J Korean Soc Radiol 2017;76(2):104-110 https://doi.org/10.3348/jksr.2017.76.2.104
INTRODUCTION
Uterine vascular malformation (UVM) is a tangle of abnormal arteriovenous connections located in or around the uterus (1).
UVM can be congenital or acquired, and in 1−2% of cases, mas- sive vaginal bleeding or intraperitoneal hemorrhage can occur, which can be life-threatening (2, 3). These complications may occur as late postpartum or post-abortion hemorrhages, result- ing from spontaneous vessel rupture or traumatic rupture trig- gered by dilatation and curettage (D & C).
The major cause of acquired UVM is usually traumatic, and it is caused by prior D & C, direct uterine trauma, or previous uter-
ine surgery. Sometimes, it originates from endometrial carcino- ma, cervical carcinoma, and gestational trophoblastic disease (GTD).
The preferred noninvasive method for diagnosing UVM is color Doppler ultrasound. Ultrasonographic diagnosis is based on the presence of hypoechoic, tortuous spaces in the myometri- um, demonstrating a low impedance and high velocity flow upon color Doppler examination (4). Computed tomography (CT) and magnetic resonance imaging (MRI) may be used to deter- mine the size, extent, vascularity, and involvement of the adjacent organs.
Traditionally, UVMs have been treated by uterine artery liga-
Acquired Uterine Vascular Malformation: Clinical Outcome of Transarterial Embolization
후천성 자궁 혈관 기형: 경피적 경동맥 색전술의 임상적 결과
Chae Hoon Kang, MD
1, Seung Boo Yang, MD
2*, Dong Erk Goo, MD
2, Yong Jae Kim, MD
2, Jae Myung Lee, MD
2, Woong Hee Lee, MD
21Department of Radiology, Gangneung Asan Hospital, Gangneung, Korea
2Department of Radiology, Soonchunhyang University Gumi Hospital, Gumi, Korea
Purpose: To evaluate clinical outcomes of transarterial embolization of bilateral uterine arteries (UAE) in patients with acquired uterine vascular malformation (UVM).
Materials and Methods: This retrospective study was performed on the medical records of all 19 patients who underwent transarterial embolization of bilateral UAE for the treatment of symptomatic UVMs from January 2003 to June 2011. Emboli- zation was performed via the unilateral femoral artery approach with a catheter and angiographic techniques. Clinical success was defined as definitive resolution of abnormal vaginal bleeding. Post-procedural complications included all adverse events related to the embolization procedure.
Results: A total of 20 procedures were performed in 19 patients. One patient re- quired repeat embolization because of incomplete embolization related to promi- nent high flow malformation. Clinically, in all patients, bleeding was controlled im- mediately after embolization. No complications occurred in all patients during the follow up period. In all patients who underwent successful UAE, menstrual cycles were normally restored within 1–2 months. Normal pregnancy with term delivery was observed in two of the 19 cases.
Conclusion: Transarterial bilateral UAE is a safe and effective treatment in patients with vaginal bleeding caused by acquired UVM, and it allows the possibility of fu- ture pregnancy.
Index terms Uterus
Arteriovenous Malformation Angiography
Embolization Therapeutic
Received August 17, 2016 Revised August 25, 2016 Accepted August 28, 2016
*Corresponding author: Seung Boo Yang, MD Department of Radiology, Soonchunhyang University Gumi Hospital, 179 1gongdan-ro, Gumi 39371, Korea.
Tel. 82-54-468-9391 Fax. 82-54-464-9300 E-mail: ysbysb@sch.ac.kr
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distri- bution, and reproduction in any medium, provided the original work is properly cited.
tion or hysterectomy. Currently, arterial embolization is the pre- ferred treatment because it is minimally invasive and has the po- tential to preserve fertility.
The purpose of our study is to describe our experience in using transarterial bilateral uterine arteries (UAE) in patients with ac- quired UVM, and to evaluate the long term clinical outcomes.
MATERIALS AND METHODS
From January 2003 to June 2011, a total of 19 patients (mean age: 30.8 years, range: 22−44 years) underwent bilateral UAE for the treatment of a symptomatic UVM. The medical records of all 19 patients were retrospectively reviewed. This study received ap- proval from Soonchunhyang University’s institutional Review Board.
All but one patient underwent a single embolization session.
