Pituitary Gland (Hypophysis, 뇌하수체)
병 리 과2006. 9. 18
김 교 영
Pituitary Gland (Hypophysis, 뇌하수체)
• A small bean-shaped organ
• About 1 cm, 05 gm
• Enlarge during pregnancy
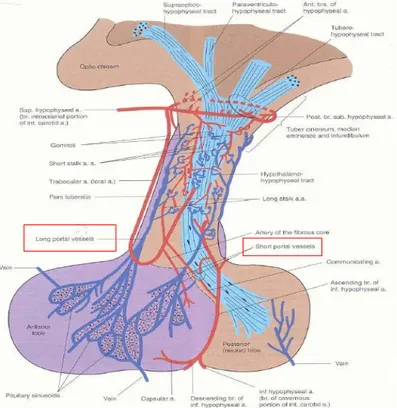
• Attached to hypothalamus by pituitary stalk
• Two component
– Anterior lobe (adenohypophysis, 샘뇌하수체)
– Posterior lobe (neurohypophysis, 신경뇌하수체)
The adenohypophysis (anterior pituitary) releases five hormones that are in turn under the control of various stimulatory and inhibitory hypothalamic releasing factors.
•TSH, thyroid-stimulating hormone (thyrotropin) • PRL, prolactin
• ACTH, adrenocorticotrophic hormone (corticotropin) • GH, growth hormone (somatotropin) • FSH, follicle-stimulating hormone • LH, luteinizing hormone. • TRH (thyrotropin-releasing factor) • CRH (corticotropin-releasing factor) • GHRH (growth hormone-releasing factor) • GnRH (gonadotropin-releasing factor).
• The inhibitory hypothalamic influences are comprised of PIF (prolactin inhibitory factor or dopamine) and growth hormone inhibitory factor (GIH or somatostatin).
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier
Hormones released by the anterior pituitary
Localization of Anterior Pituitary
Figure 24-2 A, Photomicrograph of normal pituitary. The gland is populated by several distinct cell populations containing a variety of stimulating (trophic) hormones. B, Each of the hormones has different staining characteristics, resulting in a mixture of cell types in routine histologic preparations. Immunostain for human growth hormone.
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier Immunostain for human Growth Hormone
Cells of Anterior Pituitary
•Acidophilic (esosinophilic cytoplasm) • Basophilic (basophilic cytoplasm) • Chromophobe (poorly staining cytoplasm)
Pituitary Gland (Hypophysis, 뇌하수체)
Normal
- 0.5 gm, 1 ~ 1.5 cm
No antibody angainst the pituitary hormone 6) Chromophobes (15-20%) Basophil FSH, LH 5) Gonadotrophs Basophil TSH 4) Thyrotrophs Basophil ACTH, MSH Lipotrophin, Endorphin Pro-piomelanocortin (POMC) 3) Corticotrophs Acidophil Prolactin 2) Lactotrophs (mammotrophs) Acidophil Producing GH outpouching of floor of 3rd ventricle Rathke's pouch 유래
unmyelinated nerve fibers containing secretory granule [vasopressin (ADH), oxytocin] 1) Somatotrophs (50%)
조직
Neurohypophysis Adenohypophysis (80%)
pituicyte (modified glial cells) secretory epithelial cells
구성
Posterior lobe Anterior lobe
Posterior Pituitary
Herring body (axonal swelling)
Pituicyte
• Axon
• Glial cells (pituicyte) • Vascular network
Disease of the Pituitary
1) Increased or decreased tropic Hormone
production
– Hyperpituitarism (뇌하수체 기능항진증)
– Hypopituitarism (뇌하수체 기증저하증)
• ≥ 75% destruction:
– ischemic injury, radiation, inflammatory reaction, non-functioning neoplasm
2) Local effects
– Enlargement of sella turcica by x-ray film
– visual field defect : bitemporal hemianopsia
– increased intracranial pressure (ICP↑)
Pituitary Adenomas
• Most common cause of hyperpituitarism arising in the anterior lobe
• Incidence
– 10% of intracranial neoplasm (25% of autopsy cases) – adult (30-50세)
• Functional adenoma
– Hormone excess and clinical manifestation
• Silent adenoma
– Immunohistochemical and/or ultrastructural demonstration of hormone production at the tissue only, without clinical symptoms of hormone excess
• Hormone-negative adenoma (“null cell adenoma”)
• rarely nonfunctioning adenoma
→ normal anterior lobe 눌러 hypopituitarism 유발
Classification of Pituitary Adenomas
Hormone-negative adenomas Other plurihormonal adenomas
