재활치료과학 제 10 권 제 2 호
Therapeutic Science for Rehabilitation Vol. 10. No. 2. 2021.
https://doi.org/10.22683/tsnr.2021.10.2.109
Cross-cultural Adaptation and Psychometric Evaluation
of the Korean Version of the A-ONE
Kang, Jaewon
*, M.S., O.T., Park, Hae Yean
**, Ph.D., O.T.,
Kim, Jung-Ran
***, Ph.D., O.T., Park, Ji-Hyuk
**, Ph.D., O.T.
*Dept. of Occupational Therapy, University of Florida, Doctoral Program, Student **
Dept. of Occupational Therapy, College of Software and Digital Healthcare Convergence, Yonsei University, Professor
***
Dept. of Dementia Prevention and Rehabilitation, College of Human Service, Catholic Kwandong University, Professor
Abstract
Objective : The purpose of this study was to develop a Korean version of the Activities of Daily Living (ADL)-focused Occupation-Based Neurobehavioral Evaluation (A-ONE) through cross-cultural adaptation and examine its validity and reliability.
Methods : This study translated the A-ONE into Korean and performed cross-cultural adaptation for the Korean population. After the development of the Korean version of the A-ONE, cross-cultural and concurrent validities were analyzed. Internal consistency, test-retest reliability, and inter-rater reliability were also evaluated. Results : We adapted three items to the Korean culture. The Korean version of the A-ONE showed high
cross-cultural validity with a content validity index (I-CVI) >0.9. It correlated with the Functional Independence Measure (FIM) (r=0.52–0.77, p<0.001), except for communication. Cronbach’s α was 0.58-0.93 for the functional independence scale (FI) and 0.42-0.93 for the neurobehavioral specific impairment subscale (NBSIS). Intraclass correlation coefficients (ICCs) indicated high test-retest and inter-rater reliability for FI (ICC=0.79-1.00 and 0.75-1.00, respectively) and NBSIS (ICC=0.74-1.00 and 0.72-1.00, respectively).
Conclusion : The Korean version of the A-ONE is well adapted to the Korean culture and has good validity and reliability. It is recommended to evaluate ADL performance skills and neurobehavioral impairments simultaneously in Korea.
Keywords : Activities of Daily Living (ADL), Cognition, Cross-cultural adaptation, Reliability, Stroke, Validity
교신저자 : 박지혁(otscientist@yonsei.ac.kr) || 접수일: 2020.05.02 || 심사일: 2020.05.21 || 게재승인일: 2020.09.04
Ⅰ. Introduction
Occupational therapists evaluate patients’ activities of daily living (ADL) performance skills to assess baseline abilities, set reasonable treatment goals, and examine functional changes after rehabilitation (Duffy, Gajree, Langhorne, Stott, & Quinn, 2013). Evaluating ADL is essential since a major goal of rehabilitation is usually to return home and resume independent living (Duffy et al., 2013). It is also important to evaluate neurobehavioral impairments, such as ideomotor apraxia, perseveration, or visuospatial disorder, that can impact ADL performance (Arnadottir, Lofgren, & Fisher, 2012). For example, ideomotor apraxia interferes with the ability to plan and perform typical behaviors, such as combing hair (Arnadottir, 1990; Arnadottir et al., 2012). As patients’ ADL performance skills vary with the neurobehavioral impairments, it is essential to select an appropriate evaluation tool (Arnadottir, 1990).
While various evaluation tools have been developed to assess ADL performance skills, such as the Functional Independence Measure (FIM) (Hamilton, Laughlin, Fiedler, & Granger, 1994), the Barthel Index (BI) (Mahoney & Barthel, 1965), and the Canadian Occupational Performance Measure (COPM) (Law et al., 1990), these tools do not evaluate neurobehavioral impairments concurrently with evaluating ADL performance skills. To increase ecological validity, it is important to assess ADL performance and neurobehavioral impairments (Arnadottir, 2010). Ecological validity can be good when performance on neurobehavioral evaluation administered in controlled settings is similar to performance in natural settings (Johnstone & Frank,
1995).
The ADL-focused Occupation-Based Neurobehavioral Evaluation (A-ONE) was developed to assess ADL performance skills and overall neurobehavioral impairments (Arnadottir, 1990). Occupational therapists observe and score patients in natural settings which increases ecological validity. The A-ONE consists of two scales: the Functional Independence (FI) scale identifies the level of ADL performance skills, while the Neurobehavioral (NB) scale evaluates neurobehavioral impairments. The A-ONE allows occupational therapists to make clinical decisions and select appropriate evidence- based interventions for patients (Arnadottir, Lofgren, & Fisher, 2010).
Although the A-ONE has advantages, it has not been used frequently in South Korea (Yoo, Jung, Park, & Choi, 2006). The A-ONE was originally developed in the United States by Gudrun Arnadottir, an Icelandic occupational therapist. However, cultural differences exist between Western and Korean cultures. Although an A-ONE training course has been held annually in South Korea, Korean occupational therapists could not use the A-ONE in clinical settings because some items do not apply to the Korean population. For example, one of the items, ‘use a knife’, is difficult to observe, especially in hospitals, as Korean usually use spoons and chopsticks as eating utensils. Since patients’ culture could influence ADL, assessment tools are recommended to conduct cross-cultural adaptation before use in other countries (Jia et al., 2016; Roy, Esculier, & Maltais, 2014). Furthermore, culturally adapted assessment tools are required to evaluate the psychometric properties, as well as conceptual and linguistic equivalence (Lohr, 2002).