All 19 patients initially presented with vaginal bleeding. The re- cent obstetrical history prior to embolization revealed a history of D & C after missed abortion (n = 12), cesarean section (n = 5), normal vaginal delivery (n = 1), and ectopic pregnancy (n = 1).
All patients underwent abdominal and transvaginal ultra- sound examinations or CT or MRI before embolization. Emboli- zation was performed using the unilateral femoral artery ap- proach with a catheter and angiographic techniques. After in- sertion of a 5-French introducer sheath (Terumo, Tokyo, Japan), bilateral UAE were catheterized using a 5-French Cobra catheter (Cook Medical, Bloomington, IN, USA) under local anesthesia.
Depending on the vascular anatomic findings during angiogra- phy, decisions were made regarding whether or not to use an ad- ditional 2.7-French microcatheter (Progreat; Terumo) to cathe- terize the feeding uterine artery. Bilateral UAE was performed using gelatin sponge particles made from gelatin sponge sheets (Gelfoam; Upjohn, Kalamazoo, MI, USA) and/or additional mi- crocoils (Tornado; Cook Medical).
Angiographic success was defined as successful embolization of the vascular malformation with stasis of blood flow in the main feeding uterine artery and no residual opacification of the UVM. Ultrasonographic success was defined as eradication of the UVM and restoration of normal uterine vasculature. Clinical success was defined as definitive resolution of abnormal vaginal bleeding. Post-procedural complications included all adverse events related to the embolization procedure.
The medical records were reviewed with respect to post-pro- cedural complications, recurrence of vaginal bleeding, menstrual cycle, pregnancy or delivery.
RESULTS
Angiographic success was achieved in all 19 patients. One pa- tient required repeat embolization since the UVM was not com- pletely embolized due to prominent high flow in the first session.
Therefore, a total of 20 procedures were performed in 19 patients.
Angiography revealed the presence of a pseudoaneurysm dur- ing five procedures (25%) (Fig. 1). During the remaining 15 pro- cedures (75%), hypertrophied main UAE with hypervascular mass-like lesions and early draining into a large pelvic vein were opacified. No direct arteriovenous communication was demon- strated (Fig. 2). During all procedures, no contrast extravasation into the uterine cavity was depicted. The embolic agents used in all embolization sessions were gelatin sponge particles, along with additional microcoils during three procedures due to high flow. On completion angiography, no evidence of non-target em- bolization or vessel wall damage in the uterine or internal iliac artery was noted.
Duplex ultrasound evaluation performed three days after em- bolization showed ultrasonographic success in all patients.
The mean clinical follow-up period was 20 months, and it ranged from 1 to 42 months. Vaginal bleeding was controlled im- mediately after embolization in all patients, and none of the pa- tients reported any clinical symptoms associated with UVM dur- ing the follow-up period. Minor adverse events consisting of post-embolization pelvic pain were noted in three patients within a week of the procedure. All patients were treated conservatively by intramuscular or intravenous administration of 100 mg tram- adol HCL daily (Tradol; Bugwang, Seoul, Korea) for 3−7 days.
All patients had complete resolution of their pain within a week.
Recovery of their normal menstrual cycle was seen in all 19 patients. Among these 19 patients, two patients achieved full- term intrauterine pregnancy with uneventful labor. In these cas- es, the mean time period between embolization and delivery was 20.1 months.
DISCUSSION
Vascular malformation can occur in any part of the body, in- cluding the female pelvis. Mulliken and Glowacki (5) proposed the classification of vascular malformation based on their flow characteristics (fast flow or slow flow), and their vascular channel components (capillary, venous, lymphatic, arterial and com- bined). UVM, a type of fast flow malformation, can affect the pelvic structures such as the pelvic wall, the visceral organs, or both (6, 7). It can form congenitally or can be caused by other secondary causes, and it can be difficult to differentiate between these causes depending on the patient’s history. Congenital UVM arises from abnormal embryologic development of the primitive vascular structure, and it results from multiple abnormal arterio- venous communications. It contains multiple arterial feeders and venous drainage channels, and an intervening nidus (8-11). Ac- quired UVMs are more common than primary UVMs, and their growth is typically stimulated by trauma such as D & C, or hor-
monal changes that occur during puberty or pregnancy (12).
They can also be associated with malignancies such as endome- trial carcinoma or GTD.
Compared with congenital UVMs, acquired UVMs tend to have single or bilateral feeding UAE without an extrauterine ar- tery supply, and do not have a nidus (8). UVMs typically evolve over time, from an asymptomatic lesion to a lesion with active shunting, venous engorgement or hypertension. If they rupture, UVMs can cause life-threatening bleeding; hence, prompt diag- nosis and treatment are important.
