Effect of Pre-operative Biliary Drainage on Surgical Outcomes after Pancreaticoduodenectomy in Patients with Common Bile Duct Cancer
전체 글
수치


관련 문서
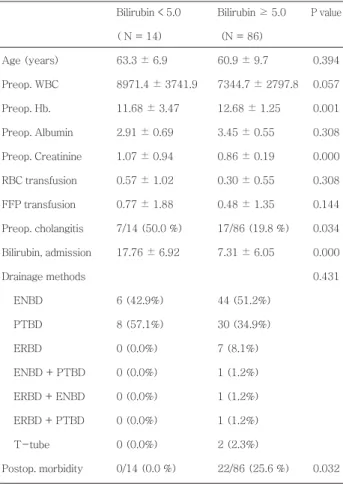
Through a review of electronic medical records, we analyzed the applied BCSs, perioperative hematologic changes, and morbidity and mortality in JW patients
Polypoid lesions of the gallbladder; Report of 111 cases with surgical reference to operative indication.. Polypoid lesion of GB: Indication of carcinoma
Background The aim of this study was to compare the surgical outcomes of robotic single-site (RSS-H) and laparoendoscopic single-site total hysterectomy (LESS-H) and to
Among the various pulmonary manifestations, interstitial lung disease (ILD) is known to be associated with substantial morbidity and mortality rates in RA patients.. As RA-ILD
First, the comparison of pre and post-cardiovascular endurance between the experimental group, which participated in 12-week sports leisure activities regularly,
To evaluate the Effect of mutant RANKL on mRNA expressions in related with osteoclastogenesis,we investigated the expression of several osteoclast- specific genes both
The Development and Application of Unified Prestress System with Post-tension and Post-compression for Bridge... Unified Prestress
In the control group, lifestyle-related factors were significantly different only in blood glucose (p <.01) and there was no significant difference in