Case report
A 23-years old male was referred with painful mass on the Right fibular head for three month after minor trauma on the knee, progressive motor weakness of dorsi- flexion of the ankle and toes, and eversion of the foot and hypoesthesia of the peroneal nerve territory were developed gradually.
Electromyography (EMG) revealed abnormal spontaneous activities in the examined mus- cles innervated by the peroneal nerve below
knee level, and motor nerve conduction velocity (NCV) study revealed slowed con- duction velocity of peroneal nerve below knee level and diagnosed as incomplete paralysis of the common peroneal nerve.
Ganglionic cyst typically image similar to fluid on MRI with a low signal intensity on T1-weighted images and high signal intensi- ty on T2-weighted images. After contrast administration, T1-weighted image shows significant contrast enhancement peripheral- ly. In this case, MR imaging showed cystic mass in the postero-inferior portion of the
※통신저자: 송 광 순
대구시 중구 동산동 1 9 4
계명대학교 의과대학 정형외과학교실
Tel: 053) 250-7250, Fax: 053) 250-7205, E-mail: skspos@dsmc.or.kr
총 비골 신경에 발생한 결절종
- 증례보고 -
계명대학교 의과대학 정형외과학교실
송광순・전시현・김인규
결절종으로 인한 총 비골 신경 마비는 매우 드문 예에서 보고되고 있지만, 잘 알려져 있는 질환이다. 결절종으로 인한 비골 신경 포착을 보이는 자기 공명 영상 소견에 대하여 3편이 보 고되어 있다. 본 증례에서는 진단을 위해 초음파, 자기 공명 영상, 근전도, 신경전도 검사 및 조직 검사를 시행하였다. 비골 경부 주변의 관상 구조는 자기 공명 영상 소견 상 특징적으로 T2 강조영상에서 고신호를 보이면서 상부 경비골 관절의 아래 부분까지 종축으로 뻗어있는 소 견을 보였다. 비골 신경을 노출시키고 결절종에 대해 병소내 절제술을 시행하였다. 수술 후에 도 마비 증상이 지속되었으나, 수술 후 4개월부터 점차적으로 마비의 회복소견을 보이기 시작 했고 술 후 7개월에 완전한 회복을 보였다. 본 증례에서 자기 공명 영상은 낭종의 범위, 위 치, 기원을 밝혀 내는데 도움을 주었고, 외과적 절제술로 좋은 결과를 얻을 수 있다.
색인 단어: 결절종, 비골 신경, 자기 공명 영상, 절제술 J. of Korean Bone & Joint Tumor Soc.
Volume 9, Number 2, December, 2003
fibular head, measuring about 16 mm in diameter with subtle peripheral rim enhancement on Gandolinium-enhanced T1- weighted images and high signal intensity on the T2-weighted image and intermediate
signal on the T1-weighted image of the per- oneal nerve with extending to the proximal tibiofibular joint (Fig. 1, 2, 3). The mass around the fibular head was exposed with curvilinear incision in 5 cm length on the fibula head, and a pale tan to white colored ganglionic cyst was located within the per- oneal nerve. Also, a stalk of cyst was extended to the proximal tibiofibular joint beneath the tibialis anterior muscle. We iso- lated and intralesionally excised the cystic mass originated from interfuniculi without microscope. Then, we carefully decompressed three funiculi that were stretched and attached to the lateral wall of the cyst.
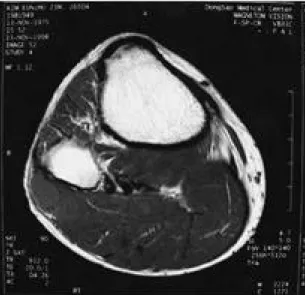
During dissection of the cystic mass from the nerve, one funiculus was removed with the cyst. The histologic finding of the speci- men showed typical endothelial lining cells on the inner wall of the cyst, which is con- comitant to the histology of the ganglion (Fig.4). Immediately after operation, com- plete loss of motor power was noted, so we applied ninety degrees ankle stop short leg Fig. 1. T1-weighted images (TR/TE: 912/20) transverse
images show a mass at just below the knee level.
The ganglion cyst is seen as round mass of inter- mediate signal intensity near the fibular neck.