Currently, the diagnostic modalities available for UVM are ul- trasonography (US) and MRI. Color and duplex Doppler US are especially good screening and diagnostic methods (6, 9, 13). The most common Gray-Scale ultrasonographic feature of UVM is the anechoic tubular space in the myometrium without a mass effect, but this feature is nonspecific; hence, the diagnosis of AVM is not based on Gray-Scale ultrasonographic morphology.
On color Doppler US, a tangle of tortuous vessels with multidi-
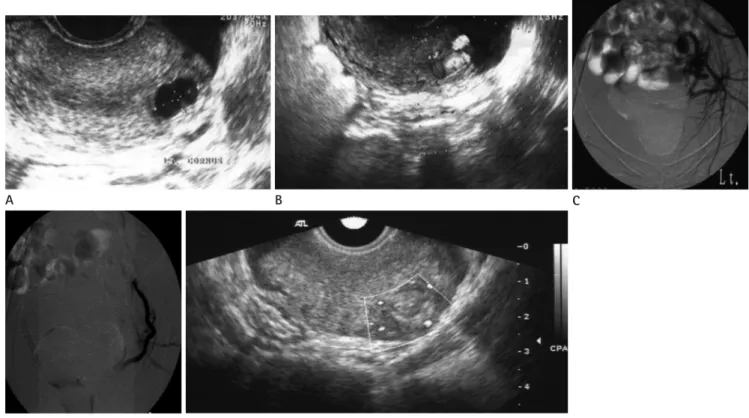
Fig. 1. A 27-year-old woman presented with vaginal bleeding for 2 months after D & E.
Gray-Scale ultrasonogram (A) shows a cystic mass in the uterus. Color Doppler ultrasonogram (B) reveals a pseudoaneurysm. Selective left uter- ine angiogram (C) shows a pseudoaneurysm in the uterus. Completion uterine angiogram (D) after uterine artery embolization with gelatin sponge particles reveals the disappearance of pseudoaneurysm with occlusion of the uterine artery. Color Doppler ultrasonogram (E) obtained two days after embolization reveals complete thrombosis of the pseudoaneurysm.
A
E
B C
D
rectional, high-velocity arterial flow with an asymmetric distri- bution is observed. Duplex Doppler US examination shows the features of arteriovenous shunting, like fast arterial flow with low resistance (8, 9). MR angiography, performed as a time-resolved contrast-enhanced three-dimensional acquisition, can be useful in evaluating the extent of the lesion and the vascular anatomy around this anomaly. Furthermore, 3D-reconstruction of the vascular structures with elimination of overlapping vessels or other anatomic features allows better depiction of the anatomy of the arterial and venous components (14). However, uterine ar- tery angiography remains the diagnostic tool of choice for UVM, because both diagnosis and immediate embolization can be per- formed simultaneously by the interventionist (1, 15).
In the past, hysterectomy or surgical ligation of the uterine ar- tery was widely performed for the treatment of UVM (16). How- ever, hysterectomy has a major limitation as it cannot preserve the patient’s fertility after surgery (17-19).
Wu et al. (17) introduced laparoscopic bipolar coagulation of
uterine vessels, which can relieve symptoms and has advantages such as shorter surgical times and absence of radiation exposure.
However, general anesthesia and laparoscopic surgery are re- quired.
Transarterial embolization of a UVM was first introduced by Forssman et al. (18). The benefits of UAE are that it is minimally invasive, preserves the uterus, requires less hospitalization and results in a shorter recovery period. Currently, hysterectomy is performed to treat uterine AVM only in those women who do not want additional pregnancies or who do not have the capacity to bear children. In addition, many previous studies have re- vealed that UAE is safer and less invasive than surgical proce- dures (19-21).
UAE should be performed in bilateral uterine arteries, be- cause the uterine artery has many collateral supply channels and reperfusion from a contralateral uterine artery can occur, which may induce continuous bleeding or rebleeding after emboliza- tion (22-24).