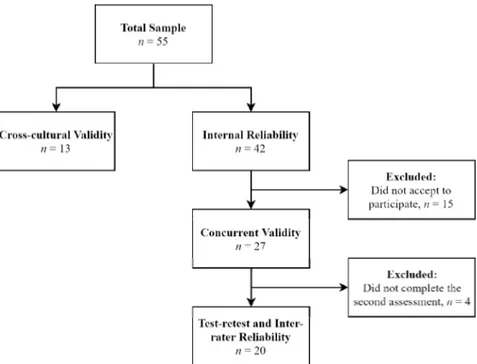
Figure 1. Flowchart of Participants in the Validity and Reliability Assessment The purpose of this study is to develop the Korean
version of the A-ONE through cross-cultural adaptation and to examine its validity and reliability.
Ⅱ. Methods
1. ParticipantsWe analyzed the validity and reliability of the Korean version of the A-ONE. Forty-two patients with stroke from a community health center and two rehabilitation hospitals in South Korea were included in this study (Table 1). We used the following inclusion criteria for the sample: (1) 20 years of age or older, (2) diagnosed with stroke, (3) onset at least three months prior to the study, (4) without dementia or scored≤20 on the Korean version of the Mini-Mental State Examination (MMSE-K) (Kwon, 1989), and (5) able to speak and
understand Korean. Exclusion criteria for the sample as follows: (1) fully dependent on assistance, and (2) had an unstable medical condition. We explained the purpose and study procedure to participants and asked them to provide written informed consent.
A further 13 individuals were recruited for cross-cultural validity. 12 out of 13 individuals completed the A-ONE training course and evaluated cross-cultural adaptation and linguistic understanding. We included one occupational therapy faculty who did not know the A-ONE to investigate the understanding of a non-expert. In this sample, 53.8% were occupational therapists, and 38.5% were occupational therapy faculty. Forty-six percent had 5-10 years of clinical experience. Figure 1 shows the flowchart of participants in the validity and reliability assessment. The study was approved by the Yonsei University Wonju Institutional Review Board (1041849-201701-BM-006-01).
2. Measures
1) The ADL-focused Occupation-Based Neurobehavioral Evaluation (A-ONE)
The A-ONE is a standardized tool that evaluates ADL performance and neurobehavioral impairments in patients with central nervous system dysfunction through direct observation. The FI of the A-ONE includes 22 items in five ADL domains: dressing, grooming and hygiene, transfers and mobility, feeding, and communication. Occupational therapists should prepare the ADL items before the assessment (e.g., a shirt, pants, socks, washcloth, comb, spoons). The following 5-category rating scale is used: 4=independent and able to transfer activity to other environmental situations; 3=independent with supervision; 2=requires verbal assistance; 1=requires demonstration or physical assistance; and 0=unable to perform/totally dependent on assistance.
The NB scale contains two sub-scales: the Neurobehavioral Specific Impairment Subscale (NBSIS) and Neurobehavioral Pervasive Impairment Subscale (NBPIS). The NBSIS contains 46 items (e.g., motor apraxia, spatial relations, and organization), and the NBPIS contains 31 items (e.g., anosognosia, lability, and impaired judgment). In this study, the NBSIS was used for the validity and reliability assessment. Each item in the NBSIS is rated using a 5-category rating scale: 0=no neurobehavioral impairments observed; 1=patient can perform without additional information, but there is neurobehavioral impairment; 2=patient can perform with additional verbal assistance, but there is neurobehavioral impairment during the performance; 3=patient can perform with a
demonstration or minimal to considerable physical assistance; and 4=patient cannot perform due to neurobehavioral impairment/needs maximum physical assistance. The A-ONE is not based on summed total scores because it aims to provide useful information for decision-making and to describe changes in scores rather than to identify differences in scores (Arnadottir, 2010).
The A-ONE showed high correlations between the FI and Barthel Index (BI) (r=0.85) and between the NB scale and MMSE (r=0.70). However, communication did not fit on a scale with ADL domains. The A-ONE also showed high inter-rater reliability (kappa=0.84) and the test-retest reliability (0.85) with a 1-week interval (Arnadottir, 1990; Arnadottir, 2010).
2) Functional Independence Measure (FIM) The FIM is an assessment tool to evaluate the level of an individual’s disability and the degree of assistance required to perform ADL (Hamilton et al., 1994). It contains 18 items (e.g., eating, grooming, bathing, upper body dressing, and memory). The total score ranges from 18 to 126. A higher score indicates a higher level of independence. According to Yoo et al. (2006), Korean occupational therapists use the FIM most frequently to evaluate ADL. In this study, we used the FIM to measure the concurrent validity of the FI of the Korean version of the A-ONE.
3) Lowenstein Occupational Therapy Cognitive Assessment (LOTCA)
The LOTCA was developed to evaluate cognition skills and visual perception in patients with neurological impairments (Katz, Itzkovich, Averbuch, & Elazar, 1989). The subscales include
Figure 2. The Process of Translation and Cross-cultural Adaptation orientation, perception, visuomotor organization,
and thinking operation, which are scored separately. The total score ranges from 21 to 91. A higher score indicates less cognitive impairment. The LOTCA is also one of the most frequently used cognitive assessment tools in Korean clinical settings (Yoo et al., 2006). As neurobehavioral impairments are highly related to cognitive impairments (Conti, 2017), the LOTCA was selected to evaluate the concurrent validity of the NB scale of the Korean version of the A-ONE.