Fig. 2. T2-weighted images(TR/TE: 4500/96) at the same level as Fig.1 showing the high signal from the cyst.
Fig. 3. Gadolinium-enhanced T1-weighted images (TR/TE: 1500/20) at the same level as Fig.1 showing peripherally enhanced cyst.
brace. We checked periodically the change of the neurologic sign with a month interval.
The findings of EMG & NCV checked at 4 weeks after the operation, revealed no inter- val change, compare to the preoperative finding despite of an aggravation of the motor power. At 4 months after the opera- tion, motor function started to recover and had recovered completely at 7 months fol- low-up.
D i s c u s s i o n
Ganglionic cysts in the peroneal nerve are rare but well recognised entities after the first description by Duchenne in 18011 , 2 , 3 , 8 ). Nucci reviewed the literatures and found 60 c a s e s9 ).
The pathogenesis of ganglionic cyst found in the common peroneal nerve, is still con- troversial. Cobb reviewed many literatures and several hypotheses were proposed for the ganglionic cyst within the nerve including mucinous degeneration or metaplasia of the perineural connective tissue, normal response to a stimulus to the specialised connective
tissue forming joints and nerve sheath or intraneural haemorrhage with reabsorption of the hematoma. However, Cobb believed that ganglia arising from the joint capsule are a different entity, and they may cause dysfunction by extrinsic pressure on the nerve, not intraneurall 2 ). Scherman suggest- ed that they are formed from myofibroblasts outside the nerve and susbsequentially invade the nerve sheath and myofibroblast was confirmed by electron microscopy1 3 ). Currently, the synovial theory is the most consensus regards these lesions as genuine cysts of articular or para-articular origin1 , 8 - 1 0 , 1 3 ). The stalk connecting the cyst to the superior tibiofibular joint seen in about 40% of reported cases is said to be an important point of this theory. The same findings in our case are also consistent with this theory.
For the diagnosis of the ganglion cyst of the common peroneal nerve, clinical combination is said to be diagnostic, whether or not there is a palpable swelling at the fibular neck1 1 ). There have been reports about diagnostic modalities including ultrasonography, com- puted tomography, MRI were used1 , 3 , 4 , 6 , 8 ). Coakley reported that the finding of a tubu- lar structure near the fibular neck extension towards the superior tibiofibular joint and intermediate T1 and high T2 signal intensity of the cyst with increased signal in the per- oneal compartment in association with clini- cal and EMG evidence of denervation are n o t e w o r t h y2 , 1 5 ). The findings of MR imaging of our case showed very similar findings described by Coakley. The image of MR imaging was helpful for diagnosis and preop- erative planning for the surgical excision of the mass. Various treatment regimens have been reported over the years, some surgeons recommend the injection of sclerosing agent and others prefer radiotherapy1 2 ). In our Fig. 4. Light micrograph shows a fibrous connective tis-
sue, a portion of cyst wall(large arrow), which is connected, with sheath of adjacent nerve(small arrow). The cystic wall is not lined by synovial cells (H & E stain, 100)
opinion, operation is the treatment of choice if palsy is evident. Even though some sur- g e o n2 , 5 , 9 , 1 3 , 1 4 ) prefer subtotal removal of the cyst due to nerve damage by total removal.
Nucci et al said that the accurate dissection made possible by operating microscope often permits total removal of the cyst without damage of the nerve fascicle, thus providing the conditions for good functional recovery8 , 1 5 ). In our case, total removal of the cyst was performed. In spite of the iatrogenic resec- tion of one funiculus during operation, our patient showed almost complete recovery of the function at 7 months after the opera- tion. So, cause of neurologic impairment seems nerve retraction in our case.
According to the literature, clinical improve- ment varies from gradual recovery to nearly full recovery. However, we believe that clin- ical improvement depends on the severity of the nerve damage caused by the cyst and most of all, meticulous dissection of the c y s t .
REFERENCES
11) Coakley FV, Finaly WM, Harper WM and Allen M J: Direct and indirect MRI findings in ganglion cysts of the common peroneal nerve. Clini Radiol, 50(3): 168-169, 1995.
