저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다.
Risk of cervical lymph node metastasis in
papillary thyroid carcinoma: Correlations
with lymphangiogenesis and ultrasound
features
by
Yoon-Jung Choi
Major in Radiology
Department of Medical Sciences
The Graduate School, Ajou University
Risk of cervical lymph node metastasis in
papillary thyroid carcinoma: Correlations
with lymphangiogenesis and ultrasound
features
by
Yoon-Jung Choi
A Dissertation Submitted to The Graduate School of Ajou University
in Partial Fulfillment of the Requirements for the Degree of
Ph. D. in Radiology
Supervised by
Kyung-Joo Park, M.D., Ph.D.
Major in Radiology
Department of Medical Sciences
The Graduate School, Ajou University
This certifies that the dissertation
ofYoon-Jung Choi is approved.
SUPERVISORY COMMITTEE
Kyung Joo Park
Mison Chun
Doo Kyoung Kang
Yong SikJoeng
Sunmi Kim
The Graduate School, Ajou University
December, 31st, 2012
i
-
ABSTRACT
-Risk of cervical lymph node metastasis in papillary thyroid
carcinoma: Correlations with lymphangiogenesis and ultrasound
features
Stratification of risk factors for cervical lymph node metastasis (LNM) in thyroid papillary carcinoma is important for providing standards for post-operative adjuvant radio-iodine therapy and for predicting patient prognosis. We investigated pathological factors based on the lymphatic vessel system and ultrasound features associated with tumor with cervical LNM. Among patients who had undergone thyroidectomy confirmed to be papillary thyroid carcinoma, we selected 126 age-sex matched paired patients without cervical LNM (group 1) and with LNM (group 2) to evaluate risk factors. Pathological factors evaluated were size, multiplicity, and extra thyroid extension state, based on the pathological reports using stored data. The lymphatic vessel density (LVD) of each tumor was evaluated by staining forVEGFR-3 and D2-40 and correlated with cervical LNM state.Ultrasound features were evaluated to compare the differences between these two groups. Larger tumor size, multiplicity, extrathyroid extension were more common in group 2 (p<0.05). The median percentage of VEGFR-3 for group 1 was 20 (range 0-30) and D2-40 was 13 (range 7-23) while for group 2,VEGFR-3 was 80 (70-90) and D2-40 was 78 (54-114). LVD measured by intratumoral D2-40 staining was 20.6% and 79.4% for group 1 and group 2, respectively. Intra-tumorallymphatics measured by D2-40 stain had a strong correlation with cervical LNM (Odds 1.230, CI 1.01.-1.499p value 0.040). US features had no significant differences between the two groups although calcifications tended to be higher in group 2 (84% vs 76% p=0.264). Lymphatic vessel density and nodule echogenicity did not show correlations.
ii
Intratumorallymphangiogenesiswas most strongly associated with LNM and thus,could be a useful predictive marker for cervical LNM.