4) The Korean version of Mini-Mental State Examination (MMSE-K)
The MMSE-K has commonly used to screen cognitive impairments in Korea. It consists of 30 questions about orientation in time and place, memory registration/recall, attention/calculation, language, and visuospatial function. A total score of
<20 is considered a cognitive impairment (Kwon, 1989). In this study, we used the MMSE-K to screen patient samples.
3. Procedures
1) Translation and cross-cultural adaptation After receiving consent from the author of the original version, we conducted translation and cross-cultural adaptation. This study modified the international guidelines for cross-cultural adaptation due to the absence of a gold standard (Beaton, Bombardier, Guillemin, & Ferraz, 2000; Epstein, Santo, & Guillemin, 2015). The first stage was a forward translation (T1 and T2) by two translators. They translated English into Korean. T1 and T2 were synthesized into one consensual version (T-12). A bilingual translator translated T-12 back into English (BT-1). Next, the author of the original
version reviewed BT-1 to investigate whether the Korean version of the A-ONE is linguistically equivalent to the original version of the A-ONE.
After the original authors’ review, we conducted a pilot test to evaluate cultural adequacy. As the A-ONE is not a patient-reported assessment, we included six occupational therapists and an occupational therapy faculty for the pilot test. At the next stage, an expert committee reviewed all reports. The committee consisted of three occupational therapists and two occupational therapy faculty, who work at the Korean A-ONE Research Association. The committee produced the final version with the cross-cultural adaptations (Figure 2).
2) Validity and reliability assessment of the Korean version of the A-ONE
After translation and cross-cultural adaptation of the Korean version of the A-ONE, we analyzed cross-cultural validity. Thirteen individuals evaluated each item, considering cultural adequacy. They used the following 4-category rating scale: 4=very relevant, 3=relevant, 2=not relevant, and 1=never relevant.
An occupational therapist (OT1) evaluated 42 patients using the final version of the Korean version of the A-ONE. OT1 did not observe four items related to toileting and bathing due to privacy. 27 out of 42 patients agreed to participate in additional assessments, the FIM and LOTCA. Internal consistency was calculated using data from 42 patients with stroke. Twenty-seven patients were included for the concurrent validity assessment. For test-retest reliability, OT1 evaluated twenty patients twice, with a 1-week interval between each
evaluation. For inter-rater reliability, another occupational therapist (OT2) evaluated the same 20 patients by watching videos recorded by OT1. Prior to the study, OT1 and OT2 completed five-day A-ONE training courses to practice reasoning, administration, and scoring from the original author of the A-ONE.
4. Statistical analysis
Descriptive statistics were used to analyze the demographic characteristics of the patient sample. For cross-cultural validity, the content validity index (I-CVI) was calculated at the item level. The I-CVI typical formula is the number of raters giving a rating of 3 or 4 divided by the total number of raters. When using more than ten experts, I-CVI scores of 0.78 and above are considered the minimum acceptable indices (Polit, Beck, & Owen, 2007). All items should be revised and re-evaluated until the minimum acceptable indices are achieved (Sousa & Rojjanasrirat, 2011). We conducted Pearson correlations to evaluate the concurrent validity of the FI and the NB scales. Correlations were categorized as high (≥0.70), moderate (0.50–0.69), and low (0.26–0.49) (Carter & Lubinsky, 2015). Internal consistency was calculated using Cronbach’s α with values of >0.70 considered acceptable (Ursachi, Horodnic, & Zait, 2015). The intraclass correlation coefficient (ICC) was used to estimate test-retest and inter-rater reliability. The ICC values were classified as excellent (>0.90), good (0.74–0.90), moderate (0.50–0.75), and poor (<0.50) (Koo & Li, 2016). All analyses were conducted using SPSS Statistics ver. 23, with the significance level set at p<0.05.
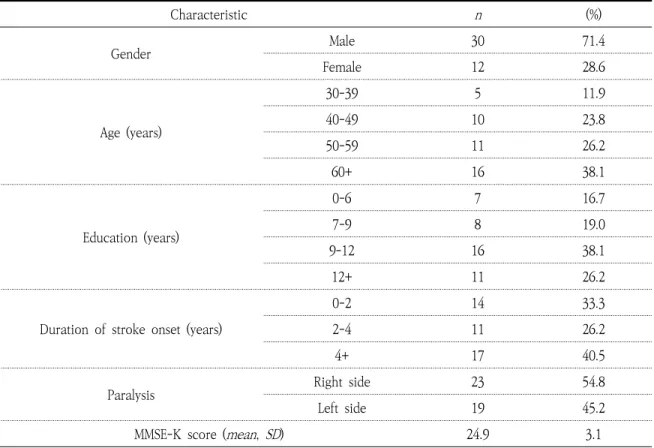
Characteristic n (%) Gender Male 30 71.4 Female 12 28.6 Age (years) 30-39 5 11.9 40-49 10 23.8 50-59 11 26.2 60+ 16 38.1 Education (years) 0-6 7 16.7 7-9 8 19.0 9-12 16 38.1 12+ 11 26.2
Duration of stroke onset (years)
0-2 14 33.3
2-4 11 26.2
4+ 17 40.5
Paralysis Right side 23 54.8
Left side 19 45.2
MMSE-K score (mean, SD) 24.9 3.1
MMSE-K=The Korean version of Mini-Mental State Examination
Table 1. Demographic Characteristics (N=42)
Ⅲ. Results
1. Demographic characteristicsForty-two patients with stroke were recruited for this study. 71.4% were male, and the mean age was 54.8 (SD=12.2) years old with the range of 30-75 years. The average duration of stroke onset was 6.2 (SD=9.4) years. 23 out of 42 patients were paralyzed on the right side of the body. On average, patients scored 24.9 (SD=3.1) on the MMSE-K, ranging from 20 to 30 (Table 1).
