pISSN 2287-2892 • eISSN 2288-2561
JLA
Acute Stent Thrombosis after Coronary Stenting in Patients with Acute Coronary Syndrome
Hyo-Sun Shin1,3, Sang-Hyun Kim2,3, Hack-Lyoung Kim2,3, Jae-Bin Seo2,3, Woo-Young Chung2,3, Joo-Hee Zo2,3, Myung-A Kim2,3
1Division of Cardiology, Department of Internal Medicine, Seoul National University Hospital, Seoul,
2Division of Cardiology, Department of Internal Medicine, Seoul Boramae Medical Center, Seoul,
3Seoul National University College of Medicine, Seoul, Korea
Acute stent thrombosis after percutaneous coronary intervention (PCI) is still problematic because of the subsequent development of myocardial infarction and poor prognosis. The incidence of acute stent thrombosis, occurring within 0-24hours after PCI, is relatively low, but underlying causes and treatment strategy are not well defined. Multi-vessel disease, ST-elevated myocardial infarction (STEMI), and large thrombotic burden are known risk factors of acute stent thrombosis. Thrombus aspiration, balloon angioplasty and glycoprotein IIb/IIIa receptor blocker could be therapeutic options.
Recently we experienced two cases of acute stent thrombosis which developed during PCI with the aggravation of chest pain, and acute stent thrombosis were diagnosed immediately and successfully treated. Here we report two cases of acute stent thrombosis during PCI for one patient with STEMI and the other with acute coronary syndrome, which were successfully treated with thrombus aspiration and intravenous infusion of glycoprotein IIb/IIIa receptor blocker.
Key Words: Coronary thrombosis, Acute coronary syndrome, Abciximab
Received:
Revised:
Accepted:
March 14, 2014 May 29, 2014 June 11, 2014
Corresponding Author: Sang-Hyun Kim, Division of Cardiology, Department of Internal Medicine, Seoul Boramae Medical Center, Seoul National University College of Medicine, 20, Borimae-ro, 5-gil, Dongak-gu, Seoul 156-707, Korea Tel: +82-2-870-3864, Fax: +82-2-870-3866, E-mail: shkimmd@snu.ac.kr
This is an Open Access article distributed under the terms of the creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
INTRODUCTION
After the advent of percutaneous coronary inter- vention (PCI), mortality of acute coronary syndrome continues to decline, but stent thrombosis (ST) after PCI remains a residual problem of the procedure. ST occurs about 1-2% of total PCI cases1-7 and acute stent throm- bosis, occurring within 0-24hours after PCI, accounts for 6-25% of all ST cases.1,8 Although the incidence of ST is relatively low, prognosis of ST is dismal; with a case-fatality rate of 15-45%.5,7 Nonetheless underlying causes and treatment strategy of ST are not-well defined.
Physician’s concept or suspicion of acute stent throm- bosis can be enough for the diagnosis and improve the prognosis of those patients. Here we report two cases of acute stent thrombosis during PCI for one patient with ST-elevated myocardial infarction (STEMI) and the other with acute coronary syndrome, which were successfully treated with thrombus aspiration and intravenous injection of glycoprotein IIb/IIIa inhibitor.
CASE 1
A 66-year-old man visited the Emergency Department
Fig. 1. Initial electrocardiogram showed ST-segment elevation in leads I, avL, V1, V2, V3, V4 with reciprocal changes of ST-segment in leads II, III, and aVF.
Fig. 2. Initial chest X-ray showed bilateral pulmonary edema.