Keyword:Lymphangiogenesis, lympho-vascular density, Papillary thyroid cancer,
iii
TABLE OF CONTENTS
ABSTRACT i
TALBLE OF CONTENTS ⅲ LIST OF FIGURES AND TABLESⅳ ABBREVIATIONⅴⅠ. INTRODUCTION ··· 1
Ⅱ. MATERIALS AND METHODS ··· 3
1. Patient Selection ··· 3
2. Immunohistochemistry ··· 4
3.Imaging and Imaging Analysis ··· 10
4. Statistical Analysis ··· 11 Ⅲ. RESULTS ··· 12 1. Univariate analysis ··· 12 2. Multivariate analysis ··· 14 3. Imaging analysis ··· 16 Ⅳ. DISCUSSION ··· 20 Ⅴ. CONCLUSION ··· 25 REFERENCES ··· 26 국문요약 ··· 32
iv
LIST OF FIGURES AND TABLES
Fig. 1.D2-40 Immunostain for intratumoral area 6 Fig. 2.D2-40 Immunostain for peritumoral area 7 Fig. 3.VEGFR-3 Immunostain 9 Table 1. Distribution of clinical and pathological risk factors 13
Table 2.Conditional logistic analysis of risk factors for cervical LNM 15 Table 3. Comparisons of US features 17 Table 4.US features suggesting malignancy between PMC and PTC 19
v
LIST OF ABBREVIATION
PMC, papillary microcarcinoma PTC, papillary thyroid carcinoma ETE, extra thyroid extension LMN, lymph node metastasis LVD, lymphatic vascular density D2-40, Podoplamin
- 1 -
I. INTRODUCTION
Papillary thyroid cancer (PTC) is known to have a low postsurgical recurrence rate about 5-20% with overall high survival rate. (Byar et al., 1979; Tennvall et al., 1986; DeGroot et al., 1990; Hay et al., 1993; Sebastian et al., 2000). Risk stratification has been investigated as a way to minimize the extent of surgery and exposure to high dose iodine therapy (Baek et al.; Riemann et al.; Jeong et al., 2011; Ito et al., 2012b). Patient age, tumor subtype, extra thyroid extension (ETE), and cervical lymph node metastasis (LMN), are known risk factors
associated with increased recurrence of PTC(Baek et al.; Beasley et al., 2002a; Kuo et al., 2008; Ito et al., 2012a; Ito et al., 2012c). Patients with cervical LNM at the time of surgery should undergo lateral neck dissection and consider high dose iodine therapy,even though it can lower a patient’s quality of life. Furthermore, patients with cervical LNMhave an increased chance of recurrences even after the high dose iodine therapy (Beasley et al., 2002a; Ito et al., 2009). Thus, improved prediction of cervical LNM and understanding of the factors affecting LNM would have a strong clinical impact.
A high incidence of cervical LNM in PTC suggests a possibleassociation of tumor spread and lymphangiogenesis. The mechanisms that drive metastasis arelargely unknown
andlymphangiogenesis has not beenwidely studied (Yasuoka et al., 2005).Podoplanin (D2-40 ) is a monoclonal antibody with selective immunoreactivity for lymphatic endothelium only and not the vascularity, which enable to quantify lymphatic vessel density(Kahn and Marks, 2002; Kawaura et al., 2007). Vascular endothelial growth factor receptor-3 (VEGFR-3) is a potent stimulator of endothelial cell growth and can promote more
- 2 -
selectively on lymphangiogenesis(Kukk et al., 1996). We sought to evaluate the
relationships between cervical LNM status and lymphatic vascular density (LVD) using D2-40 intratumorally and peritumorally, and VEGFR-3expression focused on the pathological features, especially in lymphatic vessel systems since the degree of tumorlymphangiogenesis may theoretically be related tothe risk for LNM.
US features suggestive of malignancy in thyroid nodules have been well established, such as the presence of microcalcifications, hypoechogenicity, irregular margins, and solid composition (Frates and Benson, 2001; Kim et al., 2002; Nam-Goong et al., 2004; Cappelli et al., 2007) but US features of thyroid malignancy associated with increased frequency of LNM have not been previously reported. One study recently published by Kwak et al. focused on LNM of papillary micro-carcinoma and suggested that an upper pole location, contact with the adjacent capsule of >25%, presence of calcifications, and central LNM seen in pre-operative ultrasound were all high risk factors for lateral LNM in papillary micro-carcinomas (Kwak et al., 2009). This study included only papillary micro-carcinoma so we attempted to identify malignant US feature that were associated with cervical LNM
regardless of tumor size, since US is a highly sensitive and specific imaging modality used in thediagnosis of thyroid malignancy.