2. Cross-cultural adaptation
Three items, ‘Washing face and upper body’,
‘Using fingers (sandwich)’ and ‘Using a knife’ were modified based on cultural adequacy. Among five domains, feeding underwent the most modifications based on Korean culture. For example, a knife is commonly used as an eating utensil in Western culture. However, spoons and chopsticks are commonly used in Korea. Also, Kim (roasted seaweed) and Ssam (lettuce wraps) are more familiar to Koreans of all ages when they eat foods with their hands rather than a sandwich (Table 2). Additionally, ‘Continence/toilet’ was changed into ‘Performing toilet hygiene’ because the original author requested that the word for function needs to be replaced with the term for ADL. Committee members concluded that NB might not be affected by culture, so that there was no cultural adaptation in NB.
Original version Korean version Reason for modification 1 Wash face and upper body
(with washcloth) Washing face
Koreans usually wash their face and hands without a washcloth. 2 Use fingers-Sandwich Using fingers-Kim (roasted seaweed)
and Ssam (lettuce wraps)
Koreans of all ages are more familiar with Kim and Ssam than sandwiches.
3 Use knife Using Chopsticks Koreans usually use chopsticks
when they eat.
Table 2. Modifications After Cross-Cultural Adaptation
Domain Pearson correlation (r)
FIM
Dressing 0.53**
Grooming and hygiene 0.52**
Transfers and mobility 0.71**
Feeding 0.77**
Communication 0.17
**
p<.01; FIM=Functional Independence Measure
Table 3. Concurrent Validity With the FIM (N=27)
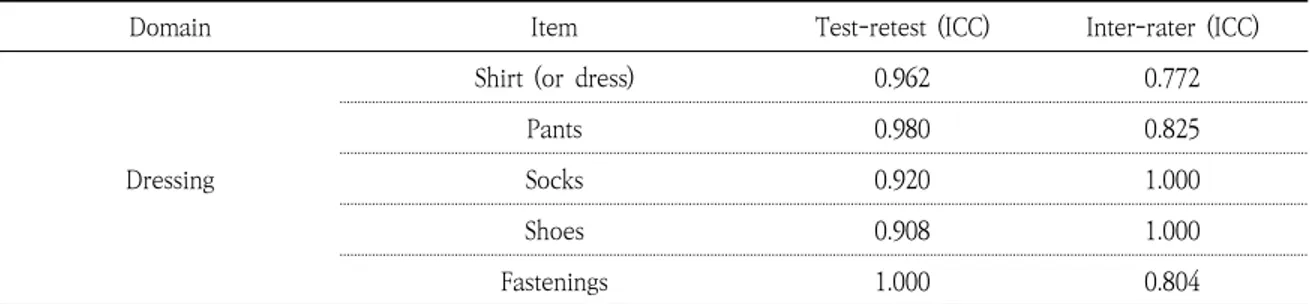
Domain Item Test-retest (ICC) Inter-rater (ICC)
Dressing
Shirt (or dress) 0.962 0.772
Pants 0.980 0.825
Socks 0.920 1.000
Shoes 0.908 1.000
Fastenings 1.000 0.804
Table 4. Reliability of the Korean Version of the A-ONE in the FI (N=20)
3. Validity
The results of I-CVI comparisons across all categories of the FI ranged from 0.92 to 1. The Korean version of the A-ONE showed a significantly high concurrent validity with the FIM (r=0.52–0.77, p<0.01), except for the communication domain (r=0.17, p>0.05) (Table 3). However, only three items, ‘Abnormal tone: Left’, ‘Perseveration’ and ‘Dysarthria’, in the NBSIS showed significant
correlations with the LOTCA.