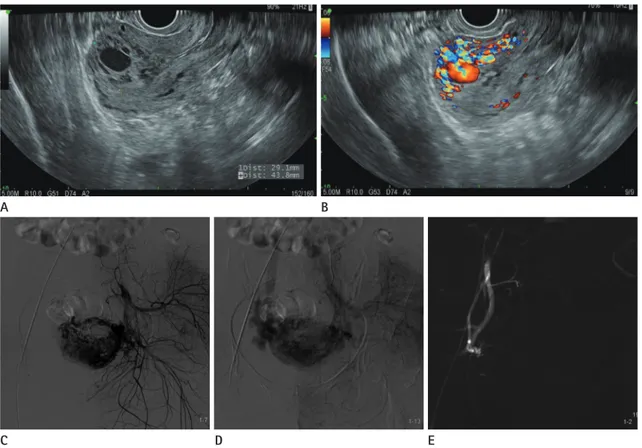
Fig. 2. A 30-year-old woman presented with intermittent vaginal bleeding for 1 month after missed abortion.
Transvaginal Gray-Scale (A) and color Doppler (B) ultrasonograms show a tangle of tortuous vessels with increased vascularity in the uterine fundus. Selective left uterine angiogram (C, D) demonstrates an hypertrophied uterine artery and a vascular mass lesion with early venous drain- age during the arterial phase. Post-embolization pelvic angiogram (E) shows eradication of the vascular mass and complete occlusion of the uterine artery.
A
C D E
B
Embolization materials widely used in these procedures are gelatin sponge particles, polyvinyl alcohol (PVA), coils, glues, de- tachable balloons, or a combination thereof (15, 19, 21-23). Gela- tin sponge particles are used as a means of causing mechanical obstruction, slowing blood flow and hastening thrombus forma- tion (25). However, embolization using gelatin sponge particles causes temporary vessel occlusion and allows recanalization in a few weeks, leading to a risk of reperfusion or rebleeding (25).
PVA results in a permanent embolic effect by adherence to the vessel wall, causing stagnation of flow, and direct occlusion of the smallest vessels into which it can fit. Coils are also permanent embolic agents available in various sizes and shapes. They induce mechanical thrombosis by themselves and chemical thrombo- genesis due to their fibers. However, a potential complication of coil embolization is the occlusion of non-targeted vessels due to migration, which can result in cerebral infarction or pulmonary embolism. This can occur during treatment of high-flow condi- tions such as AVM or arteriovenous fistula. N-butyl-2-cyanoac- rylate (NBCA), commonly used in the treatment of cerebral AVM and spinal tumors, is also used to treat uterine AVM. NBCA is a clear and free-flowing monomer. When it is exposed to water or blood, polymerization is induced, and it results in an intravascu- lar cast. McCormick and Kim (26) reported successful emboliza- tion of uterine AVMs with NBCA. The disadvantages of using NBCA are the need for a special syringe and materials and the risk of catheter embedding (25). Ethylene vinyl alcohol copoly- mer (Onyx is the commercial name) is also widely used for treat- ment of cerebral AVM. Akbayir et al. (27) reported a case of uter- ine AVM treated with a combination of Onyx and other materials. However, in our study, the embolic agents used in all embolization sessions were gelatin sponge particles. Only during three procedures, additional microcoils were needed due to high flow malformation. Hence, gelatin sponge particles are adequate embolic agents for management of acquired UVMs.
Kim et al. (28) reported successful restoration of the menstrual cycle within two months in all 19 patients who underwent UAE using gelatin sponge particles or PVA. This result of the previous study is compatible with that of our study.
Peitsidis et al. (20) performed a systematic review of case re- ports of UVM treatment and identified 17 pregnancies (17%) af- ter UAE for treatment of UVM. We observed normal pregnancy and term delivery in two patients (10.5%), who had undergone
bilateral UAE. Maleux et al. (4) estimated that the mean time pe- riod from UAE to subsequent pregnancy was 15.6 months in their report. The mean time period between embolization and delivery was 20.1 months in our study. Therefore, our study con- firms the previously reported result regarding the potential to be- come pregnant after particulate UAE (3, 29, 30).
The possible complications associated with UAE are groin he- matoma, uterine ischemia, pelvic infections such as tubo-ovarian abscesses, endometritis, and transient or permanent amenorrhea (31). In our study, the number of minor adverse events due to the procedure was low. Pelvic pain was observed during the first week in three patients, but the pain was relieved by conservative treatment. None of the patients presented with amenorrhea, as described in 4% of the cases after bilateral UAE for the treatment of uterine myomas. No major adverse events were observed in our study.
Our study has some limitations. The retrospective design and the small number of patients included in the study do not allow extensive statistical analysis.