Mixed growth hormone-prolactin cell (mammosomatotroph) adenomas
Silent gonadotroph adenomas include most so-called null cell and oncocytic adenomas
Gonadotroph cell adenomas ACTH cell (corticotroph) adenomas
Thyroid-stimulating hormone cell (thyrotroph) adenomas
Densely granulated GH cell adenoma
Sparsely granulated GH cell adenoma with fibrous bodies
Growth hormone cell (somatotroph) adenoma Prolactin cell (lactotroph) adenoma
ACTH, adrenocorticotropic hormone
Pituitary Adenomas
•
3% of cases a/w MEN (multiple endocrine
neoplasia, type 1 (Wermer syndrome, 3P's)
1. Parathyroid hyperplasia (primary
hyperparathyroidism : most common
manifestation)
2. Pancreatic islet cell tumor
3. Pituitary
adenoma: 주로 prolactinoma
•
Microadenoma: less than 1 cm in diameter
•
Macroadenoma: exceed 1 cm in diameter
–
Silent an hormone-negative adenomas
Pituitary Adenomas
•
Pathogenesis
– Monoclonal in origin: arise from a single somatic cell
– G-protein mutation
– MEN (multiple endocrine neoplasia) syndrome, type 1
– Activating mutation of RASoncogene
• Aggressive or advanced adenoma
– Overexpression of c-MYConcogene
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier
The mechanism of G-protein mutations in endocrine neoplasia
• Mutations in the G-protein-signaling pathway are seen in a variety of endocrine neoplasms, including pituitary, thyroid, and parathyroid adenomas.
• G-proteins play a critical role in signal transduction, transmitting signals from cell-surface receptors (GHRH, TSH, or PTH receptor) to intracellular effectors (e.g., adenyl cyclase), which then generate second messengers (cAMP). • G-protein mutation
– mutation of GNAS1(Guanine
nucleotide-binding protein Gs, alpha
subunit) gene (gsponcogene)
Æ interfere with its intrinsic GTPase activity
Æ constitutive activation of Gsα
Æ persistent generation of cAMP Æ unchecked cellular proliferation
• 40% of somatotroph cell adenoma
• Minority of corticotroph adenoma
• Absent in thyrotroph, lactotroph, and
gonadotroph adenoma
Pituitary Adenomas
• Morphology *
<Gross>
• microadenoma (<1 cm)
– 40% of unselected autopsy, single or multiple
• macroadenoma (>1 cm)
– expansile, bony erosion
suprasellar extension through the diaphragm of the sella.
Coronal section of sella showing diffuse tumor that fills sella and compresses residual pituitary tissue into thin peripheral rim. Note moderate suprasellar extension. (Whole mount, H&E)
Pituitary apoplexy
.
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier
• This massive, nonfunctional adenoma has grown far beyond the confines of the sella turcica and has distorted the overlying brain. • Nonfunctional adenomas tend to be larger at the time of
diagnosis than those that secrete a hormone
Pituitary Adenomas
• Morphology *
<Micro>
• uniform appearance
• sheets, cords, or nests of cells having only a delicate, vascularized stroma, absence of reticulin network • pseudoglanduar, papillary formation
• invasive adenoma (30%)
– not grossly encapsulated, infiltrate adjacent bone and dura or brain
• ischemic necrosis, psammoma body, hemorrhage
– "pituitary apoplexy" - acute hemorrhage into an adenoma
• variation in cell and nuclear size and shape in rapidly growing adenoma
• mitosis : variable
The monomorphism of these cells contrasts markedly with the mixture of cells seen in the normal anterior pituitary.
Note also the absence of reticulin network.
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier
Pituitary Adenomas
Pituitary adenoma invasive to brain. (H&E)
Pituitary adenoma. Diffuse pattern. (H&E.) Pituitary adenoma. Sinusoidal pattern. (H&E.)