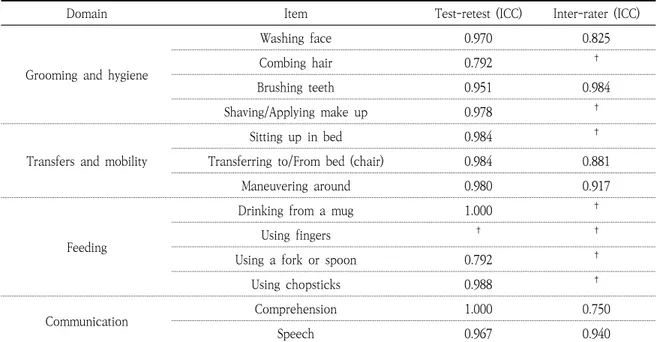
4. Reliability
Cronbach’s α for the total patient sample ranged from 0.58 to 0.93 for the FI and 0.42 to 0.93 for the NBSIS, suggesting acceptable internal consistency. The Korean version of the A-ONE showed good test-retest reliability (ICC=0.79–1.00 for the FI, ICC=0.74–1.00 for the NBSIS) and inter-rater
Domain Item Test-retest (ICC) Inter-rater (ICC)
NBSIS
Motor apraxia 0.737 0.812
Ideational apraxia 1.000 0.750
Unilateral body neglect 0.977 0.750
Somatoagnosia 1.000 †
Spatial relations 0.978 0.723
Unilateral spatial neglect 1.000 †
Abnormal tone: Right 0.899 0.818
Abnormal tone: Left 0.952 0.750
Perseveration 0.964 †
Organization/Sequencing 0.772 0.812
Topographical disorientation 0.792 0.791
Wernicke’s aphasia/Sensory aphasia 0.750 1.000
Jargon aphasia 0.912 †
Anomia 0.792 †
Paraphasia 0.792 †
Broca’s aphasia/Expressive aphasia 1.000 †
Dysarthria 0.853 0.818
†
ICC cannot be calculated due to the lack of observations; ICC=Intraclass correlation coefficient; NBSIS=Neurobehavioral specific impairment subscale
Table 5. Reliability of the Korean Version of the A-ONE in the NBSIS (N=20)
Domain Item Test-retest (ICC) Inter-rater (ICC)
Grooming and hygiene
Washing face 0.970 0.825
Combing hair 0.792 †
Brushing teeth 0.951 0.984
Shaving/Applying make up 0.978 †
Transfers and mobility
Sitting up in bed 0.984 †
Transferring to/From bed (chair) 0.984 0.881
Maneuvering around 0.980 0.917
Feeding
Drinking from a mug 1.000 †
Using fingers † †
Using a fork or spoon 0.792 †
Using chopsticks 0.988 †
Communication Comprehension 1.000 0.750
Speech 0.967 0.940
†
ICC cannot be calculated due to the lack of observations; FI=Functional independence; ICC=Intraclass correlation coefficient
reliability (ICC=0.75–1.00 for the FI, ICC=0.72–1.00 for the NBSIS) (Table 4 and Table 5).
Ⅳ. Discussion
This study aimed to conduct a cross-cultural adaptation of the A-ONE and examine the validity and reliability of the Korean version. We developed the Korean version of the A-ONE through translation and cultural adaptation to Korean culture. The Korean version of the A-ONE showed good validity and reliability in Korean stroke patients.
Through the cross-cultural adaptation, three items are modified based on cultural differences. Among five domains in the A-ONE, the feeding domain displayed the most cultural differences between Western and Korean cultures. For example, we modified ‘Use knife’ into ‘Use Chopsticks’ because Korean usually use Chopsticks as an eating utensil. We also changed ‘Use fingers (sandwich)’ into ‘Use fingers (Kim or Ssam)’. Those Korean foods are more familiar to Koreans of all ages, especially older people. When researchers conduct the cross-cultural adaptation, they should consider all age groups.
Occupational therapists and occupational therapy faculty evaluated the cross-cultural validity of the Korean version of the A-ONE. The results showed an excellent cross-cultural validity, indicating that all items reflect Korean culture well. Also, the Korean version of the A-ONE showed a good concurrent validity with the FIM, excluding communication. Low correlation in communication might be explained by the fact that the FIM evaluated communication skills considering the use of assistive devices, such as hearing aids, while the
A-ONE evaluated communication skills focusing on physical or verbal assistance. The Korean version of the A-ONE showed a low correlation with the LOTCA. The reason is that LOTCA focuses more on task-oriented items, such as shape identification, pegboard construction, and symbolic action, while the A-ONE focuses more on ADL performance (Kang, 2017). These differences result in a low correlation between the two assessment tools. It is important to evaluate neurobehavioral impairments or cognitive impairments by observing patients performing ADL (Hodges, Kirsch, Newman, & Pollack, 2010). Hodges et al. (2010) used sensor-collected data to evaluate cognitive impairments while individuals performed ADL, such as making coffee. This assessment may show a higher correlation to the Korean version of the A-ONE because both assessments are conducted in a natural setting.
Internal consistency showed moderate-to-good reliability that was similar to the results of the original version of the A-ONE (ICC=0.85) (Arnadottir, 1990). The NBSIS showed lower internal consistency than the FI. The level of neurobehavioral impairments varies between different ADL (Arnadottir, 1990). For example, impairment of spatial relations might be detected while walking but not while eating. This may result in lower internal consistency. Test-retest reliability of the Korean version of the A-ONE was as good as that of the original version of the A-ONE (Arnadottir, 1990). Although two raters in the inter-rater reliability had different years of clinical experience (OT1 had less than one year of clinical experience, while OT2 had ten years of clinical experience), the Korean version of the A-ONE showed good inter-rater reliability.
The A-ONE training course that both raters completed may explain the inter-rater reliability, suggesting that the Korean version of the A-ONE is reliable when it is scored by an occupational therapist who receives formal training.
This study has several limitations. First, our sample does not represent the entire Korean population since they were recruited in two specific cities, Seoul and Wonju, South Korea. Further research should include patients from diverse clinical settings. Second, there is no variety of disease groups. All patients in this study were diagnosed with a stroke. The A-ONE was originally developed to assess individuals with a variety of central nervous system dysfunctions, such as vascular disorders, metabolic disorders, and head injuries. Thus, further studies should include patients with diverse diseases, including dementia, multiple sclerosis, and Parkinson’s disease. Moreover, further psychometric evaluations using factor analysis, Rasch analysis, or item response theory (IRT) are encouraged to ensure the validity and reliability of the Korean version of the A-ONE.
Ⅴ. Conclusion
This study provides evidence that the Korean version of the A-ONE was well adapted to Korean culture and had good validity and reliability in Korean stroke patients. With trained occupational therapists, the Korean version of the A-ONE can be used to evaluate ADL performance skills and overall neurobehavioral impairments simultaneously in Korean stroke patients.
References
Arnadottir, G. (1990). The brain and behavior: Assessing cortical dysfunction through activities of daily living (ADL). St. Louis: Mosby Elsevier.
