Introduction
Stroke is the 2nd most common cause of mortality in the world, and it is also the most common cause of morbidity among all the neurological diseases.
Therefore, prevention, early diagnosis and treatment of complications after stroke are important.
1,2Motor weakness of limb is common complaint after stroke.
Particularly, paresis of the wrist or finger extensor muscles is more common because of antisynergic effect of upper limb,
3,4which may be called as pseudoradial nerve palsy.
5Stroke patients may also have polyneuropathies and entrapment neuropathies because of long stay in bed due to paresis.
6It could lead to pain, paresthesia and loss of function of parts innervated by the nerves. If there are another causes
뇌졸중 환자의 마비 측에 동반된 급성 요골신경병증: 증례보고
정필우
1
, 김기훈2
, 박병규2
, 김동휘2
1금천 재활요양병원 재활의학과, 2고려대학교 의과대학 재활의학교실
A Case of Acute Radial Neuropathy in the Affected Side of a Patient with Stroke
Pill Woo Choung
1, Ki Hoon Kim
2, Byung Kyu Park
2, Dong Hwee Kim
21
Department of Physical Medicine & Rehabilitation, Kumcheon Su Hospital,
2Department of Physical Medicine & Rehabilitation, College of Medicine, Korea University, Seoul, Korea
Received November 21, 2016
Revised (1st) January 23, 2017, (2nd) May 4, 2017 Accepted May 10, 2017
Corresponding Author: Dong Hwee Kim
Department of Physical Medicine & Rehabilitation, Korea University Ansan Hospital, Korea University College of Medicine, 123 Jeokgeum-ro, Danwon-gu, Ansan 15355, Korea
Tel: 82-31-412-5330, Fax: 82-31-412-5344, E-mail: rmkdh@korea.ac.kr
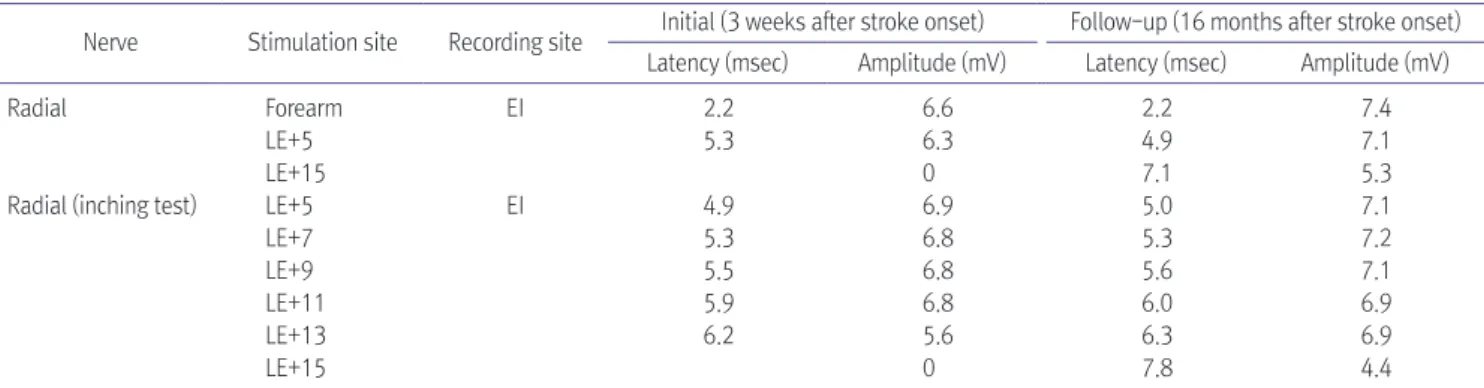
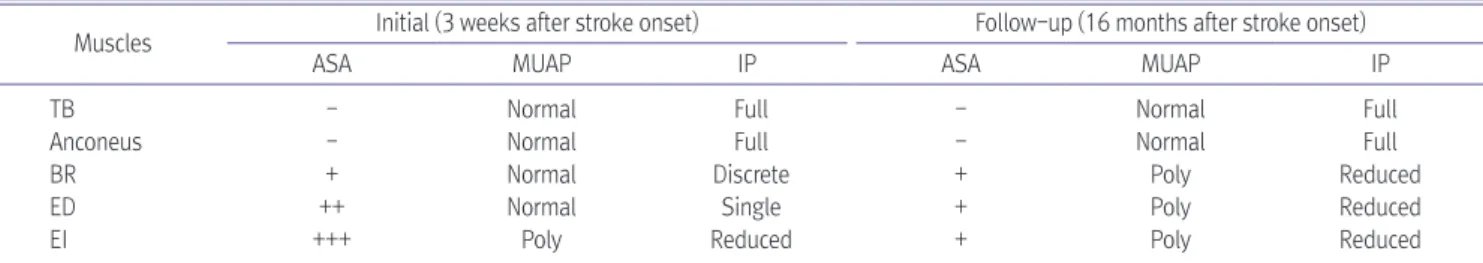
Motor weakness of limbs and trunk are common complaint after stroke. If there are other concurrent causes of motor weakness like focal entrapment neuropathy in paretic limb, it is hard to find them because of weakness due to stroke. A man with the left basal ganglia hemorrhage complained of motor weakness of the right upper extremity, especially wrist and finger extensors. Motor nerve conduction study revealed the right radial neuropathy with definite conduction block between 13 cm and 15 cm proximal to the lateral epicondyle. Ultrasonography showed swelling of right radial nerve at the same lesion. After dexamethasone injection around the right spiral groove, electrodiagnostic findings and clinical feature were significantly improved. In case stroke patients with hemiplegia show persistent motor and sensory impairment in the specific peripheral nerve territory despite of recovery, concomitant neuropathy on the affected side should be considered.
Key Words: stroke, radial nerve, wrist drop, electrodiagnois, ultrasonography
Copyright © by Korean Association of EMG Electrodiagnostic Medicine
This is an Open Ac cess article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.