Effects of Passive Shoulder-Lifting on the
Pain, Proprioception, and Range of Motion
in Neck Pain Patients With Scapular
Downward-Rotation Syndrome.
Sungmin Ha
The Graduate School
Effects of Passive Shoulder-Lifting on the
Pain, Proprioception, and Range of Motion
in Neck Pain Patients With Scapular
Downward-Rotation Syndrome
A Masters Thesis
Submitted to the Department of Rehabilitation Therapy
and the Graduate School of Yonsei University
in partial fulfillment of the
requirements for the degree of
Master of Science
Sungmin Ha
This certifies that the masters thesis of Sungmin Ha
is approved.
Thesis Supervisor: Ohyun Kwon
Chunghwi Yi
Hyeseon Jeon
The Graduate School
Yonsei University
Acknowledgements
First of all, I would like to take this opportunity to express my appreciation to Professor Ohyun Kwon, for his guidance and support. He is my primary director and mentor. He has introduced me to new things and has taught me to have a pioneering spirit and to think creatively. I would also like to express my deep gratitude to Professor Chung-hwi Yi, who gave me prudent advice and sincere encouragement, and will remain a good role model for me for the rest of my life. I sincerely appreciate to Professor Hyeseon Jeon, who gave me copious advice and encouragement throughout the study, and to Professor Sanghyun Cho and Seunghyun Yoo, who helped expand my knowledge and perspective.
I am also thankful all members of the KEMA, and especially Jonghyuck Weon, Yeonggil Jung, Heonseock Cynn, Taeho Kim, and Munhwan Kim. I am also grateful to my colleagues, Sujung Kim, Youngju Hong, and Kyuenam Park, and in particular my senior, Jaeseop Oh, who has been like a brother to me, always giving me intellectual support and guidance. Thank you also to Wonhwee Lee, who has been supportive, listened to my grumbling, and offered solutions to my many questions when needed, and to Mr. Byungkyu Lee for administrative support.
Finally, I would like to express my immense gratitude to my parents and sister. They have provided me with love and prayed to God for me every day. Thank you all.
Table of Contents
List of Figures ··· iii
List of Tables ··· iv Abstract ··· v Introduction ··· 1 Method ··· 5 1. Subjects ··· 5 2. Experimental Equipment ··· 6
2.1 3-D Motion Analysis System ··· 6
2.2 EMG-Biofeedback System ··· 6
2.3 Shoulder-Lifting Apparatus ··· 7
2.4 Visual Analogue Scale ··· 7
3. Experimental Procedure ··· 9
3.1 Neck Pain ··· 9
3.2 Joint Position Error ··· 10
3.3 Active Neck ROM ··· 11
4. Statistical Analysis ··· 12
Results ··· 13
3. Maximal Neck-Rotation ROM ··· 13
Discussion ··· 17
Conclusion ··· 21
References ··· 22
List of Figures
Figure 1. Shoulder-lifting apparatus ··· 8 Figure 2. Water-based horizontal level ··· 8 Figure 3. Two sets of ultrasound triple marker attachments ··· 10 Figure 4. Neck pain with and without passive shoulder-lifting maneuver ·· 15 Figure 5. Neck joint position error with and without passive shoulder
-lifting maneuver ··· 15 Figure 6. Maximal neck-rotation ROM with and without passive shoulder -lifting maneuver ··· 16
List of Tables
Table 1. General characteristics of the subjects ··· 5
Table 2. Comparison of neck pain ··· 14
Table 3. Comparison of neck joint position error ··· 14
ABSTRACT
Effects of Passive Shoulder-Lifting on the
Pain, Proprioception and Range of Motion
in Neck Pain Patients With Scapular
Downward-Rotation Syndrome
Sungmin Ha
Dept. of Rehabilitation Therapy (Physical Therapy Major) The Graduate School Yonsei University
The effects of the passive shoulder-lifting maneuver (PSLM) on pain, proprioception, and range of motion (ROM) were investigated in neck-pain patients with scapular
recruited from an industrial factory. They had no medical history of neurological or surgical problems. The intensity of pain felt was quantified using a visual analogue scale. Kinematic data for ROM and joint-position error (JPE) were analyzed using a 3D motion-analysis system. Differences in pain, JPE, and ROM with and without the PSLM were assessed using a paired t-test, and the level of statistical significance was set at p=0.05. The PSLM significantly decreased neck pain and JPE, and significantly increased neck ROM (p<0.05).
