperfractionated accelerated radiotherapy to
preoperative hyperfractionated accelerated radiotherapy in rectal cancer. Int J Radiat
Oncol Biol Phys 30:181-8, 1995
6. Fisher B, Wolmark N, Rockette H, Redmond C, Deutsch M, Wickerham DL, Fisher
ER, Caplan R, Jones J, Lerner H, et al.: Postoperative adjuvant chemotherapy or
radiation therapy for rectal cancer: results from NSABP protocol R-01. J Natl
Cancer Inst 80:21-29, 1988
7. Fowler JF: How worthwhile are short schedules in radiotherapy? A series of
exploratory calculations. Radiother Oncol 18:165-81, 1990
8. Gastrointestinal Tumor Study Group: Prolongation of the disease-free interval in
9. Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, Rutten HJ,
Pahlman L, Glimelius B, van Krieken JH, Leer JW, van de Velde CJ: Preoperative
radiotherapy combined with total mesorectal excision for resectable rectal cancer. N
Engl J Med 345:638-646, 2001
10. Krook JE, Moertel CG, Gunderson LL, Wieand HS, Collins RT, Beart RW, Kubista
TP, Poon MA, Meyers WC, Mailliard JA: Effective surgical adjuvant therapy for
high-risk rectal carcinoma. N Engl J Med 324:709-715, 1991
11. Minsky BD: Adjuvant therapy for rectal cancer--a good first step. N Engl J Med
336:1016-1017, 1997
12. Mohiuddin M, Hayne M, Regine WF, Hanna N, Hagihara PF, McGrath P, Marks
GM: Prognostic significance of postchemoradiation stage following preoperative
chemotherapy and radiation for advanced/recurrent rectal cancers. Int J Radiat
13. Mohiuddin M, Regine WF, John WJ, Hagihara PF, McGrath PC, Kenady DE, Marks
G: Preoperative chemoradiation in fixed distal rectal cancer: dose time factors for
pathological complete response. Int J Radiat Oncol Biol Phys 46:883-888, 2000
14. Mohiuddin M, Winter K, Mitchell E, Hanna N, Yuen A, Nichols C, Shane R,
Hayostek C, Willett C: Randomized phase II study of neoadjuvant
combined-modality chemoradiation for distal rectal cancer: Radiation Therapy Oncology
Group Trial 0012. J Clin Oncol 24:650-655, 2006
15. NIH consensus conference. Adjuvant therapy for patients with colon and rectal
cancer. Jama 264:1444-1450, 1990
16. Roof KS, Coen J, Lynch TJ, Wright C, Fidias P, Willett CG, Choi NC: Concurrent
cisplatin, 5-FU, paclitaxel, and radiation therapy in patients with locally advanced
17. Rosen LS, Bilchik AJ, Beart RW Jr, Benson AB 3rd, Chang KJ, Compton
CC,Grothey A, Haller DG, Ko CY, Lynch PM, Nelson H, Stamos MJ, Turner RR,
Willett CG: New approaches to assessing and treating early-stage colon and rectal
cancer: summary statement from 2007 Santa Monica Conference. Clin Cancer Res
13:6853s-6856s, 2007
18. Sanghera P, Wong DW, McConkey CC, Geh JI, Hartley A: Chemoradiotherapy for
rectal cancer: an updated analysis of factors affecting pathological response. Clin
Oncol (R Coll Radiol) 20:176-183, 2008
19. Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, Martus P,
Tschmelitsch J, Hager E, Hess CF, Karstens JH, Liersch T, Schmidberger H, Raab
R: Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J
Med 351:1731-1740, 2004
20. Sobin LH, Wittenkind CH: International Union Against Cancer. TNM calssification
21. Swedish Rectal Cancer Trial: Improved survival with preoperative radiotherapy in
resectable rectal cancer. N Engl J Med 336:980-987, 1997
22. Tsujinaka S, Kawamura YJ, Konishi F, Aihara H, Maeda T, Mizokami K:
Long-term efficacy of preoperative radiotherapy for locally advanced low rectal cancer. Int