Arnadottir, G. (2010). Measuring the impact of body functions on occupational performance: Validation of the ADL-focused Occupation-based Neurobehavioral Evaluation (A-ONE) (Doctoral dissertation). Umea university, Umea.
Arnadottir, G., Lofgren, B., & Fisher, A. G. (2010). Difference in impact of neurobehavioural dysfunction on activities of daily living performance between right and left hemispheric stroke. Journal of Rehabilitation Medicine, 42(10), 903–907. doi:10. 2340/16501977-0621
Arnadottir, G., Lofgren, B., & Fisher, A. G. (2012). Neurobehavioral functions evaluated in naturalistic contexts: Rasch analysis of the A-ONE neurobehavioral impact scale. Scandinavian Journal of Occupational Therapy, 19(5), 439–449. doi:10. 3109/11038128.2011.638674
Beaton, D. E., Bombardier, C., Guillemin, F., & Ferraz, M. B. (2000). Guidelines for the process of cross-cultural adaptation of self-report measures. Spine, 25(24), 3186–3191.
Carter, R., & Lubinsky, J. (2015). Statistical analysis of relationships: The basics. In Carter, R., & Lubinsky, J. (Eds.), Rehabilitation research: Principles and applications (5th ed., pp. 318-325). St. Louis: Mosby Elsevier.
Conti, J. (2017). Cognitive assessment: A challenge for occupational therapists in Brazil. Dementia & Neuropsychologia, 11(2), 121–128. doi:10.1590/1980- 57642016dn11-020004
Duffy, L., Gajree, S., Langhorne, P., Stott, D. J., & Quinn, T. J. (2013). Reliability (Inter-rater Agreement) of the Barthel Index for Assessment of stroke survivors: Systematic review and meta-analysis. Stroke, 44(2), 462–468. doi:10.1161/STROKEAHA.112.678615 Epstein, J., Santo, R. M., & Guillemin, F. (2015). A review
of guidelines for cross-cultural adaptation of questionnaires could not bring out a consensus. Journal of Clinical Epidemiology, 68(4), 435–441. doi:10.1016/j.jclinepi.2014.11.021
Hamilton, B. B., Laughlin, J. A., Fiedler, R. C., & Granger, C. V. (1994). Interrater reliability of the 7-level functional independence measure (FIM). Scandinavian Journal of Rehabilitation Medicine, 26(3), 115–119.
Hodges, M. R., Kirsch, N. L., Newman, M. W., & Pollack, M. E. (2010). Automatic assessment of cognitive impairment through electronic observation of object usage. In Floroen P., Kruger A., Spasojevic M. (Eds.), Pervasive computing (8th ed., pp. 192–209). New York: Springer. doi:10.1007/978-3-642-12654-3_12 Jia, Z. Y., Wang, W., Nian, X. W., Zhang, X. X., Huang, Z.,
Cui, J., & Xu, W. D. (2016). Cross-cultural adaptation and validation of the simplified Chinese version of the knee outcome survey activities of daily living scale. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 32(10), 2009–2016. doi:10.1016/j. arthro.2016.01.068
Johnstone, B., & Frank, R. G. (1995). Neuropsychological assessment in rehabilitation: Current limitations and applications. NeuroRehabilitation, 5(1), 75–86. doi:10.3233/NRE-1995-5107
Kang, J. (2017). Validity and reliability of the cross- culturally adapted the Korean version of the ADL-focused occupation-based neurobehavioral evaluation (A-ONE) (Master’s thesis). Yonsei University, Seoul.
Katz, N., Itzkovich, M., Averbuch, S., & Elazar, B. (1989). Loewenstein Occupational Therapy Cognitive Assessment (LOTCA) battery for brain-injured patients: Reliability and validity. American Journal of Occupational Therapy, 43(3), 184–192. doi:10.5014/ ajot.43.3.184
Koo, T. K., & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15(2), 155–163. doi:10.1016/j.jcm.2016.02.012 Kwon, Y. C. (1989). Korean version of mini-mental state
examination (MMSE-K). Journal of the Korean Neurological Association, 28(1), 123–135.
Law, M., Baptiste, S., McColl, M., Opzoomer, A., Polatajko, H., & Pollock, N. (1990). The Canadian Occupational Performance Measure: An outcome measure for occupational therapy. Canadian Journal of Occupational Therapy, 57(2), 82-87. doi:10.1177/ 000841749005700207
Lohr, K. N. (2002). Assessing health status and quality-of-life instruments: Attributes and review criteria. Quality of Life Research, 11(3), 193–205. Mahoney, F. I., & Barthel, D. W. (1965). Functional
evaluation: The Barthel Index: A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Maryland State Medical Journal, 14, 61–65.
Polit, D. F., Beck, C. T., & Owen, S. V. (2007). Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Research in Nursing & Health, 30(4), 459–467. doi:10.1002/nur.20199
Roy, J. S., Esculier, J. F., & Maltais, D. B. (2014). Translation, cross-cultural adaptation and validation of the French version of the knee outcome survey–activities of daily living scale. Clinical Rehabilitation, 28(6), 614 –623. doi:10.1177/0269215513511342
Sousa, V. D., & Rojjanasrirat, W. (2011). Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline: Validation of instruments or scales. Journal of Evaluation in Clinical Practice, 17(2), 268–274. doi:10.1111/j.1365-2753.2010.01434.x Ursachi, G., Horodnic, I. A., & Zait, A. (2015). How reliable
are measurement scales? External factors with indirect influence on reliability estimators. Procedia Economics and Finance, 20, 679-686. doi:10.1016/ S2212-5671(15)00123-9
Yoo, E. Y., Jung, M. Y., Park, S. Y., & Choi, E. H. (2006). Current trends of occupational therapy assessment tool by Korean occupational therapist. The Journal of Korean Society of Occupational Therapy, 14(3), 27–37.