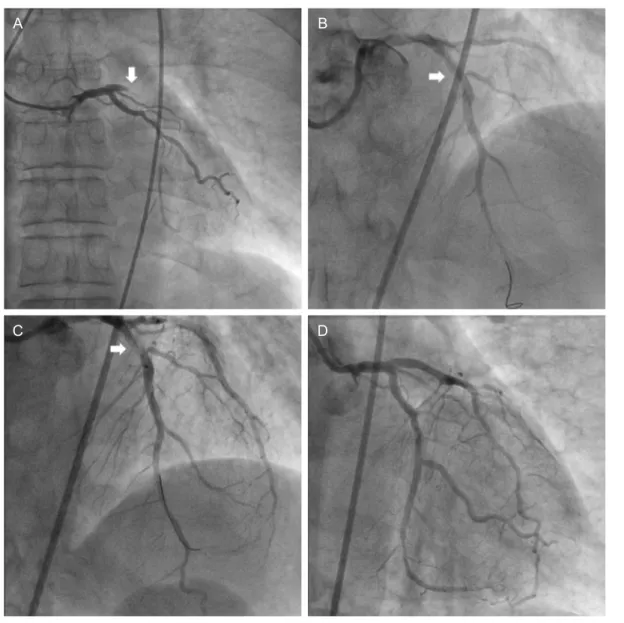
with complaint of chest pain of squeezing nature which developed 30 minutes before. On admission, his blood pressure was 113/74 mmHg, and his heart rate was 94 beats per minute, and respiration rate was 30 /min. The electrocardiogram (ECG) showed ST-segment elevation in leads I, aVL, V1, V2, V3, V4 with reciprocal changes of ST-segment in leads II, III, and aVF (Fig. 1). The chest X-ray showed severe pulmonary edema (Fig. 2). Medical treat- ment was started immediately including aspirin 300 mg, clopidogrel 600 mg, intravenous nitrate infusion and bolus injection of unfractionated heparin 6,500 units. Unfrac- tionated heparin was administered before PCI and repeatedly at every hour during PCI with monitoring activated clotting time for the maintenance over 300 seconds. He received emergent coronary angiography (CAG), and it showed total occlusion of the proximal left anterior descending coronary artery (LAD) with thrombus (Fig. 3-A) and segmental stenosis in left circumflex coro- nary artery (LCX). There were stenotic lesions in middle and distal right coronary artery (RCA). He showed severe pulmonary edema on chest x-ray and multiple stenotic lesions of coronary arteries, so we decided PCI on LAD and LCX. He underwent balloon angioplasty and evero-
limus eluting stent (3.0×18 mm Xience V stent, Abbott) was inserted in proximal LAD at first (Fig. 3-B). Two Everolimus eluting stents were inserted in proximal and distal LCX. After PCI, patient suddenly complained of chest pain again. We checked the left coronary artery angiogram again and found newly developed intraluminal filling defect due to stent thrombosis of the proximal LAD, which
Left
Fig. 3. (A) Left anterior oblique (LAO) projection with caudal angulation of selective left coronary angiogram showed the total occlusion with thrombus in the proximal part of left anterior descending artery (arrows), (B) LAO projection with cranial angulation of selective left CAG. Everolimus eluting stent (3.0×18 mm Xience V stent, Abbott, USA) was successfully placed in the LAD (arrows), (C) Right anterior oblique projection with cranial angulation of selective left CAG after RCA treatment showed intraluminal filling defect of the targeted lesion of LAD (arrows), (D) After thrombus aspiration and infusion of glycoprotein IIb/IIIa receptor blocker, CAG showed recovery of coronary flow.
was treated 45 minutes before (Fig. 3-C). After intravenous administration of a glycoprotein IIb/IIIa receptor blocker (Abciximab), thrombus aspiration and balloon angioplasty were done. A final angiogram revealed improved flow through all coronary arteries (Fig. 3-D). 4 days after, a second look CAG showed patent flow through all stented vessels. There were no predisposing factors including abnormal findings of coagulation system such as protein
C or S, anti-phospholipid antibody and no evidence of malignancy. He was discharged with triple anti-platelet therapy of aspirin 100 mg, clopidogrel 75 mg, and cilostazol 200 mg daily. This patient was followed-up via outpatient clinic uneventfully, and repeat CAG performed after 12 months showed patent coronary flow.