These findings suggest that the PSLM is an effective way of decreasing neck pain and improving neck ROM and proprioception during neck rotation in neck pain patients with SDRS.
Key Words: Neck pain, Scapular downward-rotation syndrome, Passive shoulder-lifting maneuver
Introduction
Scapular alignment is an indicator of possible change in muscle length and joint alignment, which needs to be corrected to allow optimal motion (Sahrmann 2002). Kendall, and McCreary (1993) described a standard for scapular alignment, specifying that the vertebral border of the scapula is parallel to the spine and is positioned approximately 3 inches from the midline of the thorax. The scapula is situated on the thorax between the second and seventh thoracic vertebrae; it lies flat against the thorax and rotates 30º anterior to the frontal plane.
A deviation from normal alignment suggests a muscle imbalance, which places abnormal strain on the musculoskeletal system (Braun 1991). Impairments outside the cervical region are of particular interest because some investigators have described how changes in alignment or movement in other regions have the potential to alter the biomechanics of the cervical-spine (Griegel-Morris et al. 1992; Szeto, Straker, and Raine 2002). Previous studies have suggested that scapular impairment is important, not only in the cervical region, but also in other areas when treating a patient with neck pain (Edmondston et al. 2007; May, and McKenzie 2002).
Impairments in alignment are believed to be correlated to specific movement-related diagnoses and provide clues on the resting length of muscles (Caldwell Sahrmann, and Van Dillen 2007). Scapular downward-rotation syndrome (SDRS) was first described by Sahrmann (2002). This syndrome classifies the type of impaired
movement presented in changing scapular alignment, though scapular downward-rotation. SDRS is revealed in a downwardly rotated scapular, with the inferior border being more medial than the superior border. It can result from short deltoid and supraspinatus muscles, an excessively long upper-trapezius muscle, or for shortened or stiff levator scapulae and rhomboid muscles. The shoulders are lower and slope downwardly at the acromial end, but can be higher at the base of the levator scapulae muscle, which is attached to the superior border of the scapula.
Scapular downward-rotation can contribute to prolonged compressive loading of the posterior cervical structures as a result of the transfer of the weight of the extremities to the cervical region through the attachments of the cervicoscapular muscles (upper trapezius and levator scapulae) (Van Dillen et al. 2007).An increased upper trapezius muscle length does not effectively transfer the weight of an upper extremity load to the sternoclavicular joint (Johnson et al. 1994). Furthermore, increased levator scapulae muscle stiffness occurs through loading and shear force on the neck structures during active neck movement (Szeto, Straker, and Raine 2002).Alterations in the biomechanics of the cervical region can produce local concentrations of high stress in the structure of the cervical spine (Adams et al. 2002). Repetitive stress in the cervical structure has the potential to cause cumulative microtrauma to tissue in the posterior cervical region (McDonnell, Sahrmann and Van Dillen 2005). Such stress might contribute to neck pain and a limited range of motion (ROM) (Van Dillen et al. 2007). Together with pain, a common feature of neck disorders is reduced ROM of the neck (Amstrong, McNair, and Williams. 2005; Sterling et al. 2003). In the
clinical setting, we have observed that patients typically stop moving when pain occurs (Van Dillen et al. 2007). The range of neck rotation in particular has been reported to be associated with a greater degree of disability than other types of neck motion (Olson et al. 2000).
Prolonged exposure to stress can impair proprioception-related muscle function (Jensen et al. 1993), which can further damage muscle spindles and decrease motor-unit output (Brockett et al. 1997). In this way, cervical compressive stress might inhibit the proprioceptive muscular feedback system (Adams et al. 2002; Corodo et al. 1995). According to studies by Sherrington and others, certain contemporary terms (i.e., sense of joint position, kinesthesia – perception of active and passive motion, and sense of tension or force) indicate submodalities of proprioception (Dover, and Powers 2003). Sensing the joint position is one of the most commonly used measures of proprioception (Voight et al. 1996). The determination of joint position involves measuring the accuracy of joint-angle replication, which can be conducted actively or passively in an open- or closed-chain environment (Riemann, and Lephart 2002). Abnormal joint-position error (JPE) has been detected with neck pain using either tests of ability to relocate the natural head posture after an active movement or to actively relocate a position within a movement plane (Loudon, Ruhl, and Field. 1997; Revel, Andre-Deshays, and Minguet 1991; Treleaven, Jull, and Stering 2003). These disturbances to posture control have been attributed to enhanced input from cervical afferents (Heikkilä, and Aström 1996). There is an abundance of receptors in the cervical muscles, and multiple cervical central and reflex connections to the vestibular,
visual, and postural control systems (Jull et al. 2007). The deep portions of the suboccipital muscles in particular have the highest cervical receptor density and are known to play a specific role in these reflex and central connections (Liu, Thornell, and Pedrosa-Domellof 2003).