A, Electron micrograph of a sparsely granulated prolactinoma. The tumor cells contain abundant granular endoplasmic reticulum (indicative of active protein synthesis) and small numbers of secretory granules (6000x).
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier
B, Electron micrograph of densely granulated growth hormone-secreting adenoma. The tumor cells are filled with large, membrane-bound secretory granules (6000x).
(Courtesy of Dr. Eva Horvath, St. Michael's Hospital, Toronto, Ontario, Canada.)
Electron Micrograph
• Sparse or abundant secretory granules
1. Prolactinomas (lactotroph adenomas)
• most frequent type of hyperfunctioning pituitary
adenoma (30% of all pituitary tumors)
• micro- to macroadenoma
– weakly acidophilic or chromophobic cells (sparsely granulated prolactinoma)
– rarely strongly acidophilic (densely granulated prolactinoma)
• Propensity to undergo dystrophic calcification
– Isolated psammona body– Extensive calcification (“pituitary stone”)
• Prolactinemia
Æ amenorrhea, galactorrhea, loss of libido & infertility
• more obvious in premenopausal female • Dx. at earlier stage
Prolactin immuno staining
2. Somatotropic adenomas (Somatotroph)
• GH ↑ → acromegaly, gigantism
• Gigantism (거인증)
– Excessive secretion prior to closure of the
epiphyseal plates
– Long limbs
– Height reaches 7-8 feet tall
– Can be mentally retarded
• Acromegaly (말단비대증)
– Excessive secretion after growth has been
completed
– Large hands and feet, mandibles, facial features
• Usually small microadenoma
• Basophilic or chromophobic
• ACTH ↑ → adrenal hypersecretion of cortisol
→ Hypercortisolism (“Cushing disease”)
• Nelson syndrome
– large, aggressive corticotroph adenoma after
surgical remove of adrenal glands
– absence of adrenal gland → no hypercortisolism
ACTH immunostaining3. Corticotroph tumors
• Nonfunctional adenoma (25%)
– Clinically silent (silent somatotroph adenoma) – Hormone-negative adenoma (Null cell adenoma)
• Unusual
– Mass effect – most presentation
• Gonadotroph adenoma (10-15%)
– Chromophobic cells
• Thyrotroph adenoma (1%) – TSH
• Pituitary carcinoma (quite rare)
– Demonstration of metastasis – Lymph node, bone, liver
4. Other anterior pituitary adenomas
Hypopituitarism (뇌하수체 기능저하증)
• Decreased secretion of pituitary hormone
– Result from disease of hypothalamus or pituitary
• Hypopituitarism with posterior pituitary dysfunction in the form of diabetes insipitus (요붕증)
– Almost always of hypothalamic origin
• Hypofunction of the anterior pituitary
– loss or absence of ≥ 75% anterior pituitary parenchyme
• Hypopituitarism의 90%이상의 원인
– adenohypophysis를 직접적으로 involve 하는 destructive process에 의해
– 그 중 most common한 3가지 원인은
• Tumor (nonsecreting adenoma) (비분비 뇌하수체샘종) • Sheehan's pituitary necrosis (시한증후군)
Hypopituitarism (뇌하수체 기능저하증)
• Hypofunction of anterior pituitary1) Nonsecretory pituitary adenoma
• Gradual (adenoma) • Pituitary apoplexy
– Sudden hemorrhage into pituitary gland – Excruciating headache, diplopia, hypopituitarism – Neurosurgical emergency
2) Ischemic necrosis of the pituitary
• Sheehan's syndrome (postpartum necrosis of pituitary)
– most common form of clinically significant ischemic necrosis of the ant. pituitary
– during pregnancy, anterior pituitary enlarge (x2), not accompanied by an increased blood supplyfrom low pressure venous system (obstetric hemorrhage and shock Æ infarction of anterior pituitary
3) Ablation of the pituitary by surgery of radiation
Hypopituitarism (뇌하수체 기능저하증)
• Hypofunction of anterior pituitary4) Rathke cleft cyst
• Cyst, lined by ciliated cuboidal epithelium with goblet cell and anterior pituitary gland
