Received:October 3, 2016, Revised:January 2, 2017, Accepted:March 16, 2017
Corresponding to:Jin-Su Park, Division of Rheumatology, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, 100, Ilsan-ro, Ilsandong-gu, Goyang 10444, Korea. E-mail:jinsulog@naver.com
Copyright ⓒ 2017 by The Korean College of Rheumatology. All rights reserved.
This is a Open Access article, which permits unrestricted non-commerical use, distribution, and reproduction in any medium, provided the original work is properly cited.
A Case of Polymyositis Associated with Immunoglobulin A Nephropathy
Yoon-Jeong Oh1, Eun Sung Park1, Mi Jang2, Ea Wha Kang3, Jeong-Hae Kie4, Sang-Won Lee1, Jason Jungsik Song1, Yong-Beom Park1, Chan-Hee Lee5, Jin-Su Park5
1Division of Rheumatology, Department of Internal Medicine, Yonsei University College of Medicine, 2Department of Pathology, Yonsei University College of Medicine, Seoul, 3Division of Nephrology, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, 4Department of Pathology, National Health Insurance Service Ilsan Hospital, 5Division of Rheumatology, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
Polymyositis (PM) is a chronic inflammatory disease that predominantly affects muscles. Systemic organ involvement, includ- ing the respiratory and gastrointestinal tracts, is frequently observed in PM, but renal involvement is rare. Herein, we report the case of a 56-year-old woman presenting with weight gain, edema, and generalized myalgia. Laboratory tests revealed elevated creatinine kinase level, hypoalbuminemia, and proteinuria. Histopathological examination of muscle biopsy revealed in- flammatory myositis, and a renal biopsy confirmed immunoglobulin A (IgA) nephropathy. Based on the clinico-pathological re- sults, the patient was diagnosed with PM with IgA nephropathy. This is a report of a rare occurrence of IgA nephropathy in a patient with PM presenting with chronic glomerulonephritis. (J Rheum Dis 2017;24:241-245)
Key Words. Polymyositis, IgA nephropathy, Proteinuria
INTRODUCTION
Polymyositis (PM) is a chronic autoimmune inflam- matory disease with a progressive course mostly involv- ing muscles. It is characterized by symmetrical proximal muscle weakness, elevation of muscle-enzymes’ levels, characteristic electromyographic (EMG) features, and specific histopathological findings in a muscle biopsy specimen. Systemic organ involvement, including the respiratory and gastrointestinal tracts, is frequently ob- served in PM, but renal involvement in patients with idio- pathic inflammatory myopathies is rare. We report the case of a patient with PM, who was diagnosed with im- munoglobulin A (IgA) nephropathy while being eval- uated for the cause of persistent proteinuria. To our knowledge, this is the first case to be reported in Korea and the second in the world.
CASE REPORT
A 56-year-old woman was admitted for a 1-month his- tory of pruritus, weight gain (3 kg over a month), general- ized myalgia, anorexia, and Raynaud’s phenomenon.
Typical skin lesions were absent. Physical examination showed grade II bilateral pretibial pitting edema and grade IV muscle strength in the proximal muscles of all limbs.