In the current studies, modifying shoulder alignment is performed to reduce mechanical stress on the cervical spine in the clinical fields (McDonnell, Sahrmann and Van Dillen 2005). Several researchers have investigated the efficacy of shoulder alignment modification in neck-pain patients (McDonnell, Sahrmann and Van Dillen 2005; Szeto, Straker, and Raine 2002; Schuldt et al. 1987; Straker, and Raine 2002; Van Dillen et al. 2007). However, no studies have examined the effects of the passive shoulder-lifting maneuver (PSLM) on ROM, proprioception, and pain in neck pain patients with SDRS. Accordingly, in the present study the effects of the PSLM on ROM, proprioception, and pain were investigated in neck-pain patients with SDRS. We hypothesized that the PSLM would increase ROM and proprioception, and decrease pain in neck-pain patients with SDRS.
Methods
1. Subjects
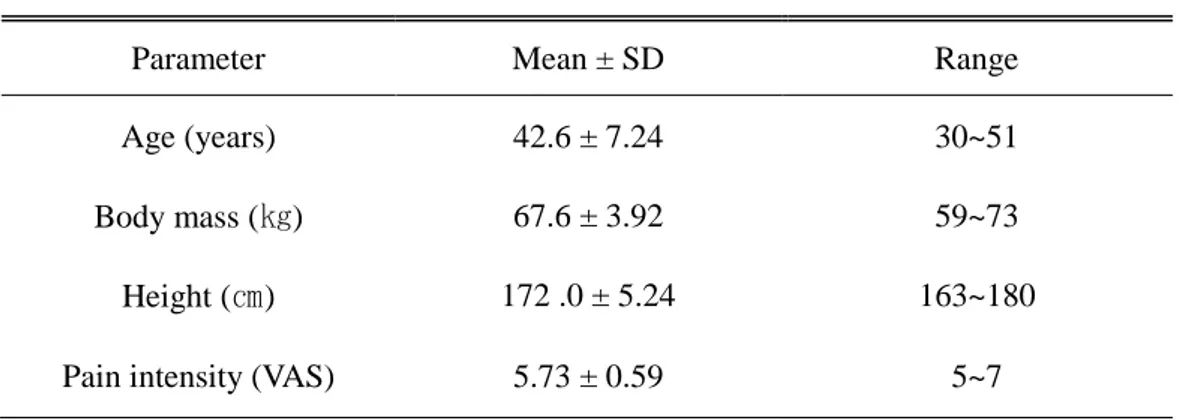
Fifteen male neck-pain patients with SDRS were recruited from an industrial factory. The following screening criteria were used for subject selection: (1) Scapulae downwardly rotated; inferior angle closer to spine than root of spine of scapulae; (2) Clavicle angle lower than normal; (3) Vertebral border of scapulae less than 3 inches from spine; (4) History of neck pain for at least 6 weeks; (5) Visual analogue scale (VAS) score more than 5. The exclusion criteria were no past or present spinal fracture and no history of unresolved cancer. The principal investigator explained all of the procedures to the subjects before the start of the study, and obtained their written informed consent to participate. The main characteristics of the subjects are presented in Table 1.
Table 1. Characteristics of the subjects. (N=15)
Parameter Mean ± SD Range
Age (years) 42.6 ± 7.24 30~51
Body mass (㎏) 67.6 ± 3.92 59~73
Height (㎝) 172 .0 ± 5.24 163~180 Pain intensity (VAS) 5.73 ± 0.59 5~7
2. Experimental Equipments
2.1 3-D Motion Analysis System
Three dimensional ultrasonic motion analysis system (CMS-HS, Zebris, Medizintechnik, Isny, Germany) was used to measure JPE, cervical ROM, and proprioception. Two sets of ultrasound triple markers, one mounted on a head attachment and another on a bar (reference marker), located over the head attachment, were arranged to detect the real-time cervical motion via three ultrasound transmitters. The transducer sensor stand comprised three integrated microphones that recorded the ultrasound signals. The angles measured were normalized to 0° relative to the starting or neutral head position (NHP). The sampling rate was 20 ㎐. The collected kinematics data were analyzed by Win-data software (ver.2.19, Zebris, Medizintechnik, Isny, Germany).