• Ablation by surgery or radiation Æ empty sella
5) Empty sella syndrome
• destroy part or all of pituitary gland, primary or secondary 1) primary empty sella
– Defect in diaphragma sellaÆ arachnoid mater and CSF herniate into sella Æ
expansion of sella and compression of pituitary
2) secondary empty sella
– Mass, pituitary adenoma Æ enlarge sella Æ surgical removal or spontaneous necrosis Æ loss of pituitary function
6) Genetic factors
• Mutation in pit-1(pituitary transcription factor) Æ combined deficiency of GH, prolactin, and TSH
Hypopituitarism (뇌하수체 기능저하증)
•
Hypothalamic lesions
1) Tumors
–
Craniophryngioma, metastatic tumor from
breast, lung
–
Brain or nasophryngeal tumor with radiation
2) Inflammatory disorders and infections
•
Sarcoidosis
•
Tuberculous meningitis
Posterior pituitary syndromes
(뇌하수체후엽증후군)
• Diabetes insipidus (요붕증)
– ADH deficiency
• excessive urination (polyuira)
• increased serum sodium and osmolality → thurst and polydipsia
– Causes
• head trauma, neoplasm and inflammatory disorders, surgical procedures involving hypothalamus and pituitary
• Syndrome of inappropriate ADH (SIADH)
– ADH excess
• resorption of excessive amounts of free water, hyponatremia
– Causes :
• secretion of ectopic ADH by malignant neoplasm – most common
– small cell lung carcinoma, thymoma, pancreas tumor, lymphoma,
• non-neoplastic disease of the lung
Hypothalamic Suprasellar Tumors
• Glioma and craniopharyngioma
– Most common• Craniopharyngioma
– 3-4 cm– Encapsulated and solid – Cystic and multiloculated
– Two variants
• Adamantinomatous craniopharyngioma
– Squamous epithelium in spongy reticulum with peripheral palisading
– Frequently calcification – Keratin formation, cyst
• Papillary craniopharyngioma
– Papillae, lined by squamous epithelium without peripheral palisading and spongy reticulum
– Lack keratin, calcification and cysts
Thyroid Gland
Thyroid gland (갑상샘)
• Normal
1) 발생
• Root of tongue (foramen cecum) 에서
생겨 trachea의 anterior side와 thyroid
cartilage쪽으로 downward growth
2) Congenital anomaly
• Site에 문제
– Lingual or aberrant subhyoid thyroid – Substernal thyroid gland
• Malformations of branchial pouch
differentiation
– Intrathyroidal sites of thymus or parathyroid가 형성
Thyroid gland
•
Normal
1) 15-25 gm in adult 2) Lobules : 20-40 follicles 3) 조직학적 소견• variable-sized follicles lined by regular cuboidal cells • neuroectodermal calcitonin-secreting ‘C-cells’ or
‘parafollicular cells’
– lateral lobe의 upper와 middle 1/3 junction에 많이 분포 – Function of calcitonin
» Promote the absorption of calcium by the skeletal system » Inhibit the resorption of bone by osteoclasts
Immunoreactivity for calcitonin in thyroid C cells.
Metabolism
• Thyroid follicular epithelial cell converts thyroglobulin
to T4 (thyroxine) and T3 (Triiodothyronine)
Æ
systemic release
• T4 and T3 + thyroxine-binding globulin (TBG) and
transthyrenin
Æ transport to peripheral tissue
• In the periphery, free T4 is deionated to T3
⇒ unbound or free T3 ⇒ more effective function ⇒ interact with nuclear thyroid hormone receptor (TR)
⇒ form hormone-receptor complex ⇒ translocate to nucleus ⇒ bound to thyroid response elements (TREs) in the target
gene
⇒ transcription
➡ ↑ during puberty, pregnancy, and physiologic stress
• Secretion of thyroid hormones (T3 and T4) is controlled by trophic factors secreted by both the hypothalamus and the anterior pituitary.
• Decreased levels of T3 and T4 stimulate the release of thyrotropin-releasing hormone (TRH) from the hypothalamus and thyroid-stimulating hormone (TSH) from the anterior pituitary, causing T3 and T4 levels to rise.
