저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다.
The Incidence of Postoperative Nausea and
Vomiting after Thyroidectomy using Three
Anesthetic Techniques
by
Young Ju Won
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
The Incidence of Postoperative Nausea and
Vomiting after Thyroidectomy using Three
Anesthetic Techniques
by
Young Ju Won
A Dissertation Submitted to The Graduate School of
Ajou University in Partial Fulfillment of the Requirements
for the Degree of
Master of Medicine
Supervised by
Sook Young Lee, M.D., Ph.D.
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
This certifies that the dissertation
of Young Ju Won is approved.
SUPERVISORY COMMITTEE
Jin Soo Kim
Sook Young Lee
Sang Gee Min
Yun Geong Chae
Yong Woo Hong
The Graduate School, Ajou University
December, 20th, 2011
- ABSTRACT -
The Incidence of Postoperative Nausea and Vomiting after
Thyroidectomy using Three Anaesthetic Techniques
Introduction: The choice of anaesthetics can affect the incidence of postoperative nausea and vomiting (PONV). This study compared the incidence of PONV in female patients who underwent thyroidectomy with anaesthesia induced by sevoflurane, propofol– remifenanil or sevoflurane–propofol–remifentanil.
Methods: 177 female patients who underwent thyroidectomy were randomly allocated to three groups. Each patient was induced and maintained using one of three regimens: (i) sevoflurane (thiopental sodium 4 – 5 mg/kg and sevoflurane 2.0 – 2.5 vol% in 50% air); (ii) total intravenous anaesthesia (TIVA; propofol–remifentanil [target blood concentrations 2.5 – 3.5 μg/ml and 3.5 – 4.5 ng/ml, respectively]); or (iii) combined inhalation and intravenous anaesthesia (sevoflurane 1.0 vol% in 50% air plus propofol–remifentanil [target blood concentrations 1.5 – 2.5 μg/ml and 2.5 – 3.5 ng/ml, respectively]) The incidence and severity of PONV and the need for rescue antiemetics were assessed at 0 – 24 h postoperatively. Results: The overall incidence of PONV was significantly lower in the TIVA and combined groups compared with the sevoflurane group (33.9%, 39.0% and 64.4%, respectively). Conclusion: The maintenance of anesthesia with propofol–remifentanil or sevoflurane– propofol–remifentanil decreased the incidence of PONV compared with sevoflurane alone.
ii
Keyword:Thyroidectomy, Postoperative nausea and vomiting, Sevoflurane, Propofol,
TABLE OF CONTENTS
ABSTRACT ··· ⅰ TABLE OF CONTENTS ··· ⅲ LIST OF TABLE ··· ⅳ . Ⅰ INTRODUCTION··· 1 .Ⅱ PATIENTS AND METHODS ··· 3 . Ⅲ RESULTS ··· 6 . Ⅳ DISCUSSION ··· 13 . Ⅴ CONCLUSION ··· 17 REFERENCES ··· 18 국문요약 ··· 23
iv
LIST OF TABLE
Table 1. : Demographic characteristics and anaesthesia data of the study paients ··· 7
Table 2. : :Incidence of postoperative nausea and vomiting ··· 8
Table 3. : The severity score of nausea ··· 9
Table 4. : The severity score of vomiting ··· 10
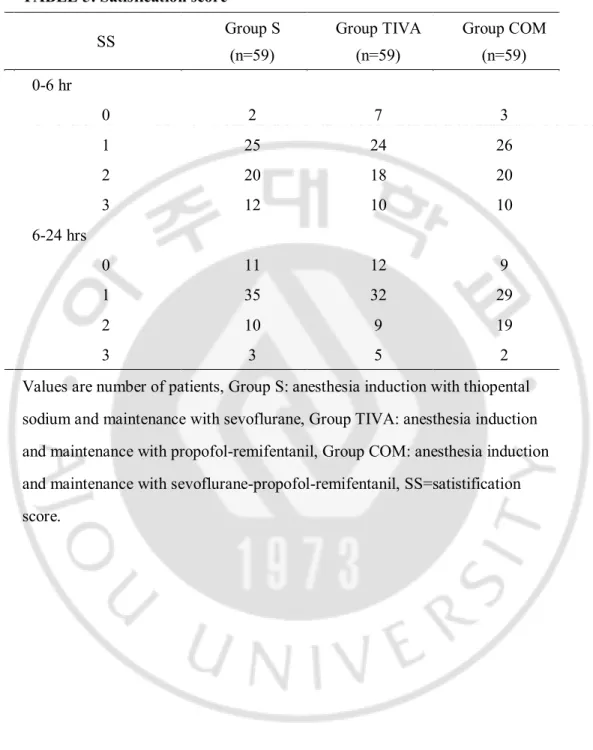
Table 5. : Satistification score ··· 11
I. INTRODUCTION
The incidence of postoperative nausea and vomiting (PONV) is estimated to be around 20-30% and is influenced by the patient, anesthetic and surgical factors (Palazzo and Strunin, 1984; Lerman, 1992; Rabey and Smith, 1992; Watcha and White, 1992; Apfel et al., 1999; Sinclair et al., 1999; Apfel et al., 2002). Certain procedures like thyroidectomy have been shown to have high rate of PONV with a reported incidence as high to 65-75 % (Ewalenko et al., 1996; Sonner et al., 1997; Gauger et al., 2008; Vari et al., 2010).As the practice of thyroid surgery shifts toward short hospital stay, the importance of PONV management increases due to its potential to delay discharge (Mowschenson PM, 1995). Additionally, vomiting may increase the risk of postoperative bleeding which may potentially cause airway obstruction (Kovac, 2000).
