저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다.
Master's Thesis in Medicine
Effectiveness of acellular dermal matrix on autologous
split-thickness skin graft in treatment of deep tissue
defect : Does cograft affect outcomes?
Ajou University Graduate School
Major in Medicine
Effectiveness of acellular dermal matrix
on autologous split-thickness skin graft
in treatment of deep tissue defect
: Does cograft affect outcomes?
Il Jae Lee, M.D., Ph.D., Advisor
I submit this thesis as theMaster's thesis in Medicine.
February 2017
Ajou university Graduate School
Major in Medicine
The Master's thesis of Yoo Jung Lee in Medicine is
hereby approved.
Thesis Defense Committee President
Il Jae Lee
MemberYoung Uk Park
Member Han Bum Joe
Ajou University Graduate School
January 4th, 2017
i
ABSTRACT
Background: A split-thickness skin graft is usually performed to cover a large full-thickness skin defect.
Aesthetic and functional deficits can result, and many studies have sought to overcome them. This study compared the effectiveness of the acellular dermal matrix(ADM) graft and split-thickness skin graft concerning aesthetic and functional effectiveness of ADM on scar quality of the donor site of anterolateral thigh free flap compared to split thickness skin graft only.
Methods: Of the patients who underwent anterolateral thigh free flap defect coverage from 2011 to 2015 at
our institution, patients who received skin graft only(n=10) or skin graft with ADM(n=20) for coverage of the donor site were enrolled. The retrospective study reviewed medical records and clinical photos to
investigateearly outcome (skin loss rate, duration of negative-pressure wound therapy);days to removal of stitches; days to achieve complete healing; complications;days from surgery to the start of rehabilitation); late outcomesin terms ofscar vascularity, pigmentation, pliability and height; and graft-related itching sensation and pain. Assessments used the Vancouver Scar Scale (VSS) and patient scar assessment scale of the Patient and Observer Scar Assessment Scale (POSAS). Skin fold was measured to evaluate the elasticity of scar tissue.
Results:There was no statistically difference in sex, age, underlying disease, defect size, and the early
outcomes between two groups. The VSS vascularity subscore(p=0.003) and total score(p=0.016) were