• Elevated T3 and T4 levels, in turn, suppress the secretion of both TRH and TSH. (negative-feedback loop) • TSH binds to the TSH receptor on the thyroid follicular epithelium, which causes activation of G proteins, and cyclic AMP (cAMP)-mediated synthesis and release of thyroid hormones (T3 and T4).
• In the periphery, T3 and T4 interact with the thyroid hormone receptor (TR) to form a hormone-receptor complex that
translocates to the nucleus and binds to so-called thyroid response elements (TREs) on target genes initiating transcription.
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier
Homeostasis in the hypothalamus-pituitary-thyroid axis and mechanism of action of thyroid hormones
Thyroid hormone
• Cellular effect
– Up-regulation of carbohydrate and lipid catabolism – Stimulation of protein synthesis
Æ net result: increase in basal metabolic rate (BMR)
• Brain development
• Response to stimuli
• During puberty, pregnancy, and physiologic stress
– Increase in size and more activeMetabolism
• Inhibitors; goitrogens
: suppress T3 and T4 synthesis Æ increase levels of TSH Æ subsequent hyperplastic enlargement of the gland (goiter)
– antithyroid agents: propylthiourcil (PTU)
⇒ Inhibit oxidation of iodide and block production of thyroid H. ⇒ inhibit peripheral deiodination of circulating T4 into T3
– Iodine, when given to pt with thyroid hyperfunction
⇒ also blocks release of thyroid hormones
➡ Large doses Iodide ⇒ inhibit proteolysis of thyroglobulin
⇒ Incorporated within increasing amounts of colloid ⇒ not released into the blood
➡ Iodine Tx
⇒ distended follicles with thyroglobulin and stromal vascularization, inactive gland
Pathology of Thyroid
• Disease of thyroid
– Medical and surgical management
• Hyperthyroidism (갑상샘기능항진증)
• Hypothyroidism (갑상샘기능저하증)
• Mass
Hyperthyroidism
• Thyrotoxicosis:
– hypermetabolic state by elevated free T3 & T4
– most common cause: hyperfunction of thyroid
(hyperthyroidism)
– often in woman
– Thyrotoxicosis ≥ Hyperthyroidism
• Excess release of preformed thyroid H. (thyroiditis) or extrathyroidal source 도 포함
– Three most common cause of thyrotoxicosis
• Diffuse hyperplasia a/w Graves disease (85%) • Hyperfunctional multinodular goiter• Hyperfucntional adenoma
Disorders Associated with Thyrotoxicosis
Subacute granulomatous thyroiditis (painful) Subacute lymphocytic thyroiditis (painless)
Struma ovarii (ovarian teratoma with ectopic thyroid) Factitious thyrotoxicosis (exogenous thyroxine intake)
Not Associated with Hyperthyroidism Primary
Diffuse toxic hyperplasia (Graves disease) (85%) Hyperfunctioning ("toxic") multinodular goiter Hyperfunctioning ("toxic") adenoma
Hyperfunctioning thyroid carcinoma Iodine-induced hyperthyroidism
Neonatal thyrotoxicosis associated with maternal Graves disease
Secondary
TSH-secreting pituitary adenoma (rare)*
Associated with Hyperthyroidism
*Associated with increased TSH; all other causes of thyrotoxicosis associated with decreased TSH.
Hyperthyroidism
◈ Clinical course
–
Hypermetabolic state
–
Overactivity of sympathetic nervous system
• Increase in the ß–adrenergic “tone”
1) Increase BMR (basal metabolic rate)
–
Skin: soft, warm, flushed
• Increased blood flow• Peripheral vasodilation to increase heat loss
–
Sweating
Å high level of calorigenesis
–
Weight loss depite increased appetite
Hyperthyroidism
◈ Clinical course
2) cardiac manifestations
– Earliest sign and most consistent features of hyperthyroidism – Increase in cardiac output owing to
• Increased cardiac contractility
• Increased peripheral oxygen requirements • Tachycardia, palpitations and cardiomegaly • Arrhythmias (atrial fibrillation)
⇒ Myocardial changes
i. Foci of lymphocytic and eosinophilic infiltration ii. Mild fibrosis in the interstitium
iii. Fatty changes in myofibers
iv. Increase in size and number of mitochondria
Hyperthyroidism
◈ Clinical course
3) Neuromuscular system
Overactivity of symphathetic nervous system
• Tremor, hyperactivity, emotional lability, anxiety, inability to concentrate, and insomnia
Thyroid myopathy
• Proximal muscle weakness • Decreased muscle mass
4) Skeletal system
•
Stimulate bone resorption
• Osteoporosis and increased risk of fracture
5) Ocular change
A wide-eyed, staring gaze
• caused by overactivity of the sympathetic nervous system (over stimulation of levator palpabrae superioris) • one of the features of this disorder.