Compared to inhalational anesthesia, total intravenous anesthesia (TIVA) with propofol has been shown to decrease PONV (Borgeat et al., 1992; Brooker et al., 1998; Soppitt et al., 2000; Visser et al., 2001; Gauger et al., 2008; Vari et al., 2010), especially in women. However, anesthetic techniques without halogenated drugs showed relatively high incidence of awareness with recall during general anesthesia (Miller et al., 1996; Errando et al., 2008). Furthermore, commonly used TIVA combinations like propofol-remifentanil or propofol-alfentanil, show less hemodynamic stability compared with inhaled drugs (Vuyk et al., 1996).
For these reasons, we prefer to use combined anesthesia with inhalational (sevoflurane) and intravenous (propofol-remifentanil) drugs. However, there is no data on
2
-the incidence of PONV for combined anes-thesia.
The purpose of this study was to compare the incidence of PONV with sevoflurane, propofol-remifentanil or sevoflurane-propofol-remifentanil in the women patients who underwent thyroidectomy
.
Ⅱ
PATIENTS AND METHODS
This study was approved by the Institutional Review Board. After the obtaining the informed consents, 177 euthyroid state women patients with American Society of Anesthesiologists (ASA) physical status I or II, aged 18-60 years and scheduled for thyroidectomy under general anesthesia, were prospectively enrolled. Patients with more than 50% over ideal body weight, gastrointestinal disease, and those who had taken antiemetic within 24 hr prior to surgery were excluded from the study.
A medical history (including previous motion sickness, PONV and smoking) were recorded along with demographic information and the patients were randomly allocated by the sealed envelope method to one of three groups (n=59 in each). In group S (inhalational anesthetic, sevoflurane), anesthesia was induced with thiopental sodium (4 - 5 mg/kg) and was maintained with sevoflurane 2-2.5 vol% in 50% air. In group TIVA (remifentanil-propofol), anesthesia was induced and maintained with remifentanil (target blood concentration 3.5 - 4.5 ng/ml) and propofol (target blood concentration 2.5 - 3.5 µg/ml) without the use of inhalational anesthetics. In group COM, (sevoflurane-remifentanil-propofol) anesthesia was induced and maintained with remifentanil (target blood concentration 2.5 - 3.5 ng/ml), propofol (target blood concentration 1.5 - 2.5 µg/ml), and sevoflurane 1 vol% in 50% air. All patients were given rocuronium (0.6 mg/kg) to facilitate tracheal intubation. The target blood concentration of propofol and remifentanil was titrates using a target-controlled infusion (TCI) workstation ( Orchestra; fresenius Kabi, Bad Homburg, Germany ) and the depth of anesthesia was monitored by Bispectral Index™
4
-Monitor (Aspect Medical Systems, Inc., MA, USA).
Ventilation was mechanically controlled with O2/air mixture (fractional inspired
oxygen[FIO2]=0.5) and adjusted to keep an end-tidal concentration of CO2 between 35 and
40 mmHg throughout the operation. Muscle relaxation was antagonized by a combination of glycopyrrolate 0.002 mg/kg i.v. and pyridostigmine 0.03 mg/kgi.v. at the end of surgery.
Postoperative analgesia was provided with ketorolac trimethaphane (Tarasyn®, Roche
Korea, Seoul, Korea) 30 mg i.v. as required.
Postoperative assessments were made at 1 h in post-anesthesia care unit (PACU) by interview and at 6 h and 24 h by telephone interview and medical record reviews by nursing staff or the trainees. Patients, the nursing staff and the trainees responsible for follow up in the postoperative period were blinded to the patient’s group.
Nausea was defined as a subjective, unpleasant sensation associated with awareness of the urge to vomit. Retching was defined as the labored, spastic, rhythmic contraction of the respiratory muscles without expulsion of the gastric contents and vomiting was defined as the forceful expulsion of gastric contents from the mouth.
Each episode was recorded as either present or absent. If the patients had nausea, the severity was recorded using the following scale; 1=mild nausea, 2=moderate nausea and 3=severe nausea. If the patients had retching or vomiting, the severity of the episodes was recorded using the following scale; 1=one episode, 2=two episodes and 3=more than 3 episodes. The rescue antiemetic, metoclopramide 10 mg i.v. was administered when the patient request. At the end of the each periods, general satisfication was evaluated using a numerical scale ranging from 0 (complete satisfication) to 3 (complete dissatisfication). Any
other adverse effects were also recorded.
The sample size was predetermined by using a power analysis based on the following assumptions; the incidence of PONV (nausea, retching or vomiting) in sevoflurane group would be 60% (based on the previous studies)(Ewalenko et al., 1996; Sonner et al., 1997; Vari et al., 2010), decrease of incidence from 60% to 30% could be considered clinically significant, and the value of ɑ would be 0.05 with a power (1-β) of 0.9. The analysis showed that 52 patients per each group would be sufficient to detect the effect of anesthetic methods on the development of PONV and we rounded up to 59 patients per group.