significantly lower in the skin graft with ADM group. POSAS pain(p=0.037) and stiffness subscore(p=0.002), and total score(p=0.017) were significantly lower in the skin graft with ADM group.
Conclusions: ADM applied to a full-thickness skin defect could result in a better scar quality. Delay in graft
take could be compensated by negative-pressure wound therapy at the skin graft site.
Keywords: acellular dermal matrix, skin graft, Vancouver Scar scale, Patient and Observer Scar Assessment
ii
TABLE
OF
CONTENTS
LIST OF TEXT
ABSTRACT∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙i TABLE OF CONTENTS∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ii I. INTRODUCTION∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙1 II. METHODS∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ 2 III.RESULTS∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙4 IV.DISCUSSION∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙11 V.CONCLUSION∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙14 REFERENCES∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙15 국문요약∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙18LIST
OF
FIGURES
FIGURE 1.Two donor sites of the anterolateral thigh flap.∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙10
LIST
OF
TABLES
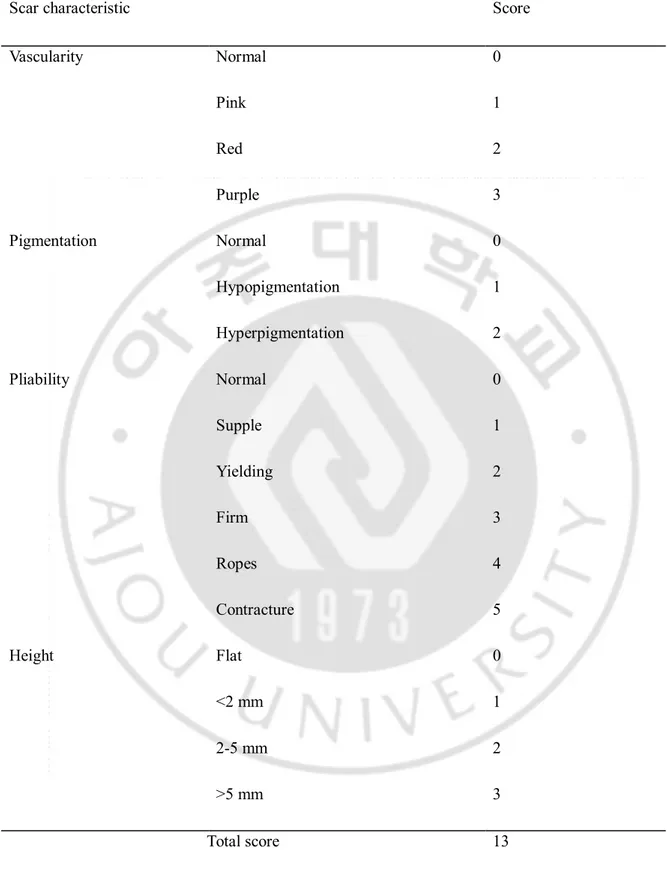
TABLE 1.∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙5
Vancouver Scar Scale (VSS)
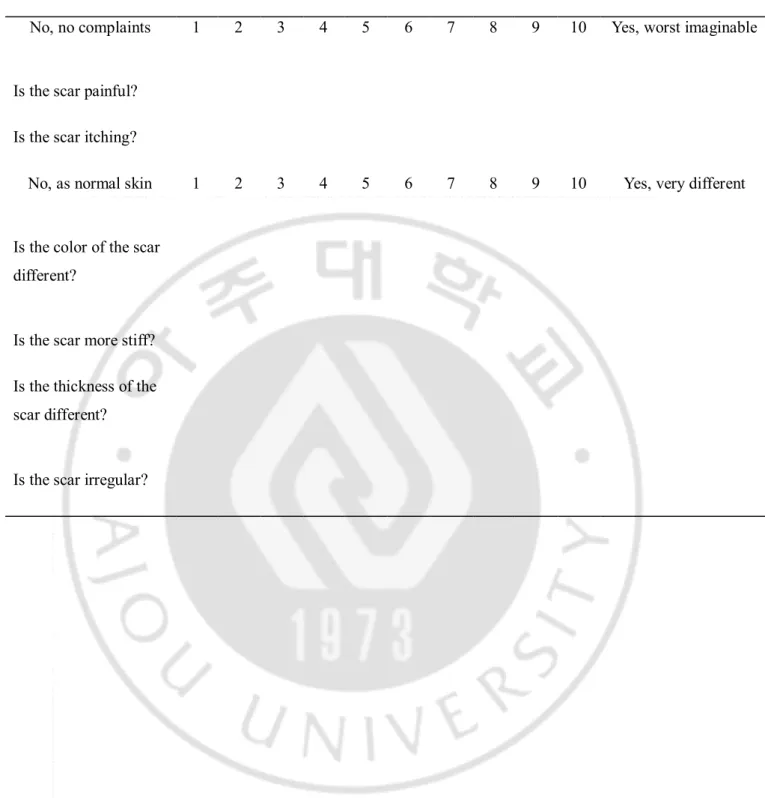
TABLE 2.∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙6
Patient Scar Assessment Scale of Patient and Observer Scar Assessment Scale (POSAS)
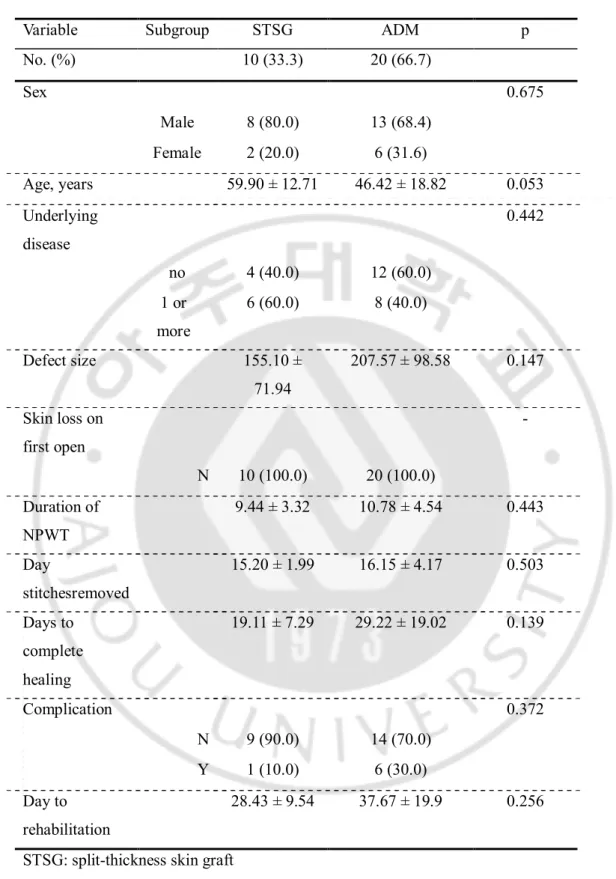
TABLE 3.∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙7
Demographic data and the early outcome of skin graft.
TABLE 4.∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙8
iii
TABLE 5. ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙9
- 1 -
I
NTRODUCTIONFull-thickness skin defect occurs by various causes including trauma, burn, and surgery. Such defects can cause aesthetic and functional problems. The latter include limited range of motion and joint stiffness because of adhesion and excessive scarring. Secondary or tertiary revision can be required. It is important to cover the full-thickness skin defect with minimal aesthetic and functional deficits in the early stage to minimize cost.Furthermore, in case of donor sites for the flap that destroy the normal structure, coverage with minimal deficits can be more significant.