In Graves disease, one of the most important
causes of hyperthyroidism
•
accumulation of loose connective tissue behind the eyeballs also adds to the protuberant appearance of the eyes.Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier
◈ Clinical course
Hyperthyroidism
Hyperthyroidism
◈ Clinical course 6) Gastrointestinal system – Sympathetic hyperstimulation• Hypermobility, malabsorption, and diarrhea
7) Thyroid storm
– abrupt onset of severe hyperthyroidism – underlying Graves disease
– acute elevation of catecholamine levels during infection, surgery, cessation of antithyroid medication, stress
– medical emergency, die of cardiac arrhythmia
8) Apathetic hyperthyroidism
– thyrotoxicosis occurring in the elderly
– blunt the typical features of thyroid hormone excess seen in younger patients
Hyperthyroidism
◈ Diagnosis
① TSH: very low level in primary hyperthyroidism
• Most useful single screening test for hyperthyroidism • → various in hypothalamic or primary pituitary disease
② Free T4: usually increased
③ TRH stimulating test
• normal rise TSH after injection of TRH -- Primary
④ T3toxicosis: TSH - low, T3 - high, T4 - normal
⑤ radioactive iodine uptake -- direct indication of activity
Hypothyroidism (갑상샘기능저하증)
Primary
Developmental (thyroid dysgenesis: PAX-8, TTF-2, TSH-receptor mutations)
Thyroid hormone resistance syndrome (TRß mutations) Postablative
Surgery, radioiodine theraphy, or external radiation
Autoimmune hypothyroidism
Hashmoto thyroiditis
Iodine deficiency
Drugs (lithium, iodides, p-aminosalicylate acid)
Cogenital biosynthetic defect (dyshormonogenetic goiter)
Secondary
Pituitary failure
Tertiary
Hypothalamic failure (rare)
Causes of Hypothyroidism
Hypothyroidism (갑상샘기능저하증)
• Cretinism (크레틴병)
– developing in infancy or early childhood
⑴ Endemic
• dietary iodine deficiency (in Himalaya, inland China, Africa, mountain areas)
⑵ Sporadic
• inborn errors in metabolism (enzyme)
– Clinical features
• impaired development of skeletal & central nervous system
– severe mental retardation, short stature, coarse facial features, protruding tongue, umbilical hernia
Hypothyroidism (갑상샘기능저하증)
• Myxedema (점액부종)
– Developing in older children & adults – Clinical features
• Slowing of physical & mental activity
– generalized fatigue, apathy, mental sluggishness – listless, cold intolerance, overweight
– Reduced cardiac output
Æ shortness of breath & ↓ exercise capacity – Decreased symphathetic activity
Æ constipation and ↓ sweating – Skin
» Cool & pale Å decreased blood flow – Histology
» Accumulation of matrix substance (glycoaminoglycans & hyaluronic acid) in skin, subcutaneous tissue & visceral site
» Edema, broadening & coarsening of facial features, enlargement of tongue, deepening of voice
– Laboratory evaluation
• TSH increase in primary, not in secondary • T4 decrease
Thyroiditis (갑상샘염)
• Infectious thyroiditis : uncommon
– Acute: direct infection via piriform sinus
– Chronic: mycobacterial, fungal,
Pneumocystis
infection
• Hashimoto thyroiditis
• Subacute (granulomatous) thyroiditis
• Subacute lymphocytic (painless) thyroiditis
• Riedel thyroiditis
• Palpation thyroiditis
• Palpation thyroiditis
– Caused by vigorous clinical palpation
– Multifocal follicular disruption with chronic
inflammatory cells and a few
– Functional abnormality is not present
• Riedel's thyroiditis
– Rare, unknown etiology
– Extensive fibrosis, involving thyroid & contiguous
neck structure
– Hard & fixed thyroid mass, stimulating carcinoma
– a/w idiopathic fibrosis, such as retroperitoneum