Laboratory test results with their corresponding refer- ence ranges were as follows: serum creatine kinase (CK), 8,493 (26∼140 IU/L); lactate dehydrogenase, 653 (98∼
192 IU/L); aldolase, 90.1 (<7.6 U/L); aspartate amino- transferase, 246 (0∼37 IU/L); alanine aminotransferase, 190 (0∼48 IU/L); C-reactive protein, 5.30 (<1.00 mg/dL); erythrocyte sedimentation rate, 62 (<20 mm/hr); serum albumin, 2.5 (3.5∼4.8 g/dL); and serum creatinine, 0.8 (0.4∼1.0 mg/dL). Urinalysis revealed 2+
protein, 2+ red blood cells, spot urine protein-to-crea-
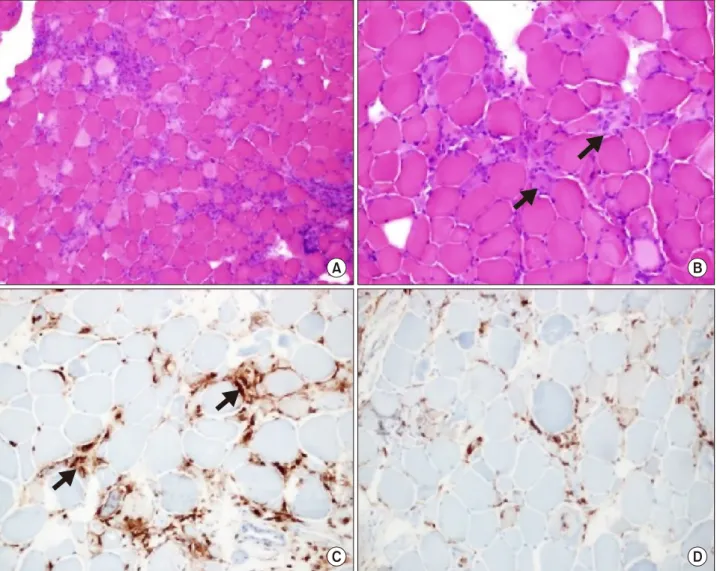
Figure 1. Muscle biopsy. (A) Light microgram of a muscle biopsy specimen (H&E, ×40). (B) Light microgram showing in- flammatory cell infiltrates (black arrows) scattered throughout the endomysium, invading individual muscle fibers (H&E, ×200).
(C) On immunohistochemistry, the inflammatory cells express leukocyte common antigen (black arrows) (Immunohistochemistry,
×200). (D) Anti CD 68 staining of the muscle biopsy specimen (Immunohistochemistry, ×200).
tinine ratio (PCR) of 2,066.9 mg/g and urine albu- min-to-creatinine ratio (ACR) of 81.1 mg/g. Anti Jo-1, anti-double stranded DNA, anti-ribonucleoprotein, anti SS-A(Ro), anti SS-B(La), anti-histone, anti-smith, an- ti-cardiolipin IgM/IgG, and anti-beta 2 glycoprotein IgM/IgG antibodies were all absent, except for anti- nuclear antibody (1:320 positive, speckled pattern).
Serum complement and immunoglobulin G, A, and M levels were within normal limits.
EMG showed low amplitude polyphasic motor poten- tials of short duration in the upper and lower proximal muscles. Examination of the biopsy specimen from the left vastus lateralis revealed myopathic changes asso- ciated with inflammatory cell infiltrates (Figure 1), and immunofluorescence of the renal biopsy showed diffuse
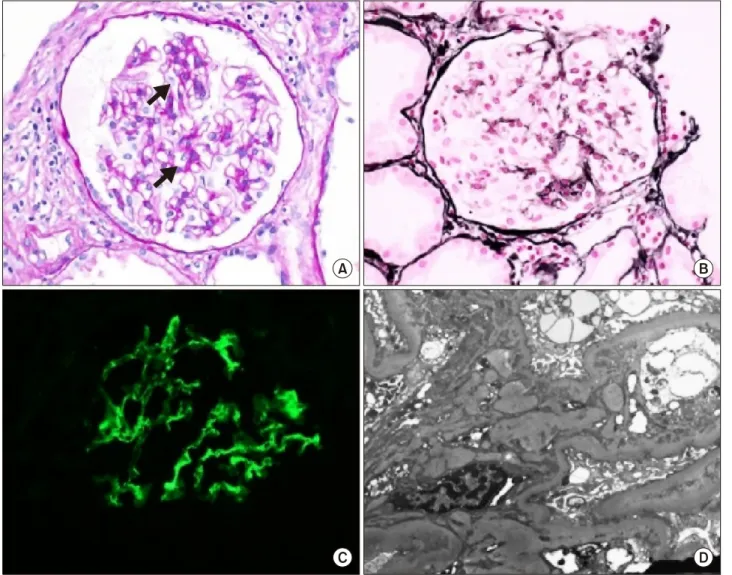
deposition of IgA in the mesangium, suggestive of IgA nephropathy (Figure 2).