Dermal substitutes share the function of normal dermis. They restore the skin anatomy and
physiologic function with their scaffolding properties and facilitate the invasion of normal fibroblasts and capillaries to synthesize new dermis.1As well, they increase the resistance to shear forces, and so
could be applicable in around joints.2
Donor sites for the flaps that are too large to achieve primary closure should be covered with a split thickness skin graft with or without acellular dermal matrix (ADM). Skin grafts with dermal substitutes results in better scar quality, such as elasticity and pliability.3,4,5However, these studies were limited in
that ADM was applied at different locations and for different wounds.
In this study, we investigated the effectiveness of acellular dermal matrix on scar quality of the skin graft sites of full-thickness skin defects. To avoid bias, we especially focused on the donor sites for the anterolateral thigh flapfrom the view of scar quality. Each graft was assessed with Vancouver Scar Scale (VSS), patient scar assessment scale of the Patient and Observer Scar Assessment Scale (POSAS), and measurement of skin fold compared to the normal side to investigate the degree of contracture.
- 2 -
II.
M
ETHODSPatient selection
Approval for the study was from our institutional review board (approval number 13-307). Written informed consent was obtained from all patients. The selected patients had received anterolateral thigh free flap to cover a defect from 2011 to 2015, and needed skin graft for the donor site with or without ADM graft. The reason for free flap coverage was related to trauma or malignancy. The patients with more than two flap donors and with an insufficient follow-up period (<6 months)were excluded.
Early and late outcomes of each skin graft were investigated by retrospectively reviewing medical records and clinical photos. Early outcome aspects included whether the skin loss occurred the first time the dressing was changedat the skin graft site, duration of the negative-pressure wound
therapy(NPWT), elapsed time in days from graft to removal of stitches, elapsed time in days to achieve complete healing (defined as > 80% graft take or change to open dressing), complications(infections or large skin loss that led to re-operation), and the elapsed time in days from graft to the start of
rehabilitation. Late outcome was evaluated after a minimum of 6 months postoperative six months and included the characteristics of the scar (vascularity, pigmentation, pliability, and height) and patient symptoms (itching sensation and pain). Assessments involved the Vancouver Scar Scale (VSS) (Table 1) and the patient scar assessment scale of the Patient and Observer Scar Assessment Scale (POSAS) (Table 2).6,7Skin fold was measured to evaluate the elasticity of scar tissue. It was measured by
examiner’s thumb and index finger and pinching the donor site and normal area of the patient’s thigh (as a control). In each patient, the assessment was performed by two experienced researchers. Forty six patients received reconstruction with anterolateral thigh free flaps from November 2011 to December 2015 at our institution. Among them, donor sites of 17 patients were covered with split thickness skin graft only, and those of 29 patients were covered with split thickness skin graft and ADM. Of the 17 patients with split thickness skin graft, 10 were available for assessment. Of the 29 patients with split thickness skin graft and ADM, 20 patients were available due to long-term follow-up loss.
Surgical procedure
We transferred free anterolateral thigh flap for the reconstruction of the defect caused by trauma or after wide excision of malignant skin tumor. The flap was elevated including the underlying fascia but without harvesting the vastus lateralis muscle. At the stage of donor site coverage, we divided the
- 3 -
patient in two groups. The skin graft only group was treated by autologous split-thickness skin graft alone. Autologous split-thickness skin graft (0.008~0.010 inch thick) was harvested from thigh using an electric dermatome (Zimmer Air Dermatome; Zimmer Inc., Warsaw, Ind., USA). The harvested skin was expanded 1.5 times with a mesh. The skin was then fixed to the recipient bed with skin stapler. The skin graft with acellular dermal matrix group was treated by cograft with autologous split-thickness skin graft with acellular dermal matrix. Autologous split-split-thickness skin graft (0.008~0.010 inch thick) was harvested from the thigh using an electric dermatome. Then, harvested skin was expanded 1.5 times with a mesh. Acellular dermal matrix (CG derm®; CG Bio, Inc., Seoul, Republic of
Korea) was rehydrated by submerging it in warm water (<37°C) for a minimum of 10 minutes. Rehydrated acellular dermal matrix and split-thickness skin graft were fixed with skin stapler. Negative-pressure wound therapy (CURAVAC; CG Bio) was applied to all of skin graft sites in both groups with negative pressure range from 80mmHg to 120mmHg in continuous mode. We changed the dressing at 4 days postoperatively for the first time and changed it every other day.
