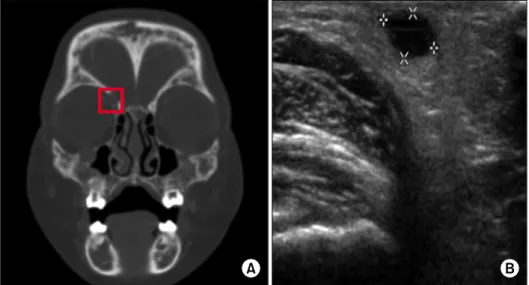
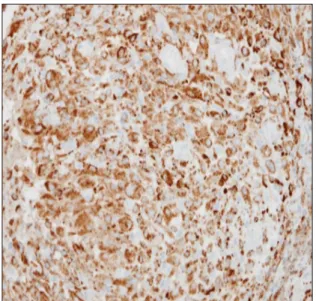
소아 백혈병 환자에서 치료 중 발생한 에드하임-체스터 병
홍준표ㆍ안원기ㆍ임주연ㆍ정조은ㆍ한승민ㆍ한정우ㆍ유철주
전체 글
홍준표ㆍ안원기ㆍ임주연ㆍ정조은ㆍ한승민ㆍ한정우ㆍ유철주
수치
관련 문서
It considers the energy use of the different components that are involved in the distribution and viewing of video content: data centres and content delivery networks
After first field tests, we expect electric passenger drones or eVTOL aircraft (short for electric vertical take-off and landing) to start providing commercial mobility
In this group of high-risk patients with severe COVID-19 pneumonia, treatment with lenzilumab was associated with a significantly shorter time to clinical improvement compared
1 John Owen, Justification by Faith Alone, in The Works of John Owen, ed. John Bolt, trans. Scott Clark, "Do This and Live: Christ's Active Obedience as the
The purpose of the present study was to elucidate the effect of photography and reporting activities conducted at a day care center on 5-year-old
- distributes indexes across multiple computers and/or multiple sites - essential for fast query processing with large numbers of documents - many variations:
Perspectives on allogeneic hematopoietic stem cell transplantation in Myeloma..
3) A comparison of the stoichiometric equation with the experimental kinetic expression can suggest whether or not we are dealing with an elementary reaction. 4) If one