– Circulating antithyroid antibody in most
Hashimoto Thyroiditis
1)
Most common cause of hypothyroidism in areas of
world where iodine levels are sufficient
2)
45-65 yrs, female (10-20:1)
3)
Gradual thyroid failure Å Autoimmune destruction
of thyroid gland
• Progressive depletion of thyroid epithelial cells (thyrocytes) • Gradually replaced by mononuclear cell infiltration and
fibrosis
Three proposed models for mechanism of thyrocyte destruction in Hashimoto disease. • Sensitization of autoreactive CD4+ T cells to thyroid antigens appears to be the initiating event for all three mechanisms of thyroid cell death. Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM)
© 2005 Elsevier
Pathogenesis of Hashimoto Thyroiditis
Morphology of Hashimoto Thyroiditis
<Gross>
– diffusely or
symmetrically enlarged
– cut surface
• pale, gray-tan, firm,
somewhat nodular
Morphology of Hashimoto Thyroiditis
<Micro>
– mononuclear inflammatory infiltrate (small lymphocytes, plasma cell) and well-developed germinal center
– Hürthle or oxyphil cells - eosinophilic granular cystoplasm – Fibrous variant – follicular atrophy and keloid-like fibrosis
• Not extend beyond the capsule of gland (cf. Reidel thyroiditis)
The thyroid parenchyma contains a dense lymphocytic infiltrate with germinal centers. Residual thyroid follicles lined by deeply eosinophilic Hurthle cells are also seen.
Hashimoto’s thyroiditis with extensive fibrosis, atrophy of follicular epithelium, and squamous metaplasia.
Clinical Course of Hashimoto Thyroiditis
• Clinically painless enlargement of thyroid (symmetric,
diffuse), associated with hypothyroidism
• Transient thyrotoxicosis
– disruption of thyroid follicles• Associated neoplasia
– malignant lymphoma (B cell lymphoma) – papillary carcinoma
• No established risk for developing thyroid epithelial neoplasm
Subacute Granulomatous Thyroiditis
(
De Quervain
Thyroiditis)
• Most common in 30-50세, F:M = 3-5:1
• Pathogenesis
– Caused by viral infection or postviral inflammatory process
• Majority of patient – history of upper respiratory infection just before onset of thyroiditis
• Peak in summer
• Associated with coxsackievirus, mumps, measles, adenovirus • Virus-induced host tissue damage
Æ Viral or thyroid antigen release Æ stimulate cytotoxic T lymphocytes Æ damage thyroid follicular cells
• Not self-perpetuating and process is limited
Morphology of Subacute Granulomatous Thyroiditis
• Gross– Uni- or bilaterally enlarged and firm, with intact capsule – On cut section, the involved areas are firm and yellow-white
• Micro
– Early
• active inflammatory phase
• Microabscesses - scattered follicles entirely disrupted and replaced by neutrophils
– Later
• aggregations of lymphocytes, histiocytes and plasma cells • Collapsed and damaged follicles
• multinucleate giant cells enclosing naked pools or fragments of colloid
⇒ "Granulomatous thyroiditis"
• chronic inflammatory infiltrate and fibrosis
– Different histologic stage in same gland, sometimes
The thyroid parenchyma contains a chronic inflammatory infiltrate with a multinucleate giant cell (above left) and a colloid follicle (bottom right).
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier
Clinical course of Subacute Granulomatous Thyroiditis
• Sudden or gradual
• Pain in neck
– radiating to upper neck, jaw, throat, or ears, particularly when swallowing
• Fever, fatigue, malaise, anorexia, myalgia
• Transient hyperthyroidism
– Disruption of thyroid follicles and release of excessive thyroid H.