Statistical analyses
VSS scores, skin fold data, and patient scar assessment scale of the POSAS were compared using Wilcoxon Rank-Sum test. Continuous variables of demographic data were compared using Student’s T test. For categorical variables of demographic data, Fisher’s exact test was applied. Statistical
- 4 -
III.
R
ESULTS10 patients were included in skin graft only group and 20 patients were included in skin graft with ADM group. There was no statistical difference in sex, age, underlying disease, and size of the defect (i.e., donor site of the anterolateral thigh flap) between the two groups. There was no statistically difference in the early outcome between two groups (Table 3). The mean follow-up was 20.5 months (range, 7 to 45 months) in the skin graft only group and 19 months (range, 9 to 36 months) in the skin graft with ADM group.
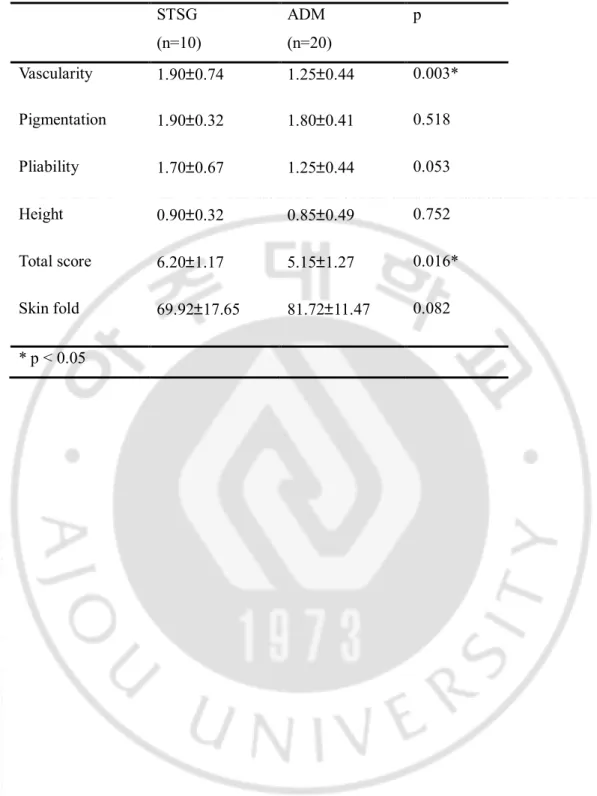
VSS scores are summarized in Table 4. The vascularity subscore was significantly lower in the skin graft with ADM group(1.25; 95% percent CI, 0.81 to 1.69) than in skin graft only group(1.90; 95% CI, 1.16 to 2.64) (p=0.003). The total score was significantly lower in the skin graft with ADM group(5.15; 95% CI, 3.88 to 6.42) than in skin graft only group(6.20; 95% CI, 4.97 to 7.43) (p=0.016). Skin fold calculated as the ratio of the skin fold thickness of donor site to that of normal area of the thighwas higher in the skin graft with ADM group than in skin graft only group, but showed no statistical significance (81.72% vs. 69.92%, p=0.082). The pigmentation subscore was lower in the skin graft with ADM group(1.80; 95% CI, 1.39 to 2.21) than in skin graft only group(1.90; 95% CI, 1.58 to 2.22), but showed no statistical significance (p=0.518). The pliability subscore was lower in the skin graft with ADM group(1.25; 95% CI, 0.81 to 1.69) than in skin graft only group(1.70; 95% CI, 1.02 to 2.38), but showed no statistical significance (p=0.053). The height subscore was lower in the skin graft with ADM group(0.85; 95% CI, 0.36 to 1.34) than in the skin graft only group(0.90; 95% CI, 0.58 to 1.22), but showed no statistical significance (p=0.752).