Statistical analysis was performed using the statistical package (SPSS 17.0 for Windows; SPSS, Chicago, IL, USA). The parametric data (age, weight, height, anesthesia time, operation time) among the groups were analyzed by one-way ANOVA with Bonferroni’s correction. Discrete variables (history of motion sickness, history of PONV, history of smoking, presence of PONV such as nausea, retching or vomiting, side effects) were analyzed with the χ2 test. Differences in the distribution of nausea/vomiting severity
score and satisfication score were assessed using the Linear–by-Linear association test. All values are expressed as means ± SD or number of patients (%). A P value of < 0.05 was considered statistically significant.
6
-.
Ⅲ
RESULTS
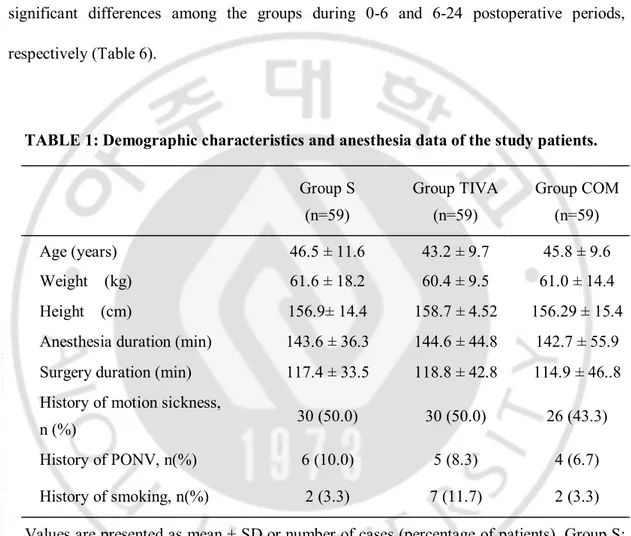
Total 177 patients (59 in each group) were included in this study. There were no differences in the patients’ demographic data among the three groups (Table 1). The incidence of postoperative nausea, retching or vomiting is listed in Table 2.
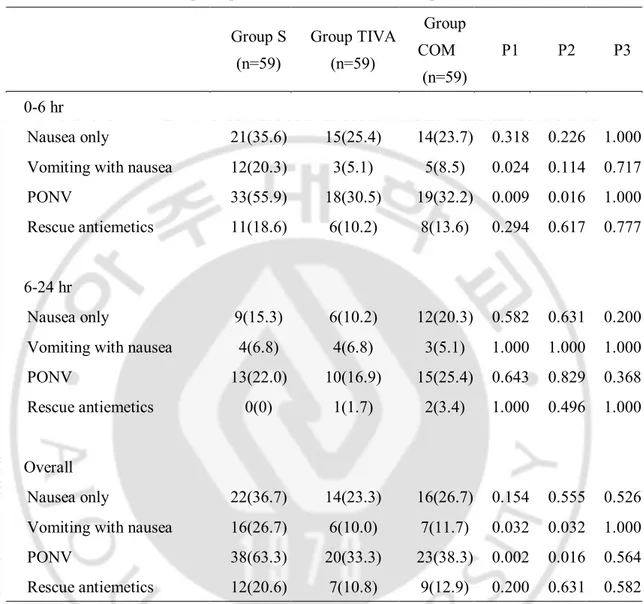
During the first 24 postoperative periods, the incidence of PONV in group TIVA (33.3%) and COM (38.3%) were significantly decreased compared to group S (63.3%) (P < 0.05; Table 2). During the same periods, the incidence of vomiting in group TIVA (10.0%) and COM (11.7%) were significantly decreased compared to group S (26.7%) (P < 0.05; Table 2). However, the incidence of nausea showed no significant differences among the groups (36.7%, 23.3% and 26.7% in group S, TIVA and COM, respectively).
During early postoperative periods (0-6 h), the incidence of PONV in group TIVA (30.5%) and COM (32.2%) were significantly decreased compared to group S (55.9%) (P<0.05; Table 2). During the same periods, the incidence of vomiting in group TIVA (5.1%) and COM (8.5%) were significantly descreased compared to group S (20.3%) (P<0.05; Table 2). However, the incidence of nausea showed no significant differences among the groups (35.6%, 25.4% and 23.7% in group S, TIVA and COM, respectively).
During late postoperative periods (6-24 h), there were no significant differences in the incidence of nausea, vomiting and PONV among the three groups (Table 2).
During the first 24 postoperative periods, there was no significant difference in the incidence of PONV between group TIVA and COM (Table 2).