In conclusion, transarterial bilateral UAE is a safe and effective treatment in patients with vaginal bleeding caused by acquired UVM. This procedure allows preservation of uterine function with the possibility of future pregnancy. Transarterial bilateral UAE should be considered as a primary treatment option in these patients.
REFERENCES
1. Hoffman MK, Meilstrup JW, Shackelford DP, Kaminski PF.
Arteriovenous malformations of the uterus: an uncom- mon cause of vaginal bleeding. Obstet Gynecol Surv 1997;
52:736-740
2. Newlands ES, Bagshawe KD, Begent RH, Rustin GJ, Holden L, Dent J. Developments in chemotherapy for medium- and high-risk patients with gestational trophoblastic tu- mours (1979-1984). Br J Obstet Gynaecol 1986;93:63-69 3. McIvor J, Cameron EW. Pregnancy after uterine artery
embolization to control haemorrhage from gestational trophoblastic tumour. Br J Radiol 1996;69:624-629 4. Maleux G, Timmerman D, Heye S, Wilms G. Acquired uter-
ine vascular malformations: radiological and clinical out- come after transcatheter embolotherapy. Eur Radiol 2006;
16:299-306
5. Mulliken JB, Glowacki J. Hemangiomas and vascular mal- formations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:
412-422
6. Mitty HA, Baron MG, Jacobson JH 2nd. Pelvic arteriove- nous malformations. Am J Roentgenol Radium Ther Nucl Med 1968;102:427-430
7. Calligaro KD, Sedlacek TV, Savarese RP, Carneval P, DeLau- rentis DA. Congenital pelvic arteriovenous malformations:
long-term follow-up in two cases and a review of the lit- erature. J Vasc Surg 1992;16:100-108
8. Kwon JH, Kim GS. Obstetric iatrogenic arterial injuries of the uterus: diagnosis with US and treatment with trans- catheter arterial embolization. Radiographics 2002;22:35- 46.
9. Polat P, Suma S, Kantarcý M, Alper F, Levent A. Color Dop- pler US in the evaluation of uterine vascular abnormali- ties. Radiographics 2002;22:47-53
10. Grivell RM, Reid KM, Mellor A. Uterine arteriovenous mal- formations: a review of the current literature. Obstet Gyne- col Surv 2005;60:761-767
11. Cura M, Martinez N, Cura A, Dalsaso TJ, Elmerhi F. Arterio- venous malformations of the uterus. Acta Radiol 2009;50:
823-829
12. Burrows PE. Vascular malformations involving the female pelvis. Semin Intervent Radiol 2008;25:347-360
13. Huang MW, Muradali D, Thurston WA, Burns PN, Wilson SR. Uterine arteriovenous malformations: gray-scale and Doppler US features with MR imaging correlation. Radiol- ogy 1998;206:115-123
14. Díaz Candamio MJ, Lee VS, Rofsky NM, Krinsky GA, Wein- reb JC. Pelvic arteriovenous malformations: gadolinium- enhanced three-dimensional MR angiography findings. Eur Radiol 2000;10:1257-1260
15. Rangarajan RD, Moloney JC, Anderson HJ. Diagnosis and nonsurgical management of uterine arteriovenous malfor- mation. Cardiovasc Intervent Radiol 2007;30:1267-1270 16. Paraskevaides E, Noelke L, Afrasiabi M. Internal iliac artery
ligation (IIAL) in obstetrics and gynaecology. Eur J Obstet Gynecol Reprod Biol 1993;52:73-75
17. Wu YC, Liu WM, Yuan CC, Ng HT. Successful treatment of
symptomatic arteriovenous malformation of the uterus using laparoscopic bipolar coagulation of uterine vessels.
Fertil Steril 2001;76:1270-1271
18. Forssman L, Lundberg J, Scherstén T. Conservative treat- ment of uterine arteriovenous fistula. Acta Obstet Gyne- col Scand 1982;61:85-87
19. Kim TH, Lee HH. Presenting features of women with uter- ine arteriovenous malformations. Fertil Steril 2010;94:2330.
e7-e10
20. Peitsidis P, Manolakos E, Tsekoura V, Kreienberg R, Schwent- ner L. Uterine arteriovenous malformations induced after diagnostic curettage: a systematic review. Arch Gynecol Ob- stet 2011;284:1137-1151
21. Molvi SN, Dash K, Rastogi H, Khanna SB. Transcatheter embolization of uterine arteriovenous malformation: report of 2 cases and review of literature. J Minim Invasive Gyne- col 2011;18:812-819
22. Pelage JP, Le Dref O, Mateo J, Soyer P, Jacob D, Kardache M, et al. Life-threatening primary postpartum hemorrhage:
treatment with emergency selective arterial embolization.