A B
C D
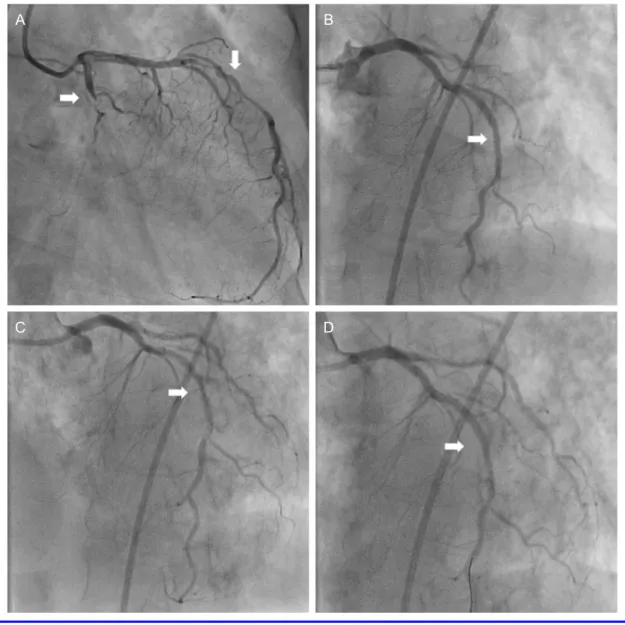
Fig. 4. (A) Right anterior oblique (RAO) projection with caudal angulation of selective left coronary angiogram showed the long segmental concentric stenosis in proximal to middle LAD and total occlusion in proximal LCX (arrows), (B) LAO projection with cranial angulation of selective left CAG. Two Everolimus eluting stents (2.5×28 mm and 3.0×23 mm Xience V stent, Abbott) were inserted in proximal and middle LAD, (C) LAO projection with cranial angulation of selective left CAG after LCX treatment showed intraluminal filling defect of the distal LAD (arrows), (D) After thrombus aspiration, infusion of glycoprotein IIb/IIIa receptor blocker and balloon angioplasty, CAG showed recovery of coronary flow.
CASE 2
A 83 year-old woman was referred to our hospital with complaints of dyspnea on exertion (New York Heart Association functional class III) from 1 month ago and hyponatremia with diuretic medication. Echocardiogra- phic examination showed hypokinesia of the anterior, inferolateral and inferior walls at base to mid-portion of
left ventricle. Under assessment of acute coronary synd- rome, the patient was treated aspirin 300 mg, clopidogrel 600 mg and intravenous nitroglycerin infusion. Also, unfractionated heparin was administered before PCI and at every hour during PCI with monitoring activated clotting time for the maintenance over 300 seconds. She underwent CAG which showed critical stenosis in the LAD and LCX (Fig. 4-A). Balloon angioplasty was done and
A B
C D
two Everolimus eluting stents (2.5×28 mm and 3.0×23 mm Xience V stent, Abbott) were inserted in the proximal and middle LAD at first (Fig. 4-B), followed by two more Everolimus eluting stents insertion in the proximal LCX.
After successful treatment with LCX artery, she com- plained of chest discomfort. CAG and intravenous ultrasonography (IVUS) revealed acute stent thrombosis in the mid-portion of LAD artery (Fig. 4-C). Thrombus aspiration and infusion of glycoprotein IIb/IIIa receptor blocker were done, and post-treatment CAG showed patent coronary flow (Fig. 4-D). After PCI, pulmonary edema disappeared and she showed the improvement of functional status. There were no predisposing factors including abnormal findings of coagulation system such as protein C or S, anti-phospholipid antibody and no evidence of malignancy. She was discharged with triple anti-platelet therapy using aspirin 100 mg, clopidogrel 75 mg, and cilostazol 200 mg daily. The patient was followed up via outpatient clinic without symptoms, repeat CAG after 9 months showed patent coronary flow.
DISCUSSION
Drug-eluting stents have reduced restenosis rates and the necessity for target-vessel revascularization. However, ST is still problematic. ST is a rare but catastrophic complication which frequently leads to death or myo- cardial infarction.