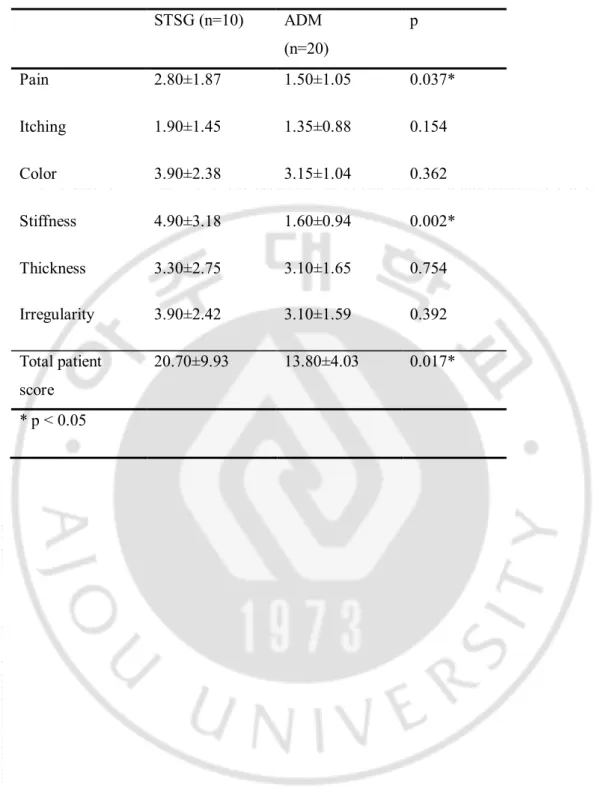
Patient score of Patient and Observer Scar Assessment Scale is described in Table 5. Total score was significantly lower in the skin graft with ADM group (13.80; 95% CI, 9.77 to 17.83) than in the skin graft only group(20.70; 95% CI, 10.77 to 30.63) (p=0.017). Pain subscore was significantly lower in skin graft with ADM group (1.50; 95% CI, 0.45 to 2.55) than in the skin graft only group (2.80; 95% CI, 0.93 to 4.67) (p=0.037). Stiffness subscore was significantly lower in the skin graft with ADM group (1.60; 95% CI, 0.66 to 2.54) than in the skin graft only group(4.90; 95% CI, 1.72 to 8.08) (p=0.002).Itching, color, thickness, and irregularity subscores were also lower in the skin graft with ADM group, but showed no statistical significance (Figure 1).
- 5 -
Table 1Vancouver Scar Scale (VSS)
Scar characteristic Score
Vascularity Normal 0 Pink 1 Red 2 Purple 3 Pigmentation Normal 0 Hypopigmentation 1 Hyperpigmentation 2 Pliability Normal 0 Supple 1 Yielding 2 Firm 3 Ropes 4 Contracture 5 Height Flat 0 <2 mm 1 2-5 mm 2 >5 mm 3 Total score 13
- 6 -
Table 2 Patient Scar Assessment Scale of Patient and Observer Scar Assessment Scale (POSAS)
No, no complaints 1 2 3 4 5 6 7 8 9 10 Yes, worst imaginable
Is the scar painful? Is the scar itching?
No, as normal skin 1 2 3 4 5 6 7 8 9 10 Yes, very different
Is the color of the scar different?
Is the scar more stiff? Is the thickness of the scar different?
- 7 -
Table 3Demographic data and the early outcome of skin graft.
Variable Subgroup STSG ADM p
No. (%) 10 (33.3) 20 (66.7) Sex 0.675 Male 8 (80.0) 13 (68.4) Female 2 (20.0) 6 (31.6) Age, years 59.90 ± 12.71 46.42 ± 18.82 0.053 Underlying disease 0.442 no 4 (40.0) 12 (60.0) 1 or more 6 (60.0) 8 (40.0) Defect size 155.10 ± 71.94 207.57 ± 98.58 0.147 Skin loss on first open - N 10 (100.0) 20 (100.0) Duration of NPWT 9.44 ± 3.32 10.78 ± 4.54 0.443 Day stitchesremoved 15.20 ± 1.99 16.15 ± 4.17 0.503 Days to complete healing 19.11 ± 7.29 29.22 ± 19.02 0.139 Complication 0.372 N 9 (90.0) 14 (70.0) Y 1 (10.0) 6 (30.0) Day to rehabilitation 28.43 ± 9.54 37.67 ± 19.9 0.256
STSG: split-thickness skin graft ADM: acellular dermal matrix
- 8 -
Table 4Results of Vancouver Scar Scale Scores
STSG (n=10) ADM (n=20) p Vascularity 1.90±0.74 1.25±0.44 0.003* Pigmentation 1.90±0.32 1.80±0.41 0.518 Pliability 1.70±0.67 1.25±0.44 0.053 Height 0.90±0.32 0.85±0.49 0.752 Total score 6.20±1.17 5.15±1.27 0.016* Skin fold 69.92±17.65 81.72±11.47 0.082 * p < 0.05
- 9 -
Table 5 Results of Patient score of Patient and Observer Scar Assessment Scale
STSG (n=10) ADM (n=20) p Pain 2.80±1.87 1.50±1.05 0.037* Itching 1.90±1.45 1.35±0.88 0.154 Color 3.90±2.38 3.15±1.04 0.362 Stiffness 4.90±3.18 1.60±0.94 0.002* Thickness 3.30±2.75 3.10±1.65 0.754 Irregularity 3.90±2.42 3.10±1.59 0.392 Total patient score 20.70±9.93 13.80±4.03 0.017* * p < 0.05
- 10 -
Figure 1. Two donor sites of the anterolateral thigh flap. Left: skin graft only, Right: skin graft with
acellular dermal matrix. Right picture shows better scar quality in vascularity, pigmentation, pliability, and subjective symptoms (pain, stiffness).
- 11 -
IV.