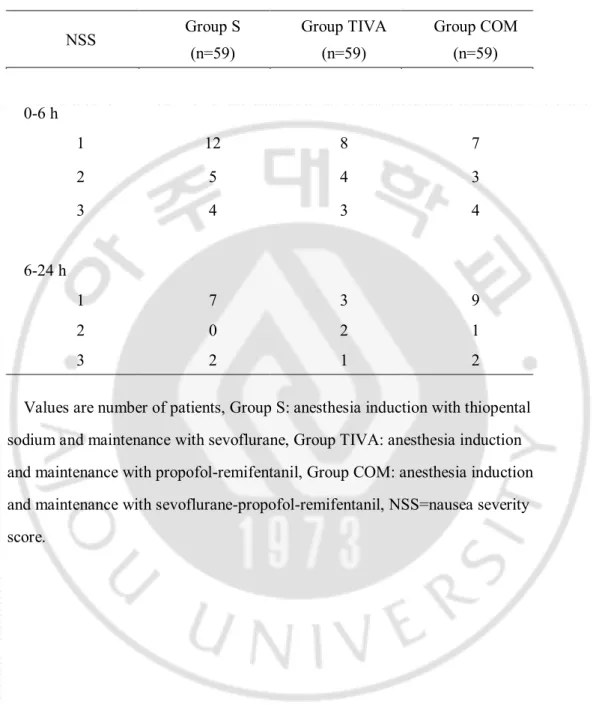
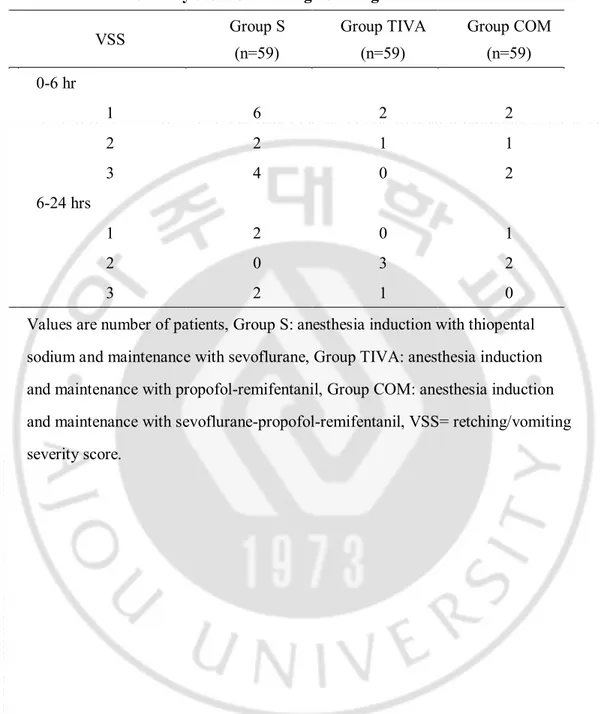
significant differences among the groups during 0-6 and 6-24 postoperative periods, respectively (Table 3, 4, 5).
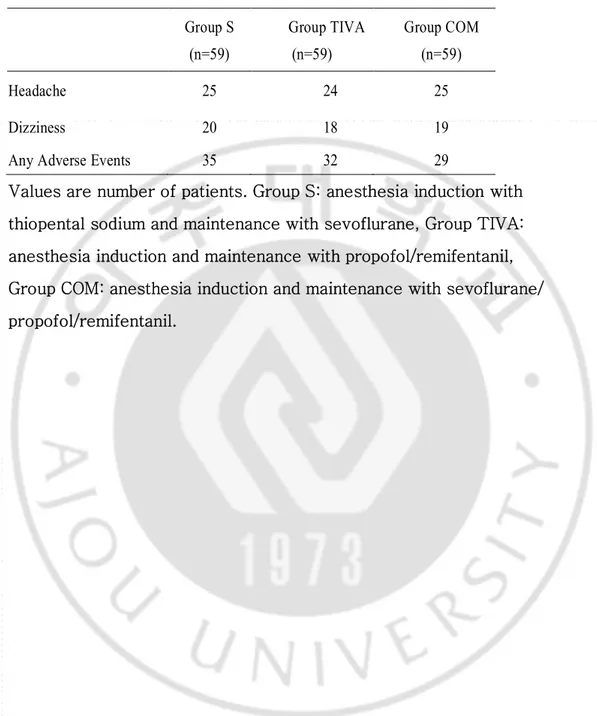
For the occurrence of side effects such as headache and dizziness, there were no significant differences among the groups during 0-6 and 6-24 postoperative periods, respectively (Table 6).
TABLE 1: Demographic characteristics and anesthesia data of the study patients. Group S (n=59) Group TIVA (n=59) Group COM (n=59) Age (years) 46.5 ± 11.6 43.2 ± 9.7 45.8 ± 9.6 Weight (kg) 61.6 ± 18.2 60.4 ± 9.5 61.0 ± 14.4 Height (cm) 156.9± 14.4 158.7 ± 4.52 156.29 ± 15.4
Anesthesia duration (min) 143.6 ± 36.3 144.6 ± 44.8 142.7 ± 55.9
Surgery duration (min) 117.4 ± 33.5 118.8 ± 42.8 114.9 ± 46..8
History of motion sickness,
n (%) 30 (50.0) 30 (50.0) 26 (43.3)
History of PONV, n(%) 6 (10.0) 5 (8.3) 4 (6.7)
History of smoking, n(%) 2 (3.3) 7 (11.7) 2 (3.3)
Values are presented as mean ± SD or number of cases (percentage of patients). Group S: anesthesia induction with thiopental sodium and maintenance with sevoflurane, Group TIVA: anesthesia induction and maintenance with propofol-remifentanil, Group COM:
anesthesia induction and maintenance with sevoflurane-propofol-remifentanil,
PONV=postoperative nausea and vomiting. n=number of cases. No significant difference among the groups.