2.2 EMG-Biofeedback System
An EMG biofeedback system (T4000P, MyotracTM EMG Biofeedback System, Montreal, Quebec, Canada) was used to monitor voluntary upper-trapezius muscle activity during the PSLM. The sampling bandwidth was 20~500㎐. Electrode sites were prepared using skin abrasion and by cleaning the area with alcohol. The active surface electrode was aligned approximately parallel to the direction of the upper trapezius muscle fibers. The electrode sites were located on each side of the subject`s
(Cram, Kasman, and Holtz 1998) on the: upper trapezius, 2㎝ lateral to the midline drawn between the C7 spinous, and the posteriolateral acromion.
The threshold amplitude was selected in the resting position. This system provided real-time auditory feedback, with a threshold that could be set at a given muscle activity. When EMG activity exceeded a threshold, a tone was heard, which gave immediate feedback on excessive upper trapezius activity. If the tone was heard, re-test performed after a 2-minute rest period.
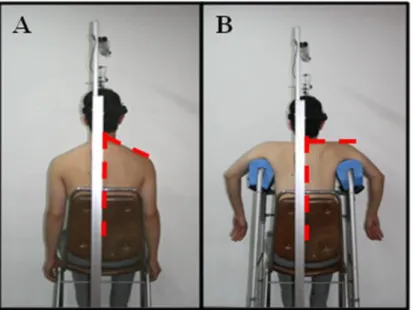
2.3 Shoulder-Lifting Apparatus
In previous studies, shoulder-lifting has been performed manually by the examiner; however, this method has the inherent problem of maintaining a constant shoulder position. We therefore used a shoulder-lifting apparatus, which consisted of a height-adjustable walker and shoulder supports that passively lift the shoulder so that they slope horizontally (Figure 1). To confirm a horizontal shoulder slope, a water-based horizontal level was attached to the shoulder slope (Figure 2). The patients were asked to relax their shoulder girdle muscles during the PSLM.
2.4 Visual analogue scale
Pain intensity was measured on visual analogue scale. The subject was asked to specify the amount of pain they experienced on scale of 0 (no pain) to 10 (the worst pain imaginable).
Figure 1. Shoulder-lifting apparatus.
(A: No passive scapular lifting maneuver, B: Passive scapular lifting maneuver)
3. Experimental procedures
3.1 Neck Pain
During maximal rotation of the neck, pain was measured with and without PSLM in the end-range. Subjects were asked to specify on the evaluation sheets how much pain they experienced, on a scale of 0 (no pain) to 10 (the worst pain imaginable).
3.2 Joint Position Error
JPE was calculated to test the accuracy of the subject’s sense of joint position. The subject’s position was identical to that used to test the active range of neck motion. The entire test procedure was divided into three parts: (1) determination of the neutral
head position (NHP), (2) determination of the target position, and (3) performance of head-to-target tests. The NHP was determined by asking the subject to maintain his head in a neutral position while sitting upright comfortably and looking ahead. The motion analysis system was recalibrated so that the NHP was defined as 0° for each
subject during each trial. The maximum ROM of cervical rotation was measured to determine the target position. The target position was defined as 65% of the maximum ROM of cervical rotation so as to avoid excessive stretching of the soft tissue of the neck. The subject’s head was moved passively until the predetermined target position was reached at a speed lower than 15°/s using a metronome. The speed
Figure 3. Two sets of ultrasound triple marker attachments.
(Goebel, Hanson, and Fishel 1994). Once the target position was established, the head-target repositioning test was performed. From NHP, the subject’s head was passively moved to the target position by the examiner. The subjects were permitted to concentrate on this position for 3-seconds, and then their head was passively moved back to NHP. After 3-seconds of rest, the subjects were asked to relocate to the target position once more. JPE was calculated as the difference between the target angle and the relocation target angle. The JPE values given were absolute values.
Subjects kept their eyes closed throughout the trial to eliminate the influence of visual inputs. They were permitted a 10-minute rest period between the two tests and the testing order was randomized to minimize learning carry-over effects.
3.3 Active Neck ROM
To measure the active range of neck movement, the subject was asked to sit upright on a chair with his feet on the floor and to look straight ahead. To prevent compensatory trunk movement, the subject`s trunk was fastened to the back of a chair using a Velcro strap as described by Wang, Tang, and Lin (2005). Two sets of ultrasound triple markers, one mounted on a head attachment and another on a bar, located over the head attachment, were arranged to detect real-time cervical movement via three ultrasound transmitters (Figure 3). Before each test, this motion was explained to the subject and demonstrated by the examiner. The subject performed actively the maximum neck rotation on his right and left side. The subject was then asked to keep his head in the maximal neck-rotation position for 3-seconds. The testing order was randomized.