D
ISCUSSIONScar tissue is clinically distinguished from normal skin by color, texture, thickness, contraction, and firmness. This leads to cosmetic and functional sequelae and, especially near the joint area, contraction causes the limitation in the range of motion of joints. Scar evaluation requires control of various conditions, such as age, sex, and other demographics, and the status of the wound. In this study, we controlled the anatomical location, depth of the defect, degree of contamination, and interval to skin graft by evaluating the skin graft sites of the donor for the anterolateral thigh fasciocutaneous free flap. Also, operations were conducted by same operator who used the same procedure.
The anterolateral thigh flap was first described by Song et al. in 1984.8It has become widely used in
reconstruction because it has a long pedicle with good caliber and a large and pliable skin territory with the ability to design more than on skin paddle and to modify flap thickness.9 Donor site complications
of the anterolateral thigh flap include limited range of motion at the hip and knee joint, compromised muscle strength, impaired wound healing, numbness, and an aesthetic problem associated with hypertrophic scarring.9,10 However, donor site morbidity is much less than that of other flap and it is
major advantage of the anterolateral thigh flap. Scarring of the donor site is less noticeable than in other parts of body, but scar contracture can impair movement, produce symptoms like pain and itching, and create patient dissatisfaction because of scarring, especially when the donor site is covered with a skin graft.
Dermal substitutes have been used to minimize scar contracture and improve the scar quality.11 The
amount of dermis negatively correlates ion with the quality of the scarring and degree of
contracture.12,13 Various kinds of dermal substitutes have been developed. These include xenogenic
ADMs (Integra®,LifeSciences Corp., Plainsboro, NJ, USA; Matriderm®, Eurosurgical Limited, Guildford, UK) and allogenic ADMs (Alloderm®, LifeCell Corp., Branchburg, NJ, USA, CGderm®,
Daewoong Bio Incorporated, Seoul, South Korea). An ADM is a dermal allograft that is free of
immunogenic components; it can augment or replace the dermis at the wound site and better resembles normal skin. It contains collagen and elastin, which control tensile strength and elasticity,
proteoglycans that induce angiogenesis, laminin that maintains binding with the connective tissues, and basement membrane that consists of collagen type IV. ADMs or artificial dermal substitutes can be used with split skin graft to compensate for a limited range of motion and stiffness, especially near the joint area. An assessment of the long-term effectiveness of the Matriderm®bovine based collagen I, III,
and V and elastin-hydrolysate based dermal substitute in acute and reconstructive burn surgery included objective assessments (scar elasticity, vascularization, pigmentation, and surface roughness) and a subjective scar assessment using POSAS.14 The authors reported that the scar parameters
- 12 -
improved in both acute and reconstructive substituted wounds and increased elasticity in substituted scars in a largely expanded autograft. Presently, among the scar parameters, vascularity and the VSS total score, and POSAS pain and stiffness subscore, and total score were significantly higher in the ADM group.
Single stage ADM and autograft is difficult because it could require a longer period of stabilization for revascularization because of the increased diffusion distance for nutrients and oxygen to the autograft.15,16To compensate for this, we applied NPWT on the graft site. NPWT minimizes shearing
between the graft and wound bed and prevents formation of fluid and seroma to promote proper contact between the graft and the recipient bed.17,18 NPWT also increases wound blood flow.19 Thus, application of negative pressure therapy facilitates imbibition, inosculation, and neovascularization, which leads to increased graft take and survival.20,21 Our data of early outcomes of skin grafts revealed
no statistically significant differences in graft take and healing process. The data indicate minimal disadvantage of ADM and autograft in one-stage with NPWT in the healing process, with minimal scar formation and more desirable aesthetic results expected.
To evaluate the scar quality, we used the VSS and POSAS scar scales. VSS was 1990; it calculates subscores in four categories (vascularity, pigmentation, pliability, and height of the scar) and
aggregates the scores.6POSAS was developed more recently, in 2004, as an attempt to emphasize the importance of the subjective symptoms of patients that include pain and urtication, which had not been considered in previous scar assessment scales. Both are widely used scar assessment scales.7 There has
been a tendency in previous studies to assessed widespread operative scars with VSS,22 so we used
VSS and the patient component of POSAS in our study.
Excessive scarring could limit the range of motion, even in the absence of muscle or ligament injury. The split thickness skin graft could adhere to underlying fascia or muscle layer, which could limit hip and knee range of motion.10 Use of an ADM with split thickness skin graft could mitigate scar
contracture and improve the range of motion. In support of this scenario, the skin fold ratio (skin graft site to normal control) was higher in the ADM group, although it was not statistically difference from the skin graft only group.
The ADM was used for 20 patients who consented to its use. All 10 patients those in the skin graft only group had rejected the use of ADM, typically because of the expensive cost. The small patient numbers are a limitation of this study.