8
-TABLE 2: Incidence of postoperative nausea and vomiting Group S (n=59) Group TIVA (n=59) Group COM (n=59) P1 P2 P3 0-6 hr Nausea only 21(35.6) 15(25.4) 14(23.7) 0.318 0.226 1.000
Vomiting with nausea 12(20.3) 3(5.1) 5(8.5) 0.024 0.114 0.717
PONV 33(55.9) 18(30.5) 19(32.2) 0.009 0.016 1.000
Rescue antiemetics 11(18.6) 6(10.2) 8(13.6) 0.294 0.617 0.777
6-24 hr
Nausea only 9(15.3) 6(10.2) 12(20.3) 0.582 0.631 0.200
Vomiting with nausea 4(6.8) 4(6.8) 3(5.1) 1.000 1.000 1.000
PONV 13(22.0) 10(16.9) 15(25.4) 0.643 0.829 0.368
Rescue antiemetics 0(0) 1(1.7) 2(3.4) 1.000 0.496 1.000
Overall
Nausea only 22(36.7) 14(23.3) 16(26.7) 0.154 0.555 0.526
Vomiting with nausea 16(26.7) 6(10.0) 7(11.7) 0.032 0.032 1.000
PONV 38(63.3) 20(33.3) 23(38.3) 0.002 0.016 0.564
Rescue antiemetics 12(20.6) 7(10.8) 9(12.9) 0.200 0.631 0.582
Values are number of patients (percentage of patients), Group S: anesthesia induction with thiopental sodium and maintenance with sevoflurane, Group TIVA: anesthesia induction and maintenance with propofol-remifentanil, Group COM: anesthesia induction and maintenance with sevoflurane-propofol-remifentanil, PONV= postoperative nausea and vomiting. P1: Group S versus Group TIVA, P2: Group S versus Group COM, P3: Group TIVA versus Group COM.
TABLE 3: The severity score of nausea
Values are number of patients, Group S: anesthesia induction with thiopental sodium and maintenance with sevoflurane, Group TIVA: anesthesia induction and maintenance with propofol-remifentanil, Group COM: anesthesia induction and maintenance with sevoflurane-propofol-remifentanil, NSS=nausea severity score. NSS Group S (n=59) Group TIVA (n=59) Group COM (n=59) 0-6 h 1 12 8 7 2 5 4 3 3 4 3 4 6-24 h 1 7 3 9 2 0 2 1 3 2 1 2
- 10 -
TABLE 4: The severity score of retching/vomiting
VSS Group S (n=59) Group TIVA (n=59) Group COM (n=59) 0-6 hr 1 6 2 2 2 2 1 1 3 4 0 2 6-24 hrs 1 2 0 1 2 0 3 2 3 2 1 0
Values are number of patients, Group S: anesthesia induction with thiopental sodium and maintenance with sevoflurane, Group TIVA: anesthesia induction and maintenance with propofol-remifentanil, Group COM: anesthesia induction and maintenance with sevoflurane-propofol-remifentanil, VSS= retching/vomiting severity score.
TABLE 5: Satisfication score SS Group S (n=59) Group TIVA (n=59) Group COM (n=59) 0-6 hr 0 2 7 3 1 25 24 26 2 20 18 20 3 12 10 10 6-24 hrs 0 11 12 9 1 35 32 29 2 10 9 19 3 3 5 2
Values are number of patients, Group S: anesthesia induction with thiopental sodium and maintenance with sevoflurane, Group TIVA: anesthesia induction and maintenance with propofol-remifentanil, Group COM: anesthesia induction and maintenance with sevoflurane-propofol-remifentanil, SS=satistification score.
- 12 -
Table 6: Adverse events
Group S (n=59) Group TIVA (n=59) Group COM (n=59) Headache 25 24 25 Dizziness 20 18 19
Any Adverse Events 35 32 29
Values are number of patients. Group S: anesthesia induction with thiopental sodium and maintenance with sevoflurane, Group TIVA: anesthesia induction and maintenance with propofol/remifentanil, Group COM: anesthesia induction and maintenance with sevoflurane/ propofol/remifentanil.
.
Ⅳ
DISCUSSION
This study showed that both TIVA (propofol-remifentanil) and combined anesthesia method (sevoflurane-propofol-remifentanil) decreased the incidence of PONV compared to inhalational anesthesia (sevoflurane) method without significant differences between TIVA and combined anesthesia method.
PONV is a distressing and frequently occurring adverse event of surgery under anesthesia with a reported incidence of 20-30% (Watcha and White, 1992). Certain surgery
like thyroidectomy is associated with high incidence of PONV as high to 65-75% (Ewalenko et al., 1996; Sonner et al., 1997; Gauger et al., 2008; Vari et al., 2010). Because patients typically have only mild-to-moderate pain after thyroid surgery, PONV may be perceived as the most unpleasant aspect of postoperative recovery. Additionally, these symptoms predispose to aspiration of gastric contents, airway obstruction by hematoma, increased intraocular pressure, psychological distress and delayed discharge (Mowschenson PM, 1995; Kovac, 2000).