4. Statistical Analysis
Data are expressed as mean and standard deviation values. The significance of the difference between the two conditions was assessed using a paired t-test with the level of statistical significance set at 0.05.
Results
1. Neck Pain
Neck-pain data are listed in Table 4 and shown in Figure 6. On both sides, neck pain decreased significantly when performing the PSLM.
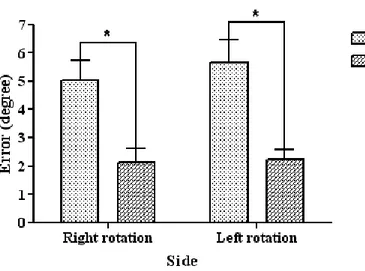
2. Neck Joint Position Error
JPE data are listed in Table 3 and shown in Figure 5. On the both sides, JPE decreased significantly when performing the PSLM.
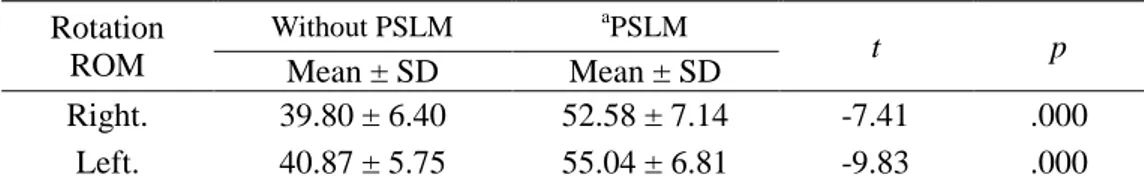
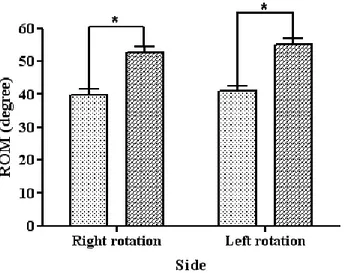
3. Maximal Neck-Rotation ROM
Neck-rotation ROM data are listed in Table 2 and shown in Figure 4. On both sides, neck-rotation ROM increased significantly when performing the PSLM.
Table 2. Comparison of neck pain (N=15)
aPSLM : passive shoulder-lifting maneuver.
Table 3. Comparison of neck joint position error (N=15)
aPSLM : passive shoulder-lifting maneuver. b
JPE: joint position error
Table 4. Comparison of maximal neck-rotation ROM (N=15)
a
PSLM : passive shoulder-lifting maneuver. Pain Without PSLM aPSLM t p Mean ± SD Mean ± SD Right. 6.47 ± 1.60 0.87 ± 0.74 16.71 .000 Left. 6.60± 0.99 1.00 ± 0.66 15.45 .000 b JPE Without PSLM aPSLM t p Mean ± SD Mean ± SD Right. 5.02 ± 2.71 2.11 ± 1.91 6.60 .000 Left. 5.65± 3.12 2.23 ± 1.34 6.23 .000 Rotation ROM Without PSLM aPSLM t p Mean ± SD Mean ± SD Right. 39.80 ± 6.40 52.58 ± 7.14 -7.41 .000 Left. 40.87 ± 5.75 55.04 ± 6.81 -9.83 .000
Figure 4. Neck pain with and without passive shoulder-lifting maneuver (PSLM).
Figure 5. Neck joint position error with and without passive shoulder-lifting maneuver (PSLM).
Figure 4. Maximal neck-rotation ROM with and without passive shoulder-lifting maneuver (PSLM).
Discussion
Scapular downward-rotation can contribute to prolonged compressive loading of the posterior cervical structures as a result of the transfer of the weight of the extremities to the cervical region through the attachments of the cervicoscapular muscles (upper trapezius and levator scapulae) (Van Dillen et al. 2007). To reduce mechanical stress on the cervical spine, modifying shoulder alignment currently is performed in the clinical field and researches (McDonnell, Sahrmann and Van Dillen 2005; Szeto, Straker, and Raine 2002; Schuldt et al. 1987; Straker, and Raine 2002; Van Dillen et al. 2007). However, no studies have examined the effects of the PSLM on pain, proprioception, and ROM in neck pain patients with SDRS. Accordingly, in the present study the effects of the PSLM on pain, proprioception, and ROM were investigated in neck-pain patients with SDRS. The study showed that the PSLM exerted a significant effect on pain, proproception, and maximal neck-rotation ROM. The PSLM significantly decreased neck pain and JPE, and significantly increased neck ROM (p<0.05).