Several prior studies have also compared the skin graft outcome and scar quality in the skin graft only and skin graft with ADM graft groups. But, our study has a notably strong point – we compared the skin graft outcome and scar quality on donor sites of anterolateral thigh free flap located at a
- 13 -
similar anatomical position with a similar defect depth.So, we controlled for other variables that could affect the short- and long-term outcomes of the skin graft.
Several studies have reported that split-thickness skin graft with ADM graft show better scar quality in burn wounds,23, 24, 25, 26, 27 but the intervals from initial event that generated defect to time of coverage
were diverse, and there may have been difficulty in controlling the status of the wound bed. Presently, we covered the donor site of the anterolateral thigh flap immediately with the skin graft, so the wound bed of each case was similar.
- 14 -
V.
C
ONCLUSIONIn conclusion, as a large anterolateral thigh flap is harvested to cover the large defect, the donor site would arise close to the knee joint. Furthermore, since it cannot be closed primarily, the defect should be covered with a skin graft. This would limit the range of motion and produce an aesthetically undesirable scar. Co-grafting with ADM can improve scar quality in subjective and objective aspects. Delay in graft take can be compensated for by NPWT at the skin graft site.
- 15 -
R
EFERENCES1. van der Veen VC, van der Wal MB, van Leeuwen MC, Ulrich MM, Middelkoop E., Biological background of dermal substitutes., Burns. 2010 May;36(3):305-21.
2. Shahrokhi S, Arno A, Jeschke MG., The use of dermal substitutes in burn surgery: acute phase.,Wound Repair Regen. 2014 Jan-Feb;22(1):14-22.
3. Haslik W, Kamolz LP, Manna F, Hladik M, Rath T, Frey M. Management of full-thickness skin defects in the hand and wrist region: first long-term experiences with the dermal matrix Matriderm. J PlastRevconstrAesthetSurg 2010;63:360-4.
4. Munster AM, Smith-Meek M, Shalom A., Acellular allograft dermal matrix: immediate or delayed epidermal coverage?, Burns. 2001 Mar;27(2):150-3.
5. van Zuijlen PP, Vloemans JF, van Trier AJ, Suijker MH, van Unen E, Groenevelt F, Kreis RW, Middelkoop E., Dermal substitution in acute burns and reconstructive surgery: a subjective and objective long-term follow-up., PlastReconstr Surg. 2001 Dec;108(7):1938-46.
6. Sullivan T, Smith J, Kermode J, et al. Rating the burn scar. J Burn Care Rehabil 1990;11:256-60. 7. Draaijers LJ, Tempelman FR, Botman YA, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. PlastReconstrSurg 2004;113:1960-5.
8. Song YG, Chen GZ, Song YL. The free thigh flap: A new free flap concept based on the septocutaneous artery. Br J PlastSurg 1984;37:149-59.
9. Collins J, Ayeni O, Thoma A., A systematic review of anterolateral thigh flap donor site morbidity., Can J Plast Surg. 2012 Spring;20(1):17-23.
10. Kimata Y, Uchiyama K, Ebihara S, Sakuraba M, Iida H, Nakatsuka T, Harii K., Anterolateral thigh flap donor-site complications and morbidity., PlastReconstr Surg. 2000 Sep;106(3):584-9.
11. Haslik W1, Kamolz LP, Manna F, Hladik M, Rath T, Frey M., Management of full-thickness skin defects in the hand and wrist region: first long-term experiences with the dermal matrix Matriderm. J PlastReconstrAesthet Surg. 2010 Feb;63(2):360-4
12. Corps BV. The effect of graft thickness, donor site, and graft bed on graft thickness in the hooded rat. Br J PlastSurg 1969;22:125-133.
- 16 -
14. Bloemen MC1, van Leeuwen MC, van Vucht NE, van Zuijlen PP, Middelkoop E., Dermal
substitution in acute burns and reconstructive surgery: A 12-Year Follow-Up, PlastReconstr Surg. 2010 May;125(5):1450-9.
15. Wainwright, D., Madden, M., Luterman, A., et al. Clinical evaluation of an acellular allograft dermal matrix in full-thickness burns. J. Burn Care Rehabil. 17: 124,1996.
16.van Zuijlen PP, van Trier AJ, Vloemans JF, Groenevelt F, Kreis RW, Middelkoop E., Graft survival and effectiveness of dermal substitution in burns and reconstructive surgery in a one-stage grafting model., PlastReconstr Surg. 2000 Sep;106(3):615-23.
17. Moisidis E1, Heath T, Boorer C, Ho K, Deva AK., A prospective, blinded, randomized, controlled clinical trial of topical negative pressure use in skin grafting., PlastReconstr Surg. 2004 Sep
15;114(4):917-22.