The cause of PONV after thyroidectomy is not clearly known, but is probably related to several factors including gender, age range and intense vagal stimulation (surgical handling of neck structure)(Ewalenko et al., 1996; Sonner et al., 1997). Other factors such as obesity, history of motion sickness, previous PONV, smoking and anesthetic techniques are also considered to affect the incidence of PONV (Palazzo and Strunin, 1984; Lerman, 1992; Rabey and Smith, 1992; Watcha and White, 1992; Apfel et al., 1999; Sinclair et al., 1999; Apfel et al., 2002). In this study, however, the three groups were comparable with respect to
- 14 -
patient demographics and type of operation. Therefore, the difference in the incidence of PONV among the groups can be attributed to the anesthetic drugs administered. It is unlikely that changes in the level of circulating thyroid hormones may play a role in the production of nausea, because as part of the preoperative preparation, our patients were known to be in euthyroid state at the time of surgery.
The use of inhalational drugs is known to be a principal cause of PONV, especially during the early postoperative periods (Apfel et al., 2002; Apfel et al., 2005). Furthermore, nitrous oxide (N2O) may increase the incidence of PONV, in which a recent meta-analysis
showed an increase of PONV from 27% to 33% (Fernandez-Guisasola et al., 2010). In previous studies, the incidence of PONV was reported as high as 71% when isoflurane and nitrous oxide (N2O) were used in women who underwent thyroidectomy (Sonner et al., 1997;
Vari et al., 2010). In our study, the overall incidence of PONV was 63.3% when sevoflurane without nitrous oxide were used as maintenance of anesthesia.
Propofol used to maintain anesthesia has been associated with a lower incidence of PONV (Ewalenko et al., 1996; Sonner et al., 1997; Soppitt et al., 2000; Visser et al., 2001; Gauger et al., 2008; Vari et al., 2010).Several antiemetic mechanisms of propofol have been postulated including direct depression of chemoreceptor trigger zone and centers implicated on nausea and vomiting (Gan et al., 1997).Recently, weak 5-HT3 antagonistic effect was
suggested (Hammas et al., 1998). The proposed concentration range for sedation and general anesthesia by propofol is 1,500–2,000 ng/ml and 3,000–10,000 ng/ml, respectively (Smith et al., 1994; Reinsel et al., 1995; Vuyk et al., 1995).And, the proposed concentrations required to treat PONV are less than these values (Gepts et al., 1987; Gan et al., 1997). Gan et al.
(Gan et al., 1997) and Gepts et al. (Gepts et al., 1987) reported the antiemetic plasma propofol concentrations as 343-592 ng/ml and 424 ng/ml, respectively.
Opioids can produce PONV by various mechanisms, including direct effect in the chemoreceptor trigger zone in the area postrema of the brain stem, sensitization of the vestibular organ to movement-induced emesis, increase of gastrointestinal secretion, gastric hypomotility, and delayed gastric emptying (Watcha and White, 1992; Murphy et al., 1997). Remifentanil is a noncumulative ultra short-acting opioid with a half-life of 8–10 min (Burkle et al., 1996), which could contribute to faster weaning from opioid side-effects, such as PONV. However, the effect of remifentanil on the incidence of PONV is unclear. Recently, Oh et al. (Oh et al., 2010)demonstrated that combining remifentanil with sevoflurane did not increase the incidence of PONV compared to sevoflurane alone. In other studies, TIVA with propofol-remifentanil demonstrated decrease in PONV (Rusch et al., 1999; Hong et al., 2008; Liao et al., 2010).
In our study, TIVA with propofol/remifentanil decreased the incidence of PONV, which is consistent with previous studies performed in other type of surgeries (Rusch et al., 1999; Hong et al., 2008; Liao et al., 2010). Furthermore, combined anesthesia with sevoflurane-propofol-remifentanil also decreased the incidence of PONV compared to sevoflurane group and there was no difference in the incidence of PONV compared to TIVA (63.3%, 33.3% and 38.3% in sevoflurane, TIVA and combined anesthesia, respectively). There may be several reasons. First, we used the target blood concentration of propofol between 2.5-3.5 µg/ml in the TIVA group and 1.5-2.5 µg/ml in the combined anesthesia group and both are higher than proposed antiemetic concentration (Gepts et al., 1987; Gan et
- 16 -
al., 1997). Second, lower concentration of sevoflurane was used in the combined group compared to the sevoflurane group (2-2.5 vol% versus 1 vol%).
Gaugher et al. (Gauger et al., 2008) demonstrated that propofol decreased the early PONV rather than the late PONV. In our study, the incidence of PONV was mainly decreased during 0-6 h postoperative periods (30.5 %, 32.2 % and 55.9% in TIVA, combined and sevoflurane group) and consistent with previous results.
For the comparing the nausea/vomiting severity score and satisfication score, there were no significant differences among the groups.
For the incidence of adverse events, such as headache and dizziness, there were no significant differences among the groups.
The limitation of this study is no data were shown about the incidence of awareness with recall and hemodynamic stability among the groups. However, in sevoflurane and combined anesthesia group, no patients complained about the awareness with recall in the PACU and there were no significant hypotension or bradycardia in all three groups.
