pISSN 1229-5418 eISSN 2671-6623
Implantology 2019; 23(4): 229-234 https://doi.org/10.32542/implantology.2019020
Received: December 24, 2019 Revised: December 27, 2019 Accepted: December 27, 2019 ORCID
Kyehee Wee
https://orcid.org/0000-0003-3185-7835 Bo-Ah Lee
https://orcid.org/0000-0003-3586-4928 Copyright © 2019. The Korean Academy of Oral &
Maxillofacial Implantology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.
org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
OPEN ACCESS
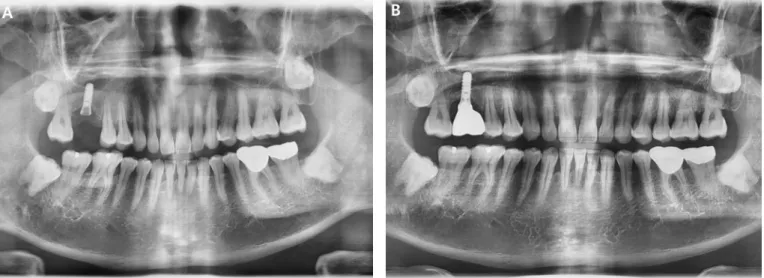
Dental implants may be a valid prosthetic treatment to replace a single tooth, but there are some complications. One complication of dental implants is a fracture of the implant. This case report describes the implant fracture of a tissue-level implant. A patient with a tissue-level implant that was placed on the right maxillary first molar ten years ago visited the clinic because the implant prosthesis was fallen out with the fractured abutment screw. Panoramic radiograph confirmed the fracture of the abutment screw. After removing the screw fragment, a new restoration was applied.
After two years, not only the screw but also the fixture was broken. The fixture fragment was surgically removed. This case implies that screw fractures can be a precursor to fixture fractures and regular check-up is necessary for preventing implant fractures.
Keywords: Dental implants, Fatigue fractures, Marginal bone loss, Peri-implant fractures
Abstract
Level Implant: A Case Report
Kyehee Wee, MS
1, Bo-Ah Lee, DDS, PhD
2*1
Specialist, Department of Dentistry, National Police Hospital, Seoul, Korea
2