The following biochemical parameters were elevated:
CK, up to 11,312 IU/L; serum aldolase, up to 104.6 U/L;
spot urine PCR, up to 4,345.5 mg/g and spot urine ACR, up to 350.7 mg/g. Administration of 60 mg oral pre- dnisolone daily was initiated under the presumptive diag- nosis of PM, according to the criteria of Bohan and Peter [1]. However, the severity of proximal muscle weakness was aggravated from grade IV to II. Muscle weakness de- teriorated despite administrating methylprednisolone (3 doses of 1 g daily each) and cyclophosphamide pulse therapies. Intravenous immunoglobulin was administered at a dose of 2 g/kg for 5 days. Thereafter, the patient’s proximal muscle strength gradually improved from grade
Figure 2. Renal biopsy. (A) Light microgram showing mild mesangial expansion (black arrows) without cellular proliferation (Periodic acid Schiff, ×400). (B) Some glomeruli showed segmental sclerotic change and synechia with Bowman’s capsule (PAS-silver stain, ×400). (C) Immunofluorescence staining revealed moderate positivity for IgA on the mesangium and para- mesangium (Immunofluorescence staining, ×400). (D) Electron microgram demonstrating deposits in the mesangium and para- mesangium (Uranyl acetate, ×6,000).
II to IV and the CK level decreased to 780 IU/L.
Malignancy workup to identify the cause of the rapid ag- gravation of PM revealed a 1.1 cm thyroid papillary carci- noma for which the patient underwent total thyroidectomy.
CK level and PCR rapidly decreased to <300 IU/L and
<60.1 mg/g, respectively, after surgery. The patient was maintained on oral prednisolone therapy. Up to 6 months after total thyroidectomy, disease activity of PM was well controlled and microscopic hematuria/proteinuria was not observed, even with low dose steroids alone.
DISCUSSION
PM not only affects muscles but also involves systemic
organs. However, unlike respiratory and gastrointestinal tract involvement, renal involvement is infrequent in PM in comparison to other autoimmune diseases [2,3]. Acute kidney injury secondary to rhabdomyolysis and PM-asso- ciated glomerulonephritis are reported as the 2 chief renal signs of PM [4,5]. Otherwise, PM-associated IgA nephr- opathy is relatively uncommon.
The histopathological features of PM include myofiber injury caused by macrophages and activated CD8+ cyto- toxic T cells that attack non-necrotic muscle fibers ex- pressing class I major histocompatibility complex (MHC-I) [6-8]. Patients with IgA nephropathy are reported to be relatively deficient in suppressor T-cell activity and to have hyperactive IgA-specific helper T-cell [9]. Although
cellular immunity is the main player in PM, humoral im- munity may also be involved via the production of IgG that reacts with IgA, causing IgA nephropathy. The patho- physiological mechanisms linking IgA nephropathy to PM remain unknown [10].
IgA nephropathy is a primary glomerulonephritis charac- terized by IgA deposition in the glomerular mesangia Most patients with IgA nephropathy have primary disease, but a secondary form is frequently reported with liver dis- ease, inflammatory bowel disease and connective tissue disorders [11]. Very little is known about the incidence of secondary IgA nephropathy compared to that of primary IgA nephropathy. Moreover, the specific interrelations be- tween autoimmune status, regulation of IgA synthesis, and development of IgA nephropathy remain uncertain.
The lack of renal biopsy result after improvement of the underlying autoimmune disease, due to the patient’s re- fusal to repeat it, was a limitation in this report. Deter- mining whether the cause was primary or secondary to other diseases such as autoimmune disease was very challenging. Moreover, a repeat renal biopsy would not discriminate between primary and secondary IgA neph- ropathy. Although our patient showed hypoalbuminemia with nephrotic range proteinuria and was diagnosed with IgA nephropathy, the proteinuria might have been of non-glomerular origin because urinary albumin to total protein concentration ratio was ˂0.4. Since most patients with IgA nephropathy have isolated hematuria or hema- turia with glomerular proteinuria, the non-glomerular proteinuria in this case suggests secondary IgA nephrop- athy, or incidental IgA nephropathy combined with PM.