.
Ⅴ
CONCLUSION
In conclusion, both TIVA (propofol-remifentanil) and combined anesthesia (sevoflurane-propofol-remifentanil) can be used with same degree decrease of the incidence of PONV compared to sevoflurane in the women patients who underwent thyroidectomy.
- 18 -
REFERENCES
1. Apfel C, Stoecklein K, Lipfert P: PONV: a problem of inhalational anaesthesia? Best
practice & research. Clinical anaesthesiology 19: 485-500, 2005
2. Apfel CC, Kranke P, Katz MH, Goepfert C, Papenfuss T, Rauch S, Heineck R, Greim
CA, Roewer N: Volatile anaesthetics may be the main cause of early but not delayed postoperative vomiting: a randomized controlled trial of factorial design. Br J Anaesth 88: 659-668, 2002
3. Apfel CC, Lr E, Koivuranta M, Greim CA, Roewer N: A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology 91: 693-700, 1999
4. Borgeat A, Wilder Smith OH, Saiah M, Rifat K: Subhypnotic doses of propofol possess direct antiemetic properties. Anesth Analg 74: 539-541, 1992
5. Brooker CD, Sutherland J, Cousins MJ: Propofol maintenance to reduce postoperative
emesis in thyroidectomy patients: a group sequential comparison with isoflurane/nitrous oxide. Anaesth Intensive Care 26: 625-629, 1998
6. Burkle H, Dunbar S, Van Aken H: Remifentanil: a novel, short-acting, mu-opioid. Anesth Analg 83: 646-651, 1996
7. Errando CL, Sigl JC, Robles M, Calabuig E, Garca J, Arocas F, Higueras R, Del Rosario E, Lpez D, Peir CM, Soriano JL, Chaves S, Gil F, Garca-Aguado R: Awareness with recall during general anaesthesia: a prospective observational evaluation of 4001 patients. Br J Anaesth 101: 178-185, 2008
8. Ewalenko P, Janny S, Dejonckheere M, Andry G, Wyns C: Antiemetic effect of subhypnotic doses of propofol after thyroidectomy. Br J Anaesth 77: 463-467, 1996
9. Fernandez-Guisasola J, Gomez-Arnau JI, Cabrera Y, del Valle SG: Association
between nitrous oxide and the incidence of postoperative nausea and vomiting in adults: a systematic review and meta-analysis. Anaesthesia 65: 379-387, 2010
10. Gan TJ, Glass PS, Howell ST, Canada AT, Grant AP, Ginsberg B: Determination of plasma concentrations of propofol associated with 50% reduction in postoperative nausea. Anesthesiology 87: 779-784, 1997
11. Gauger PG, Shanks A, Morris M, Greenfield ML, Burney RE, O'Reilly M: Propofol decreases early postoperative nausea and vomiting in patients undergoing thyroid and parathyroid operations. World J Surg 32: 1525-1534, 2008
12. Gepts E, Camu F, Cockshott ID, Douglas EJ: Disposition of propofol administered as constant rate intravenous infusions in humans. Anesth Analg 66: 1256-1263, 1987
13. Hammas B, Hvarfner A, Thorn SE, Wattwil M: Effects of propofol on ipecacuanha-induced nausea and vomiting. Acta Anaesthesiol Scand 42: 447-451, 1998
14. Hong JY, Kang YS, Kil HK: Anaesthesia for day case excisional breast biopsy: propofol-remifentanil compared with sevoflurane-nitrous oxide. Eur J Anaesthesiol 25: 460-467, 2008
15. Kovac AL: Prevention and treatment of postoperative nausea and vomiting. Drugs 59: 213-243, 2000
16. Lerman J: Surgical and patient factors involved in postoperative nausea and vomiting. Br J Anaesth 69: 24S-32S, 1992
- 20 -
17. Liao R, Li JY, Liu GY: Comparison of sevoflurane volatile induction/maintenance anaesthesia and propofol-remifentanil total intravenous anaesthesia for rigid bronchoscopy under spontaneous breathing for tracheal/bronchial foreign body removal in children. Eur J Anaesthesiol 27: 930-934, 2010
18. Miller DR, Blew PG, Martineau RJ, Hull KA: Midazolam and awareness with recall during total intravenous anaesthesia. Can J Anesth 43: 946-953, 1996
19. Mowschenson PM HR: - Outpatient thyroid and parathyroid surgery: A prospective study of feasibility, safety, and costs. Surgery 118: 1051-1054, 1995.