In the present study, the PSLM resulted in a significant reduction in neck pain, possibly by reducing the load on the pain-sensitive structure on the cervical facet joint. The cervical facet joints have been documented as a source of nociception in the cervical structure (Bogduck, and Marsland 1988). Pain occurs because of a downward or asymmetric pull on the cervical vertebrae or facet by the levator scapulae muscle,
the upper trapezius muscle, and the weight of the upper extremity (Schuldt et al. 1987). The PSLM leads to changes in compressive loading by transferring the weight of the upper extremity to the sternoclavicular joint in neck-pain patients with SDRS during neck rotation.
Our results demonstrated that the PSLM significantly decreases JPE. Several possible mechanisms could explain this decrease. First, repositioning ability is determined primarily by the function of the muscle spindles of the contracting muscles (Gandevia, McCloskey, and Burke 1992). The PSLM might directly decrease extrinsic muscle participation and activate intrinsic muscles (deep suboccipital muscle) during neck rotation. Intrinsic muscles have a relatively high density of muscle spindles density (Kulkarni, Chandy, and Babu 2001), almost five times higher than that of the splenius capitis muscle and three times that of the semispinalis capitis muscle (Peck, Buxton, and Nitz 1984). These muscles are likely to play a primary role in signaling the cervical proprioceptive information involved in the conscious perception of equilibrium, position, and spatial orientation when vision is occluded (Rix, and Bagust 2001). These muscles also aid fine rotatory movement and maintain the stability of the neck (Peck, Buxton, and Nitz 1984). Although we did not measure intrinsic muscle activity directly by EMG, the activated intrinsic muscle contractions involved in the PSLM might improve muscle-spindle function, translating to a decrease in JPE. Second, the PSLM could decrease the stress placed on the joint and other structures of the cervical region. It has been suggested that abnormal joint stress affects the firing of cervical afferents, leading to changes in proprioceptive function.
Third, accurate control of movement is dependent on the sensory element of motor control system (Hodge, and Moseley 2003). Inaccurate afferent input would affect all aspects of motor control (Zedka et al. 1999). Especially, Pain leads to change in motor control (Ganevia, McCloskey, and Burke 1992). Numerous studies using experimental model of pain have provided support for this hypothesis (Arendt-Nielsen et al. 1996; Zedka et al. 1999). These include changes in excitability at the spinal or cortical level, change in proprioception (Hodge, and Moseley 2003). Widespread changes in excitability of nervous system have been identified at many levels of motor system during pain (Hodge, and Moseley 2003). Also, muscle spindle sensitivity and muscle activation are alerted by pain (Gandevia, McCloskey, and Burke 1992; Pedersen et al. 1997). Thus, these changes may adversely affect perception of movement. The PSLM resulted in a significant reduction in neck pain. Decreased pain may contributed improvement of proprioception during PSLM.
In present study the PSLM significantly increases the maximal neck-rotation ROM. Previous studies have found that modification of scapula positioning can increase the maximal neck-rotation ROM in neck-pain patients (Van Dillen et al. 2007). One explanation for the increase in ROM is a change in the muscle length of the cervicoscapular muscles during the PSLM, which would reduce the passive stretch in these muscles. This might reduce the loading and posterior shear on the neck structures (Gajdosik 2001). The PSLM could thus increase the maximal neck-rotation ROM by reducing passive limitations to rotation ROM resulting from the loss of extensibility of the upper trapezius and levator scapulae muscles.
This study was subject to some limitations. First, we focused only on neck rotation because rotation dysfunction is associated with greater disability than other neck motions (Olson et al. 2000). Second, we did not confirm the occurrence of intrinsic muscle activation, and hence further studies are warranted to assess intrinsic muscle activity. Third, our results cannot be generalized to other populations because all of the subjects who participated in the study were men (most industrial workers are male). Additional research is therefore needed to establish whether these findings also apply to female subjects.
Conclusion
The effects of the PSLM on pain intensity, proprioception, and ROM were investigated in neck-pain patients with SDRS. The PSLM significantly increased the maximum neck-rotation ROM and decreased JPE and neck pain. The PSLM could therefore be an effective method of decreasing neck pain and improving neck ROM and proprioception during neck rotation in these patients.