Furthermore, the decrease in CK level and resolution of hematuria after treatment of PM indicate the secondary nature of IgA nephropathy.
Our patient was found to have thyroid cancer shortly af- ter being diagnosed with PM. The relationship between inflammatory myopathy and malignancy has been well known since PM associated with stomach cancer was first report by Stertz in 1916 [12]. Further studies suggest that cancer and myositis have common autoantigens such as Mi-2, HRS, DNA-PKc [13]. However, the presence of these antibodies was not checked in this patient because most of them are not used clinically. Based on the timing of muscle weakness onset, worsening pattern of PM de- spite methylprednisolone pulse therapy, and dramatic de- crease in disease activity after total thyroidectomy [13], PM in this case was more likely to be a paraneoplastic syn- drome secondary to thyroid cancer.
To the best of our knowledge, this is the first case of idio- pathic inflammatory myopathy, particularly PM, diag- nosed with IgA nephropathy to be reported in Korea, and the second worldwide [14].
SUMMARY
Renal involvement makes the poor prognosis in many autoimmune diseases. Renal biopsy is important for diag- nosis in patients with worsening renal function or in- creasing proteinuria. Our findings suggest that IgA nephropathy secondary to PM may cause proteinuria;
therefore, renal biopsy should be considered in patients with myositis presenting with proteinuria.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts). N Engl J Med 1975;292:344-7.
2. Takizawa Y, Kanda H, Sato K, Kawahata K, Yamaguchi A, Uozaki H, et al. Polymyositis associated with focal me- sangial proliferative glomerulonephritis with depositions of immune complexes. Clin Rheumatol 2007;26:792-6.
3. Cucchiari D, Angelini C. Renal involvement in idiopathic inflammatory myopathies. Clin Rev Allergy Immunol 2017;52:99-107.
4. Wu Y, Chhaya S, Hurowitz B, Ardiles T, Carlson R. Clini- cally amyopathic dermatomyositis complicated by pleural effusion case report, literature review, and proposed mechanism. Bull Hosp Jt Dis (2013) 2015;73:217-20.
5. Qian Y, Ren H, Zhang W, Chen N. Clinical features of poly- myositis and dermatomyositis in four patients with renal in- volvement as mainly presentation. Zhonghua Nei Ke Za Zhi 2009;48:930-2.
6. Nickavar A, Mehr Azma M. Nephrotic syndrome and juve- nile dermatomyositis. Rheumatol Int 2012;32:2933-5.
7. Findlay AR, Goyal NA, Mozaffar T. An overview of poly- myositis and dermatomyositis. Muscle Nerve 2015;51:638-56.
8. Couvrat-Desvergnes G, Masseau A, Benveniste O, Bruel A, Hervier B, Mussini JM, et al. The spectrum of renal involve- ment in patients with inflammatory myopathies. Medicine (Baltimore) 2014;93:33-41.
9. Shin DH, Lim BJ, Han IM, Han SG, Kwon YE, Park KS, et al.
Glomerular IgG deposition predicts renal outcome in pa- tients with IgA nephropathy. Mod Pathol 2016;29:743-52.
10. Civilibal M, Selcuk Duru N, Ozagari A, Durali K, Elevli M.
Immunoglobulin A nephropathy associated with juvenile dermatomyositis. Pediatr Nephrol 2009;24:2073-5.
11. Pouria S, Barratt J. Secondary IgA nephropathy. Semin Nephrol 2008;28:27-37.
12. Stertz G. Polymyositis. Berl Klin Wochenschr 1916;53:489.
13. Levine SM. Cancer and myositis: new insights into an old association. Curr Opin Rheumatol 2006;18:620-4.
14. Barros TB, de Souza FH, Malheiros DM, Levy-Neto M, Shinjo SK. IgA nephropathy and polymyositis: a rare association. Rev Bras Reumatol 2014;54:231-3.