Radiology 1998;208:359-362
23. Pelage JP, Soyer P, Repiquet D, Herbreteau D, Le Dref O, Houdart E, et al. Secondary postpartum hemorrhage: treat- ment with selective arterial embolization. Radiology 1999;
212:385-389
24. Deux JF, Bazot M, Le Blanche AF, Tassart M, Khalil A, Ber- kane N, et al. Is selective embolization of uterine arteries a safe alternative to hysterectomy in patients with postpar- tum hemorrhage? AJR Am J Roentgenol 2001;177:145-149 25. Vaidya S, Tozer KR, Chen J. An overview of embolic agents.
Semin Intervent Radiol 2008;25:204-215
26. McCormick CC, Kim HS. Successful pregnancy with a full- term vaginal delivery one year after n-butyl cyanoacrylate embolization of a uterine arteriovenous malformation. Car- diovasc Intervent Radiol 2006;29:699-701
27. Akbayir O, Gedikbasi A, Akyol A, Ucar A, Saygi-Ozyurt S, Gulkilik A. Cesarean scar pregnancy: a rare cause of uterine arteriovenous malformation. J Clin Ultrasound 2011;39:534- 548
28. Kim T, Shin JH, Kim J, Yoon HK, Ko GY, Gwon DI, et al. Man- agement of bleeding uterine arteriovenous malformation with bilateral uterine artery embolization. Yonsei Med J
2014;55:367-373
29. Stancato-Pasik A, Mitty HA, Richard HM 3rd, Eshkar N.
Obstetric embolotherapy: effect on menses and pregnancy.
Radiology 1997;204:791-793
30. Poppe W, Van Assche FA, Wilms G, Favril A, Baert A. Preg- nancy after transcatheter embolization of a uterine arte-
riovenous malformation. Am J Obstet Gynecol 1987;156:
1179-1180
31. Yang SB, Lee SJ, Joe HS, Goo DE, Chang YW, Kim DH. Selec- tive uterine artery embolization for management of inter- stitial ectopic pregnancy. Korean J Radiol 2007;8:176-179
후천성 자궁 혈관 기형: 경피적 경동맥 색전술의 임상적 결과
강채훈
1· 양승부
2* · 구동억
2· 김용재
2· 이재명
2· 이웅희
2목적: 후천성 자궁 혈관 기형 환자에게 있어서 양측 자궁 동맥에 대한 경동맥 색전술의 임상적 결과를 알아보고자 한다.
대상과 방법: 이 후향적 연구는 2003년 1월부터 2011년 6월까지 증상이 있는 자궁 동맥 기형 치료로 양측 자궁 동맥에 대해 경동맥 색전술을 시행받은 총 19명의 환자의 진료 기록을 토대로 이루어졌다. 색전술은 카테터와 혈관 조영술 방법 을 이용하여 한쪽 대퇴동맥 경로를 통하여 이루어졌다. 임상적 성공은 비정상적 질출혈 문제의 현저한 해결로 정의하였다.
시술 후 합병증에는 색전술과 관련된 모든 이상 반응을 포함하였다.
결과: 총 19명의 환자에서 20번의 시술이 시행되었다. 첫 번째 시술에서 현저하게 빠른 속도의 기형으로 인해 색전되지 않은 한 명의 환자에서 재시술이 요구되었다. 임상적으로 전 환자에게서 색전술 후 출혈이 즉시 조절되었다. 합병증은 추 적 관찰 기간 동안 모든 환자에게서 발생하지 않았다. 성공적인 색전술을 시행받은 환자 모두가 1~2개월 이내에 정상적 인 월경 주기에 돌아왔다. 19명 중 2명에게서 정상 임신과 만삭 분만이 이루어졌다.
결론: 후천성 자궁 동맥 기형에 의해 일어난 질출혈 환자에게 있어 양측 자궁 동맥에 대한 경동맥 색전술은 안전하고 효 과적인 치료법이며, 향후 임신의 가능성을 열어 준다.
1강릉아산병원 영상의학과, 2순천향대학교 구미병원 영상의학과