– Usually diminishing in 2 to 6 weeks
• Self limited, recovery in 6 to 8 weeks
Subacute Lymphocytic (painless) Thyroiditis
• Uncommon cause of hyperthyroidism
• Painless or silent thyroiditis
• Most common in women during postpartum period
Æ “Postpartum thyroiditis”• Self-limited, last from 2 to 8 weeks before subsiding
• Autoimmune basis is suggested
– Some, elevated antibody to thyroglobulin and thyroid peroxidase
– Familial history of thyroid autoimmune disease
– Ocassionally, evolve into over chronic autoimmune thyroiditis – No evidence toward viral or other agent
Subacute Lymphocytic (painless) Thyroiditis
• Morphology
– Mild symmetric enlargement
– Normal appearance on gross inspection
– Lymphocytic infiltration with hyperplastic germinal
centers
– Patch disruption and collapse of thyroid follicles
– Fibrosis and Hurthle cell metaplasia are not
commonly seen. (cf, Hashimoto thyroiditis)
Graves disease
• Most common cause of primary
hyperthyroidism
• Triads of clinical findings
– Hyperthyroidism, hyperfunctional, diffuse
enlargement
– Infiltrative ophthalmopathy
Æ exophthalmos
– Localized, infiltrative dermopathy, called “pretibial
myxedema”
Graves disease
• Genetic factors
– HLA-B8, and -DR3
– Polymorphism in cytotoxic
T-lymphocyte-associated-4 (CTLA-4) gene
• Pathogenesis : autoimmune disease
– Thyroid stimulating immunoglobulin (TSI)
: central to disease pathogenesis– Thyroid growth-stimulating immunoglobulin (TGI)
– TSH-binding inhibitor immunoglobulin (TBII)
Morphology of Graves disease
<Gross>
– diffusely enlarged, smooth and soft
– cut section: soft, meaty appearance
Morphology of Graves disease
<Micro>
– too many cells and tall & more crowded
→ formation of small papillae (lack fibrovascular cores)
– colloid: pale, with scalloped margins
– lymphoid tissue ↑ in interfollicular stroma with
germinal center
Goiter (갑상샘종대)
• Enlargement of thyroid Å impaired synthesis
of thyroid hormone
– 주로 Dietary iodine deficiency
ÆImpairment of thyroid hormone synthesis Æ compensatory rise TSH
Æ casue hypertrophy and hyperplasia of thyroid follicular cells
Æ enlargement of thyroid gland Æ overcome hormone deficiency Æeuthryoid metabolic state
• Most common manifestation of thyroid
disease
Diffuse nontoxic (simple) goiter
• Enlargement of thyroid without nodularity
1) Endemic goiter
– low levels of iodine in soil, water, food – mountainous area (Himalaya, Andes) – decline by dietary iodine supplementation
– goitrogens : excessive calcium, vegetables (cabbage, cauliflower, turnips)
2) Sporadic goiter
– less common
– female, puberty or young adults
– ingestion of substances that interfere synthesis of thyroid hormone – hereditary enzymatic defects: autosomal recessive
Diffuse nontoxic (simple) goiter
◈ Morphology
1) Hyperplastic phase
– modestly enlarged and rarely exceeds 100 to 150gm – diffusely, symmetrically involved and markedly hyperemic – Crowded columnar follicular epithelium
– Accumulation ⇒ not uniform (distened and small)
2) Involution
Å ↑dietary iodine or ↓demand of thyroid H.
- follicle Æ enlarge filled with colloid ⇒ progressive flattening epithelium
⇒ “Colloid goiter”
Multinodular Goiter (다결절갑상샘종대)
• Recurrent epidsodes of hyperplasia and
involution
Æ more irregular enlargement of
thyroid
– long standing simple goiters ⇒ multinodular
goiters
• Nontoxic or
• induce thyrotoxicosis (toxic multinodular
goiter) “Plummer syndrome"
– no ophthalmopathy or dermopathy, less severe
hypermetabolism
Morphology of Multinodular Goiter
• more irregular enlargement (≥ 2000 gm) -- nodular
or multinodular goiter
• multilobulated, asymmetrically enlarged glands
• Cut surface
– irregular nodules, variable amounts of brown, gelatinous colloid, fibrosis, hemorrhage, calcification, cystic change
• Micro:
– colloid follicles, flattened inactive epithelium,
Nodular goiter. The gland is coarsely nodular and contains areas of fibrosis and cystic change.
Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 19 August 2006 07:17 AM) © 2005 Elsevier