18. Andrews BT, Smith RB, Chang KE, Scharpf J, Goldstein DP, Funk GF., Management of the radial forearm free flap donor site with the vacuum-assisted closure (VAC) system., Laryngoscope. 2006 Oct;116(10):1918-22.
19. Borgquist O, Ingemansson R, Malmsjö M., Wound edge microvascular blood flow during negative-pressure wound therapy: examining the effects of negative-pressures from -10 to -175 mmHg., PlastReconstr Surg. 2010 Feb;125(2):502-9.
20. Argenta LC, Morykwas MJ, Marks MW, DeFranzo AJ, Molnar JA, David LR., Vacuum-assisted closure: state of clinic art., PlastReconstr Surg. 2006 Jun;117(7 Suppl):127S-142S.
21. Moisidis E, Heath T, Boorer C, Ho K, Deva AK., A prospective, blinded, randomized, controlled clinical trial of topical negative pressure use in skin grafting., PlastReconstr Surg. 2004 Sep
15;114(4):917-22.
22. Seong Hwan Bae, Yong Chan Bae, Analysis of frequency of use of different scar assessment scales based on the scar condition and treatment method., Arch Plast Surg. 2014 Mar;41(2):111-5. doi: 10.5999
23. Munster AM, Smith-Meek M, Shalom A., Acellular allograft dermal matrix: immediate or delayed epidermal coverage?, Burns. 2001 Mar;27(2):150-3.
24. Haslik W, Kamolz LP, Nathschläger G, Andel H, Meissl G, Frey M., First experiences with the collagen-elastin matrix Matriderm as a dermal substitute in severe burn injuries of the hand., Burns. 2007 May;33(3):364-8. Epub 2007 Jan 22.
- 17 -
25. Branski LK, Herndon DN, Pereira C, Mlcak RP, Celis MM, Lee JO, Sanford AP, Norbury WB, Zhang XJ, Jeschke MG., Longitudinal assessment of Integra in primary burn management: a randomized pediatric clinical trial., Crit Care Med. 2007 Nov;35(11):2615-23.
26. Haslik W, Kamolz LP, Manna F, Hladik M, Rath T, Frey M., Management of full-thickness skin defects in the hand and wrist region: first long-term experiences with the dermal matrix Matriderm., J PlastReconstrAesthet Surg. 2010 Feb;63(2)
27. Ryssel H1, Gazyakan E, Germann G, Ohlbauer M., The use of MatriDerm in early excision and simultaneous autologous skin grafting in burns--a pilot study., Burns. 2008 Feb;34(1):93-7.
- 18 -
- 국문요약-
Effectiveness of acellular dermal matrix on autologous split-thickness skin
graft in treatment of deep tissue defect : Does cograft affect outcomes?
아주대학교 대학원의학과 이유정 (지도교수: 이일재) 전외측 대퇴 유리피판의공여부에부분층 피부이식술 단독 시행과 무세포 동종 진피를 이용한 부분층 피부이식술을 시행하였을 경우 장기간 추적 관찰 시 확인할 수 있는 반흔 정도를 객 관적, 주관적 반흔 평가 도구를 통해 비교 연구 하였다. 2011년부터 2015년까지 전외측대퇴유리피판술을 받은 환자 중 공여부에 피부이식술을 받 은 환자를 대상으로 연구를 진행하였다. 무세포 동종 진피를 이용해 피부이식술을 받은 환자 수는 20명이었으며, 피부이식술만 받은 환자수는 10명이었다.
이번 논문의 연구를 통해서 Vancouver scar scale 중 vascularity 및 total score 에서, 그리고 Patient and Observer Scar Assessment Scale 의 Patient score 에서는 pain, stiffness. total score 항목에서 통계학적으로 유의미하게 무세포 동종 진피를 이용한 환자군에서 더 우수한 반흔 정도를 보였다. 피부이식술을 요하는 심부 조직 결손 시 전층 피부이식술을 시행하지 못하는 큰 사이즈의 결 손부에무세포 동종 진피를 이용한 부분층 피부이식술을 시행함으로써 교원질, 탄력 섬유 및 기질을 보완하여 줄 수 있고, 더 나은 반흔 형성을 기대할 수가 있다. 특히 관절 부위에 해당되지 않지만 관절 부위 근처로 심한 반흔 및 이로 인한 구축 발생 시 운 동 제한 및 미용적인 문제를 야기할 수 있는 심부 조직 결손에 있어서 부분층 피부이식술 시 행 시 무세포 동종 진피의 사용을 고려해 볼 수 있다. 결론적으로, 무세포 동종 진피를 이용한 부분층 피부이식술이 객관적, 주관적인 면에서 더 나은 반흔 형성을 기대할 수가 있다. 그리고 무세포 동종 진피를 이용하였을 때 피부 생착 지연은 음압 치료를 이용한 드레싱으로 보상해줄 수 가 있다.