국문초록
한국판 일상생활활동중심 작업기반 신경행동평가(A-ONE)의
개발 및 평가
강재원
*, 박혜연
**, 김정란
***, 박지혁
** *플로리다대학교 작업치료학과 박사과정 ** 연세대학교 소프트웨어디지털헬스케어융합대학 작업치료학과 교수 ***가톨릭관동대학교 휴먼서비스대학 치매전문재활학과 교수 목적 : 본 연구는 타문화권에서 개발된 일상생활활동중심 작업기반 신경행동평가(A-ONE)를 국내 임상에 서 사용할 수 있도록 한국판을 개발하고 한국 환자에게 적용하여 신뢰도와 타당도를 검증하고자 하였다. 연구방법 : 영문판 A-ONE을 한국어로 번역하고 문화적 차이를 검토하였다. 완성된 한국판을 13명의 작업치료학과 교수와 작업치료사에게 국내 적용 가능성을 확인받고, 뇌졸중 환자 42명을 대상으로 신뢰도와 타당성을 검증하였다.결과 : 총 3개의 문항을 국내 문화에 알맞도록 수정한 결과, 한국판 A-ONE은 Index at the item level(I-CVI)=0.92-1.00을 보이며 평가 문항들이 국내 문화를 잘 대표하고 있는 것으로 나타났다. Functional Independence Measure(FIM)과 상관관계는 의사소통영역을 제외하고 r=0.52-0.77(p>0.01) 로 높게 나타난 반면, Lowenstein Occupational Therapy Cognitive Assessment(LOTCA)와는 전반적으
로 유의미한 상관관계를 보이지 않았다(p>0.05). 내적일치도는 기능적 독립성이 Cronbach’s α
=0.58-0.93, 신경행동손상이 α=0.42-0.93을 보였다. 검사-재검사 신뢰도는 기능적 독립성이 Intraclass correlation coefficient(ICC)=0.79-1.00, 신경행동손상이 ICC=0.74-1.00으로 높은 수준을 보였다. 마지 막으로, 검사자간 신뢰도는 기능적 독립성이 ICC=0.75-1.00, 신경행동손상이 ICC=0.72-1.00으로 높은 신뢰도를 보였다.
결론 : 한국판 A-ONE은 뇌졸중 환자의 일상생활활동 수행능력과 신경행동손상의 종류 및 손상정도를 평가하기 위해 국내 임상에서 사용될 수 있는 유용한 평가도구이다.
A-ONE PartⅠ
기능적 독립성 척도와 특정 신경행동손상 하위척도 이름 날짜 독립성 점수 (IP) : 신경행동 점수 (NB) : 4 = 독립적이고 다른 환경의 상황에서 활동 전이 가능 0 = 신경행동학적 오류가 관찰되지 않음 3 = 감독 하에 독립적 1 = 약간의 신경행동학적 오류가 관찰되지만, 추가적인 도 움이나 정보 없이 수행 가능함 2 = 언어적 도움 필요 2 = 수행 시 신경행동학적 오류가 관찰되지만 추가적인 언 어적 도움 하에 수행 가능함 1 = 시연 또는 신체적 도움 필요 0 = 수행 불가. 도움에 완전히 의존 3 = 시연 또는 신체적 도움 (최소한의 도움에서 상당한 도움 까지 포함) 하에 수행 가능함 사용된 보조도구 목록 : 4 = 신경행동손상 때문에 수행 불가능함. 최대 신체적 도움 필요기본 ADL 활동 점수 의견 및 이유 옷 입기 독립성 점수 (IP) 셔츠(또는 원피스) 4 3 2 1 0 바지 4 3 2 1 0 양말 4 3 2 1 0 신발 4 3 2 1 0 옷 잠금장치(단추, 지퍼, 신발 끈 등) 4 3 2 1 0 그 밖의 활동 신경행동 손상 신경행동 점수 (NB) 운동실행증 0 1 2 3 4 관념실행증 0 1 2 3 4 편측 신체 무시 0 1 2 3 4 신체실인증 0 1 2 3 4 공간관계 0 1 2 3 4 편측 공간 무시 0 1 2 3 4 비정상적인 긴장도: 오른쪽 0 1 2 3 4 비정상적인 긴장도: 왼쪽 0 1 2 3 4 보속증 0 1 2 3 4 조직화/순서화 0 1 2 3 4 그 밖의 손상 기본 ADL 활동 점수 의견 및 이유 몸단장 및 위생 독립성 점수 (IP) 세수하기 4 3 2 1 0 머리 빗기 4 3 2 1 0 이 닦기 4 3 2 1 0 면도하기/로션 바르기 4 3 2 1 0 화장실 위생 4 3 2 1 0 목욕하기 4 3 2 1 0 그 밖의 활동 4 3 2 1 0 신경행동 손상 신경행동 점수 (NB) 운동실행증 0 1 2 3 4 관념실행증 0 1 2 3 4 편측 신체 무시 0 1 2 3 4 신체실인증 0 1 2 3 4 공간관계 0 1 2 3 4 편측 공간 무시 0 1 2 3 4 비정상적인 긴장도: 오른쪽 0 1 2 3 4 비정상적인 긴장도: 왼쪽 0 1 2 3 4 보속증 0 1 2 3 4 조직화/순서화 0 1 2 3 4 그 밖의 손상 기능적 독립성 척도와 특정 신경행동손상 하위척도 계속 :