References
Adams MA, Bogduk N, Burton K, and Dolan P. The biomechanics of back pain, Edinburgh, Churchill Livingstone. 2002.
Amstrong BS, McNair, and Williams M. Head and neck position sense in whiplash patients and healthy individuals and the effect of the cranio-cervical flexion action.
Clin Biomech. 2005; 20:675-84.
Arendt-Nielsen L, Graven-Nielsen T, Svarrer H, and Svensson P. The influence of low back pain on muscle activity and coordination during gait: A clinical and experimental study. Pain. 1996;64:231-240.
Bogduck N, Marsland A. The cervical zygapophysial joints as a source of neck pain.
Spine. 1988;13:610-617.
Braun BL. Postural differences between asymptomatic men and women and craniofacial pain patients. Arch Phys Med Rehabil. 1991;72:653-656.
Brockett C, Warren N, Gregory JE, Morgan DL, and Proske U. A comparison of the effects of concentric versus eccentric exercise on force and position sense at the humeral elbow joint. Brain Res. 1997;771:251-258.
Caldwell C, Sahrmann S, and Van Dillen L. Use of a movement system impairment diagnosis for physical therapy in the management of a patient with shoulder pain. J
Orthop Sports Phys Ther. 2007;37:551-563.
Corodo P, Gurfinkel VS, Bevan L, and Kerr GK. Proprioceptive consequences of tendon vibration during movement. J Neurophysiol. 1995;74:1675-1688.
Cram J, Kasman G. and Holtz J. Introduction to surface electromyography. Gaithersburg, MD: Aspen. 1998
Dover G, and Powers ME. Reliability of joint position sense and force reproduction measures during internal and external rotation of the shoulder. J Athl Train. 2003;38:304-310.
Edmondston SJ, Chan HY, and Ngai GC, Warren ML, Williams JM, Glennon S, and Netto K. Postural neck pain: An investigation of habitual sitting posture, perception of 'good' posture and cervicothoracic kinaesthesia. Man Ther. 2007;12:363-371.
Gandevia SC, McCloskey DI, and Burke D. Kinaesthetic signals and muscle contraction. Trends Neurosci. 1992;15:62-65.
Gajdosik RL. Passive extensibility of skeletal muscle: Review of the literature with clinical implication. Clin Biomech. 2001;16:87-101.
Goebel JA, Hanson JM, and Fishel DG. Age-related modulation of the vestibule-ocular reflex using real and imaginary targets. J Vestib Res. 1994;4:269-275.
Griegel-Morris P, Larson K, Muller-Klaus K, and Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther. 1992;72:425-431.
Heikkilä H, and Aström PG. Cervicocephalic kinesthetic sensibility in patients with whiplash injury. Scand J Rehabil Med. 1996;28:133-138.
Hodges PW, and Moseley GL. Pain and motor control of the lumbopelvic region: Effect and possible mechanisms. J Electromyogr Kinesiol. 2003;13:361-370.
Jensen C, Finsen L, Sogaard K, and Christensen H. Musculoskeletal symptoms and duration of computer and mouse use. Int J Ind Ergon. 2002;30:265-275.
Johnson G, Bogduk N, Nowitzke A, and House D. Anatomy and actions of the trapezius muscle. Clin Biomech. 1994;9:44-50.
Jull G, Falla D, Treleaven J, Hodges P, and Vicenzino B. Retraining cervical joint position sense: The effect of two exercise regimes. J Orthop Res. 2007;25:404-412.
Kendall FP, McCreary EP, and Provance PG. Muscles: testing and function. 4th ed. Baltimore: Williams & Wilkins. 1993.
Kulkarni V, Chandy MJ, Babu KS. Quantitative study of muscle spindles in suboccipital muscles of human foetuses. Neurol India. 2001;49:355-359.
Liu J, Thornell L, Pedrosa-Domellof F. Muscle spindle in the deep muscles of the human neck: A morphological and immunocytochemical study. J Histochem
Cytochem. 2003;51:175-186.
Loudon JK, Ruhl M, Field E. Ability to reproduce head position after whiplash injury.
May S, and Mckenzie RA. Mechanical diagnosis and therapy for the cervical and thoracic spine. In: Grant R, ed. Physical therapy of the cervical and thoracic spine. 3rd ed. London: Churchill Livingstone. 2002.