Recently, multiple risk factors associated with ST were reported. Especially, patients with STEMI, multi-vessel coronary artery disease, Killip class≥2 on admission, low left ventricular ejection fraction (EF), small stent diameter, long segmental stenosis and younger age are known to increase the risk of early ST.1,6 These two cases were examples of myocardial infarction with multi-vessel disease which received PCI on multi-vessel stenosis with poor Killip class.
For these cases, the physician should be alert to new
onset or aggravation of chest pain or sudden abnormal findings of vital signs. Immediate reexamination of coronary flow should be recommended even during or immediate after previous coronary angiography and PCI bearing in mind the possibility of acute stent thrombosis.
The most important thing for the diagnosis and treatment is clinical suspicion of acute stent thrombosis, which can be enough for the diagnosis and improve the prognosis of those patients. And multi-vessel PCI should be avoided if there was no derangement of symptom, sign of poor left ventricular function or pulmonary edema or the evidence of cardiogenic shock.
Currently the diagnostic and treatment strategies are not well defined. Emergent repeat PCI (thrombus aspi- ration, balloon dilatation) is commonly employed, and glycoprotein IIb/IIIa inhibitor is also used as ‘rescue’ therapy.
Glycoprotein IIb/IIIa inhibitor inhibited platelet aggre- gation and thrombus formation, and furthermore, induced lysis of fresh thrombus. In addition, treatment such as thrombus aspiration, intracoronary tirofiban injection has shown a favorable effect. The observational study conducted by Akhtar MM, et al showed that the combined use of thrombectomy with glycoprotein IIb/IIIa inhibitor improved outcome in patients with acute stent thrombosis.9
CONCLUSION
Acute ST during PCI was associated with multi-vessel disease, STEMI, and large thrombotic burden. Therefore, acute stent thrombosis can be successfully treated with thrombus aspiration, potent platelet aggregation inhibitor and balloon angioplasty.
REFERENCES
1. Aoki J, Lansky AJ, Mehran R, Moses J, Bertrand ME, McLaurin BT, et al. Early stent thrombosis in patients with
acute coronary syndromes treated with drug-eluting and bare metal stents: the Acute Catheterization and Urgent Intervention Triage Strategy trial. Circulation 2009;119:
687-698.
2. Daemen J, Wenaweser P, Tsuchida K, Abrecht L, Vaina S, Morger C, et al. Early and late coronary stent throm- bosis of sirolimus-eluting and paclitaxel-eluting stents in routine clinical practice: data from a large two-institu- tional cohort study. Lancet 2007;369:667-678.
3. Stone GW, Moses JW, Ellis SG, Schofer J, Dawkins KD, Morice MC, et al. Safety and efficacy of sirolimus- and paclitaxel-eluting coronary stents. N Engl J Med 2007;
356:998-1008.
4. Mauri L, Hsieh WH, Massaro JM, Ho KK, D'Agostino R, Cutlip DE. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med 2007;356:1020- 1029.
5. Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G, et al. Incidence, predictors, and outcome
of thrombosis after successful implantation of drug- eluting stents. JAMA 2005;293:2126-2130.
6. Park SH, Hong GR, Seo HS, Tahk SJ. Stent thrombosis after successful drug-eluting stent implantation. Korean Circ J 2005;35:163-171.
7. Park KW, Hwang SJ, Kwon DA, Oh BH, Park YB, Chae IH, et al. Characteristics and predictors of drug-eluting stent thrombosis: results from the multicenter 'Korea Stent Thrombosis (KoST)' registry. Circ J 2011;75:1626- 1632.
8. Beinart R, Abu Sham'a R, Segev A, Hod H, Guetta V, Shechter M, et al. The incidence and clinical predictors of early stent thrombosis in patients with acute coronary syndrome. Am Heart J 2010;159:118-124.
9. Akhtar MM, Jones DA, Gallagher S, Weerackody R, Sammut E, Rathod KS, et al. 035 Thrombectomy and platelet glycoprotein IIB/IIIA blockade for stent throm- bosis. Heart 2012;98:A22.