12) Cobb CA and Moiel RH: Ganglion of the peroneal nerve. J Neurosurg, 41: 255-259, 1974.
13) Fansa H, Plogmeier K, Gonschorek A and Feistner H: Common peroneal nerve palsy caused by a ganglion. Case report. Scand J Plast Reconstr Surg Hand Surg, 32(4): 425-7, 1998.
14) Gambari PI, Giuliani G, Poppi M and Pozzati E:
Ganglionic cyst of peroneal nerve at the knee: CT
and surgical correlation. J Comput Assist Tomogr, 14(5): 801-3, 1990.
15) Kart MR and Lenobel MI: Intraneural Ganglionic cyst of the peroneal nerve. J Neurosurg, 32: 692- 694, 1970.
16) Leijten FS, Arts WF and Puylaert JB: Ultrasound diagnosis of an intraneural ganglion cyst of the per- oneal nerve. Case Report. J Neurosug, 76(3): 538- 40, 1992.
17) Leon J and Marano G: MRI of peroneal nerve entrapment due to a ganglion cyst. Magn Reson Imaging, 5: 307-309, 1987.
18) Nicholson TR, Cohen RC and Grattan-Smith PJ:
Intraneural ganglion of the common peroneal nerve in a 4-year-old boy. J Child Neuro, 10(3): 213-5, 1995.
19) Nucci F, Artico M, Santoro A, Delfini R, Bosco S and Palma L: Intraneural synovial cyst of the per- oneal nerve. Report of two cases and review of the literature. Neurosurgery, 26(2): 339-40, 1990.
10) Parkes A : Intraneural ganglion of the lateral popliteal nerve. J Bone and Joint Surg(Br), 43-B:
784-790, 1961.
11) Poppi M, Nasi MT, Giuliani G, Acciarri N and Montagna P: Intraneural ganglion of the peroneal nerve: An Unusual Presentation. Surg Neurol, 31:
405-406, 1989.
12) Przystawski N, McGarry JJ, Stem MB and Edelman RD: Intratendinous ganglionic cyst. J Foot Surg, 28: 244-247, 1989.
13) Scherman BM, Bilbao JM, Hudson AR and Briggs SJ: Intraneural Ganglion: A case Report with Electron Microscopic Observations. Neurosur- gery, 8: 487-490, 1981.
14) Schrijver FD, Simon JP, Smet LD and Fabry G:
Ganglia of the superior tibiofibular joint: report of three cases and review of the literature. A c t a Orthopedica Belgica, 64-2: 233-241, 1998.
15) S p i l l a n e R M , W h i t m a n G J a n d C h e w F S : Peroneal nerve ganglion cyst. Am J Roentgenol, 166(3): 682, 1996.
Ganglionic Cyst of the Peroneal Nerve - A Case Report -
Kwang Soon Song, M.D., Si Hyun Jeon, M.D., In Kyu Kim, M.D.
Department of Orthopaedic Surgery, School of Medicine, Keimyung University, Daegu, Korea
A Common peroneal nerve palsy caused by ganglionic cyst is very rare condition but well recognised entities. There have been three previous reports describing the magnetic resonance image (MRI) findings of peroneal nerve entrapment due to a ganglionic cyst. Ultrasonography, MRI, and electromyography (EMG), nerve conduction velocity (NCV), and microscopic exami- nation were taken for diagnosis. A tubular structure near the fibular neck extending longitudinal- ly over several slices with an inferior extension towards the superior tibiofibular joint with high T2 signal intensity was characteristic. The peroneal nerve was exposed and the ganglionic cyst was excised. The nerve was paralysed immediately after operation, but at 4 month after opera- tion, started recovery of the function gradually and has recovered completely at 7 month. MRI is helpful to detect the extent, location, and origin of the cyst. Meticulous surgical excision can provide favorable result.
Key Words: Ganglionic cyst, Peroneal nerve, MRI, Excision
Address reprint requests to Kwang Soon Song, M.D.
Department of Orthopedics Surgery, School of Medicine, Keimyung University
#194 Dongsandong, Daegu, Korea
TEL: 82-53-250-7250, Fax: 82-53-250-7205, E-mail: skspos@dsmc.or.kr
Abstract