McDonnell MK, Sahrmann SA, and Van Dillen L. A specific exercise program and modification of postural alignment for treatment of cervicogenic headache: A case report. J Orthop Sports Phys Ther. 2005;35:3-15.
Olson SL, O'Connor DP, Birmingham G, Broman P, and Herrera L. Tender point sensitivity, range of motion, and perceived disability in subjects with neck pain. J
Orthop Sports Phys Ther. 2000;30:13-20.
Peck D, Buxton DF, and Nitz A. A comparison of spindle concentrations in large and small muscles acting in parallel combinations. J Morphol. 1984;180:243-252.
Pedersen J, Sjölander P, Wenngren BI, and Johansson H. Increased intramuscular concentration of bradykinin increases the static fusimotor drive to muscle spindles in neck muscles of the cat.
Revel M, Andre-Deshays C, and Minguet M. Cervicocephalic kinesthetic sensibility in patients with cervical pain. Arch Phys Med Rehab. 1991;72:288-291.
Riemann BL, and Lephart SM. The Sensorimotor System, Part I: The Physiologic Basis of Functional Joint Stability. J Athl Train. 2002;37:71-79.
Rix GD, and Bagust J. Cervicocephalic kinesthetic sensibility in patients with chronic, nontraumatic cervical spine pain. Arch Phys Med Rehab. 2001;82:911-999.
Sahrmann S. Diagnosis and treatment of movement impairment syndromes. St. Louis, Mosby. 2002.
Schuldt K, Ekholm J, Harms-ringdahl Nementh G, and Arborelius UP. Effects of arm support or suspension on neck and shoulder muscle activity during sedentary work.
Scand J Rehabil Med. 1987;19:77-84.
Sterling M, Jull G, Vincenzino B, and Darnell R. Development of motor system dysfunction following whiplash injury. Pain. 2003;103:65-73.
Szeto GP, Straker L, and Raine S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl Ergon. 2002;33:75-84.
Treleaven J, Jull G, and Stering M. Dizziness and unsteadiness following whiplash injury: Characteristics features and relationship with cervical joint position error. J
Van Dillen LR, McDonell MK, Susco TM, and Sahrmann SA. The immediate effect of passive scapular elevation on symptoms with active neck rotation in patients with neck pain. Clin J Pain. 2007;23:641-647.
Voight ML, Hardin JA, Blackburn TA, Tippett S, and Canner GC. The effects of muscle fatigue on and the relationship of arm dominance to shoulder proprioception. J Orthop Sports Phys Ther. 1996;23:348-352.
Wang SF, Tang CC, and Lin KH. Measurement of cervical range of motion pattern during cyclic neck movement by ultrasound-based motion system. Man Ther. 2005;10:68-72.
Zedka M, Prochazka A, Knight B, Gillard D, and Gauthier M.. Voluntary and reflex control of human back muscles during induced pain. J Physiol. 1999;15:591-604.
국문 요약
견갑골 하방회전 증후군을 가진 경부 통증 환자에게
수동적 어깨 거상이 경추의 통증과 고유수용성 감각,
관절 가동범위에 미치는 영향
연세대학교 대학원
재활학과(물리치료학 전공)
하 성 민
본 연구에서는 견갑골 하방회전 증후군을 가지고 있는 경부 통증 환자들 에게 수동적 어깨 거상을 시행했을 때, 경추의 관절 가동범위, 고유수용성 감각 및 통증에 어떠한 영향을 미치는지 알아보았다. 연구대상자는 산업체 에서 근무하는 근로자들 중에 견갑골 하방회전 증후군을 가지고 있는 경부 통증 호소자 15명을 선정하였다. 관절가동 범위와 관절 위치 재현 검사는 3차원 동작 분석 장비를 이용하였다. 그리고 통증은 통증 상사 척도를 이 용하여 측정하였다. 두 조건의 유의한 차이를 비교하기 위해 짝-검정을실시하였고, 유의수준은 0.05로 하였다. 연구결과 수동적 어깨 거상은 관 절 위치 재현 오류와 통증을 유의하게 감소시켰으며 경추의 관절 가동범위 는 유의하게 증가됨을 알 수 있었다. 이러한 결과들은 견갑골 하방회전 증 후군을 가진 경부통증 환자에게 수동적 어깨 거상이 경부통증을 감소시키 고 관절 가동범위와 고유수용성 감각을 증진시키는데 효과적이라 할 수 있 겠다. 핵심 되는 말: 견갑골 하방회전 증후군, 경부 통증, 수동적 어깨 거상.