J Colorectal Dis 23:67-76, 2008
23. Willett CG, Czito BG, Bendell JC: Radiation therapy in stage II and III rectal cancer.
Clin Cancer Res 13:6903s-6908s, 2007
24. Wolmark N, Wieand HS, Hyams DM, Colangelo L, Dimitrov NV, Romond EH,
Wexler M, Prager D, Cruz AB Jr, Gordon PH, Petrelli NJ, Deutsch M, Mamounas E,
Wickerham DL, Fisher ER, Rockette H, Fisher B: Randomized trial of postoperative
adjuvant chemotherapy with or without radiotherapy for carcinoma of the rectum:
National Surgical Adjuvant Breast and Bowel Project Protocol R-02. J Natl Cancer
25. Yu TK, Bhosale PR, Crane CH, Iyer RB, Skibber JM, Rodriguez-Bigas MA, Feig
BW, Chang GJ, Eng C, Wolff RA, Janjan NA, Delclos ME, Krishnan S, Das P:
Patterns of locoregional recurrence after surgery and radiotherapy or chemoradiation
- 국문요약-
국소진행성
국소진행성
국소진행성
국소진행성 직장암
직장암
직장암 환자의
직장암
환자의
환자의 술
환자의
술 전
술
술
전
전
전 병용
병용
병용
병용 항암
항암
항암
항암
: BID
: BID
: BID
: BID 방사선요법
방사선요법
방사선요법
방사선요법
아주대학교 대학원의학과 이선영 (지도교수: 전미선) 연구목적: 국소진행성 직장암 환자의 병용 항암요법의 치료효과, 순응도 및 부작용을 알아보고자 한다. 재료 및 방법: 2001 년 1 월부터 2007 년 12 월까지 국소진행성 직장암으로 술 전 방사선치료를 시행한 환자 35 명을 대상으로 분석하였다. 모든 환자는 5-FU 를 기본으로 하는 항암치료를 받았으며, 주로 사용된 항암제는 FOLFIRI (n=25)이였고, 대부분의 환자에서 방사선치료 중 총 3 차례가 시행되었다. 방사선치료는 다음과 같이 시행되었다: 일회에 1.5 Gy 씩 하루에 두 차례 첫 항암치료와 함께 21-24 Gy 시행되었고, 10-12 일간의 쉬는 기간 후에, 같은 방식으로 2 번째 항암치료와 함께 21-24 Gy 의 방사선이 조사되었다. 결과: 중앙추적관찰 기간은 19 개월 (5-36)이었다. 모두가 T3 (n=25) 혹은 T4 (n=10)이였고 가장 큰 종양의 지름은 중앙값 5cm (2.5-14cm)이었다. 총 병기감소는 71%이였고, 병리적 완전 관해율은 11% (n=4), 거의 완전 관해율 23% (10% 미만의 세포가 살아있는 현미경적 국소잔류종양) (n=8),
부분관해 60% (n=21)이였다. 2 명은 수술이 불가능하였다. 괄약근 보전 술식은 하부직장암인 30 명중 43%에서 가능하였다. 7 명 (20%)이 1~7 일간 다음과 같은 이유로 방사선치료를 쉬었다: 회음부 피부 부작용 3 명, 항암치료 부작용 3 명, 항문농양 1 명. 7 명만 (20%) 심한급성 부작용을 경험하였다 (4 명에서 등급 3 중성구 감소, 2 명에서 각각 등급 3, 등급 4 회음부 피부 부작용, 1 명에서 등급 3 직장염). 두 명은 각각 개방성 회음부 상처 지연과 직장 질 누공로 지연 부작용을 경험하였다 결론: 본 논문에서 국소진행성 직장암에서 술 전 BID 방사선치료와 동시에 항암 화학 요법 시 34%의 완전 및 거의 완전 관해율을 얻었다. 이 치료방법은 비슷한 치료효과를 갖고 더 좋은 순응도로 국소진행성 직장암 환자에서 술 전 요법으로 시행 될 수 있을 것으로 생각된다. 핵심어: 직장암, 술 전, 동시 항암 화학 방사선치료