기본 ADL 활동 점수 의견 및 이유 이동하기 독립성 점수 (IP) 침대에서 일어나 앉기 4 3 2 1 0 침대(또는 의자)로 이동하기 4 3 2 1 0 주변 돌아다니기 4 3 2 1 0 변기로 옮겨 앉기 4 3 2 1 0 욕조 또는 샤워부스로 이동하기 4 3 2 1 0 그 밖의 활동 신경행동 손상 신경행동 점수 (NB) 운동실행증 0 1 2 3 4 관념실행증 0 1 2 3 4 편측 신체 무시 0 1 2 3 4 공간관계 0 1 2 3 4 편측 공간 무시 0 1 2 3 4 비정상적인 긴장도: 오른쪽 0 1 2 3 4 비정상적인 긴장도: 왼쪽 0 1 2 3 4 보속증 0 1 2 3 4 조직화/순서화 0 1 2 3 4 공간배열 지남력장애 0 1 2 3 4 그 밖의 손상 기본 ADL 활동 점수 의견 및 이유 식사하기 독립성 점수 (IP) 컵 사용하여 마시기 4 3 2 1 0 손가락 사용하여 먹기/김 또는 쌈 싸먹기 4 3 2 1 0 숟가락 또는 포크 사용하여 먹기 4 3 2 1 0 젓가락 사용하여 먹기 4 3 2 1 0 그 밖의 활동 신경행동 손상 신경행동 점수 (NB) 운동실행증 0 1 2 3 4 관념실행증 0 1 2 3 4 편측 신체 무시 0 1 2 3 4 공간관계 0 1 2 3 4 편측 공간 무시 0 1 2 3 4 비정상적인 긴장도: 오른쪽 0 1 2 3 4 비정상적인 긴장도: 왼쪽 0 1 2 3 4 보속증 0 1 2 3 4 조직화/순서화 0 1 2 3 4 그 밖의 손상 기능적 독립성 척도와 특정 신경행동손상 하위척도 계속 :
기본 ADL 활동 점수 의견 및 이유 의사소통 독립성 점수 (IP) 이해력 4 3 2 1 0 언어능력 4 3 2 1 0 신경행동 손상 신경행동 점수 (NB) (0=손상 없음, 1=손상 있음) 베르니케실어증/감각성실어증 0 1 착각성실어증 0 1 명칭실어증 0 1 착어증 0 1 보속증 0 1 브로카실어증/표현실어증 0 1 구음장애(말더듬증) 0 1 그 밖의 손상 0 1 기능적 독립성 척도와 특정 신경행동손상 하위척도 계속 : 그 밖의 손상 ADL 의견 : 운동실행증 관념실행증 편측 신체 무시 신체실인증 공간관계 편측 공간 무시 비정상적인 긴장도: 오른쪽 비정상적인 긴장도: 왼쪽 보속증 조직화 공간배열 지남력장애 그 밖의 손상 베르니케실어증/감각성 실어증 착각성실어증 명칭실어증 착어증 브로카실어증/표현실어증 그 밖의 (언어적) 손상 관찰된 신경행동손상 목록 :
기능적 독립성 점수 (선택) 기능 총점 % 점수 옷 입기 몸단장 및 위생 이동하기 식사하기 의사소통 치료 고려 사항 : 작업치료사 : A-ONE 인증 번호 :
A-ONE PartⅠ
전반적 신경행동손상 하위척도 이름 날짜 점수기준 : 한군데만 동그라미(○) 하세요 0 = 손상 없음 1 = 손상 있음 전반적인 징후는 매뉴얼에 제시된 구체적인 지침에 따라 ADL 영역의 어느 한군데서라도 관찰되거나 기록될 수 있습니다. 신경행동손상 신경행동 점수 (NB) 의견 및 이유 실인증 1. 촉각/입체실인증: 우측/좌측 0 1 2. 운동지속불능증 0 1 3. 시각적 물체실인증 0 1 4. 시각적 공간실인증 0 1 5. 연합성 시각실인증 0 1 6. 질병불각증 0 1 신체도식장애 1. 오른쪽/왼쪽 방향감각상실 0 1 2. 신체부분식별 0 1 감정적/정서적 장애 1. 불안정성 0 1 2. 행복감 0 1 3. 무관심 0 1 4. 우울감 0 1 5. 공격성 0 1 6. 짜증남(언짢음) 0 1 7. 좌절감 0 1 8. 안절부절 못 함 0 1 인지적 장애 1. 경직된(구체적) 사고 0 1 2. 자기인식(통찰력) 감소 0 1 3. 판단력 손상 0 1 4. 혼란 0 1신경행동손상 신경행동 점수 (NB) 의견 및 이유 그 밖의 장애 1. 각성장애 0 1 2. 집중력장애 0 1 3. 주의산만 0 1 4. 결단력장애 0 1 5. 동기부여장애 0 1 6. 수행지연 0 1 7. 사고부재(넋 잃음) 0 1 8. 기억력 장애 1. 단기기억력 상실 0 1 2. 장기기억력 상실 0 1 3. 지남력장애 0 1 4. 작화 0 1 전반적 신경행동손상 하위척도 계속 : 요 약 :