20. Murphy DB, Sutton JA, Prescott LF, Murphy MB: Opioid-induced delay in gastric emptying: a peripheral mechanism in humans. Anesthesiology 87: 765-770, 1997
21. Oh AY, Kim JH, Hwang JW, Do SH, Jeon YT: Incidence of postoperative nausea and vomiting after paediatric strabismus surgery with sevoflurane or remifentanil-sevoflurane. Br J Anaesth 104: 756-760, 2010
22. Palazzo MG, Strunin L: Anaesthesia and emesis. I: Etiology. Can Anaesth Soc J
31: 178-187, 1984
23. Rabey PG, Smith G: Anaesthetic factors contributing to postoperative nausea and vomiting. Br J Anaesth 69: 40S-45S, 1992
24. Reinsel RA, Veselis RA, Wronski M, Marino P: The P300 event-related potential during propofol sedation: a possible marker for amnesia? Br J Anaesth 74: 674-680, 1995 25. Rusch D, Happe W, Wulf H: [Postoperative nausea and vomiting following stabismus
surgery in children. Inhalation anesthesia with sevoflurane-nitrous oxide in comparison with intravenous anesthesia with propofol-remifentanil]. Anaesthesist 48: 80-88, 1999
26. Sinclair DR, Chung F, Mezei G: Can postoperative nausea and vomiting be predicted? Anesthesiology 91: 109-118, 1999
27. Smith C, McEwan AI, Jhaveri R, Wilkinson M, Goodman D, Smith LR, Canada AT,
Glass PS: The interaction of fentanyl on the Cp50 of propofol for loss of consciousness and skin incision. Anesthesiology 81: 820-828; 1994
28. Sonner JM, Hynson JM, Clark O, Katz JA: Nausea and vomiting following thyroid and parathyroid surgery. J Clin Anesth 9: 398-402, 1997
29. Soppitt AJ, Glass PS, Howell S, Weatherwax K, Gan TJ: The use of propofol for its antiemetic effect: a survey of clinical practice in the United States. J Clin Anesth 12: 265-269, 2000
30. Vari A, Gazzanelli S, Cavallaro G, De Toma G, Tarquini S, Guerra C, Stramaccioni E, Pietropaoli P: Post-operative nausea and vomiting (PONV) after thyroid surgery: a prospective, randomized study comparing totally intravenous versus inhalational anesthetics. Am Surg 76: 325-328, 2010
31. Visser K, Hassink EA, Bonsel GJ, Moen J, Kalkman CJ: Randomized controlled trial of total intravenous anesthesia with propofol versus inhalation anesthesia with isoflurane-nitrous oxide: postoperative nausea with vomiting and economic analysis. Anesthesiology 95: 616-626, 2001
32. Vuyk J, Engbers FH, Burm AG, Vletter AA, Griever GE, Olofsen E, Bovill JG: Pharmacodynamic interaction between propofol and alfentanil when given for induction of anesthesia. Anesthesiology 84: 288-299, 1996
- 22 -
33. Vuyk J, Lim T, Engbers FH, Burm AG, Vletter AA, Bovill JG: The pharmacodynamic interaction of propofol and alfentanil during lower abdominal surgery in women. Anesthesiology 83: 8-22, 1995
34. Watcha MF, White PF: Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology 77: 162-184, 1992
- 국문요약 -
수술
중 투여된 전신마취 약제에 따른 갑상선 절제술 후 오심
및
구토 발생률의 변화
아주대학교 대학원 마취통증의학과 원영주 (지도교수: 이숙영) 연구 배경: 갑상선 절제술을 받은 환자에서 수술 후 오심 및 구토 (postoperativenausea and vomiting, PONV)발생률은 65-75%로 타 수술과 비교하여 높은 것으로 보고되고 있다. 본 연구는 PONV 발생률에 영향을 미치는 요인 중 하나인 전신마취 중 투여되는 약제 선택에 따른 PONV 발생률의 변화를 관찰하였다.
대상 및 방법: 177 명의 갑상선 절제술을 받는 여자 환자를 대상으로 하여
마취유도 전 무작위로 세 군으로 나누었다. 흡입마취군 (Group S)에서는 thiopental sodium 4-5 mg/kg 로 마취 유도 후 sevoflurane 2-2.5 vol%/산소/의료용 공기로 마취 유지하였고, 전정맥마취군 (Group TIVA, total intravenous anesthesia 로 마취한 군)에서는 remifentanil (목표 혈중 농도 3.5-4.5 ng/ml)과 propofol (목표 혈중 농도 2.5-3.5 μg/ml)을 사용하여 마취를 유도 및 유지하였고, 혼합마취군 (Group COM, combined anesthesia 로 마취한 군)에서는 remifentanil (목표 혈중 농도 2.5-3.5 ng/ml), propofol (목표 혈중 농도 1.5-2.5 μg/ml)의 정맥투여, sevoflurane 1 vol%/산소/의료용
- 24 -
공기로 마취를 유도 및 유지하였다. 수술 후 24 시간 동안 PONV 발생률, 오심 및 구토의 정도, 진토제의 투여 여부를 관찰 하였다.
결과: 술후 첫 24 시간 동안 PONV 발생률은 흡입마취 군(63.3%)과 비교하여
전정맥마취군(32.3%)과 혼합마취군(38.3%)에서 통계학적으로 유의하게 낮았다.
결론: propofol-remifentanil 뿐만 아니라 sevoflurane–propofol- remifentanil 을 이용한
마취유지는 sevoflurane 을 이용한 흡입마취와 비교하여 PONV 를 의미 있게 낮추었으며, 전정맥마취군과 혼합마취군 사이에는 유의한 차이를 보이지 않는다. 핵심어: 갑상선 절제술, Sevoflurane, Propofol, Remifentanil, 수술 후 오심 및 구토