- 3 -
II. MATERIALS AND METHODS
1. Patient Selection
Institutional review board approval was obtained for this study and patient informed consent was waived. All participants agreed on using their pathological specimens to carry out the immunostainings and for using their stored pathological data. The study samples were collected consecutively fromJanuary 2007 to December 2010. The data consisted of 1012 patients who had undergone thyroid cancer surgery, (age range: 16–83 years; mean: 51 years). This series was comprised of PTC of the conventional form only. Ninety-one patients subsequently underwent total thyroidectomy with central and lateral neck dissection, 371 underwent a total thyroidectomy with central node dissection alone, 455 had a total thyroidectomy or lobectomy with ipsilateral central neck dissection, and 95 patients underwent only lobectomy, without nodal dissection. Based on the pathology of the dissection results, the patients were divided into four groups: no lymph node submitted to pathology group, no central LNM group, central LNM only group, and both central and lateral LNM group. We excluded no lymph node submitted group and central LNM only group because mainly central LNM are microscopic metastatsis with small clinical impact when removed by routine ipsilateral central neck dissections are carried out and we wanted to compare more disease progressed patients with central and lateral LNM. When cases were matched to controls by age and sex, a total of 126 patients were selected to make up two groups, group 1 with no LNM (n=63) and group 2 with both central and lateral LNM (n=63). When multiple nodules were present, we selected the larger main mass to evaluate the lymphatic vessel and US features.
- 4 - 2. Immunohistochemistry
Gross pathologic specimens of the patients were sent to pathologic department for immunohistochemical stain and analysis for the final pathological diagnosis were done according to World Health Organization classification.
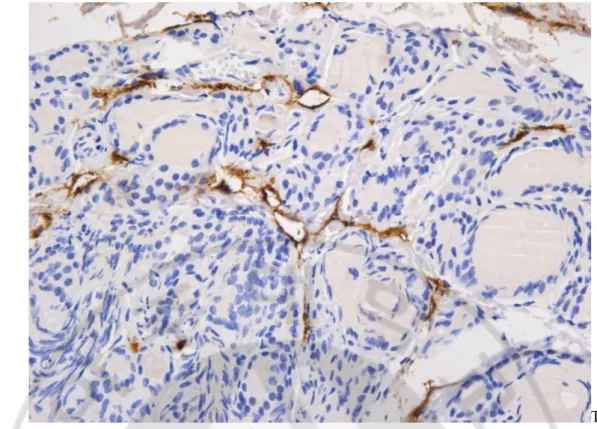
Blinded to the final report of LNM state, 126 thyroid tissue samples were analyzed for immunohistochemical expression of D2-40 and VEGFR-3 using a mouse monoclonal D2-40 clone (Cell Marque, Rocklin, CA, USA) specific antibody and mouse monoclonal antibody for VEGFR-3 (Novocastra, Benton Lane, Newcastle, UK). The level of D2-40 expression were quantified separately in intra- and peritumoral areas (Fig. 1,2).Determination of LVD assessed by immunostaining for D2-40 was performed as suggested by Weidner et al (Weidner et al., 1991). After scanning the immunostained section at low magnification (40X), the area of tissue with the greatest number of distinctly highlighted micro-vessels, or “hotspot”, was selected. LVD was then determinedby counting all immune-stained vessels at a total magnification of 200X from total areas for each case. LVD was defined as a single endothelial cell or a cluster of endothelial cells positive for D2-40, located near a visible lumen clearly separate from adjacent micro-vessels and other connective tissue components. The numbers of lymphatic spaces counted were divided by the area (total number of lymphatic spaces/cm2). Additionally, as lymphatic vessels can
generally appear as distorted and overlapped structures in a cancer setting, packed vessels were assumed to be one lymphatic unit. Determination of the staining reaction was strictly confined to the hotspots. Figure 1 demonstrates D2-40 Immunostain for intratumoral area(It was considered positive when the staining was visible in the cytoplasm of the lymphatic
- 5 -
- 6 -
T
Fig. 1.D2-40 Immunostain for intratumoral area. D2-40 immunostain showed positive for
lymphatic spaces in intratumoral area (immunohistochemical staining with DAB, X400). Lymphatic vessels can generally appear as distorted and overlapped structures in a cancer setting, packed vessels were assumed to be one lymphatic unit. Determination of the staining reaction was strictly confined to the hotspots. This figure demonstrates an immunohistochemical reaction for D2-40 intratumorally
- 7 -
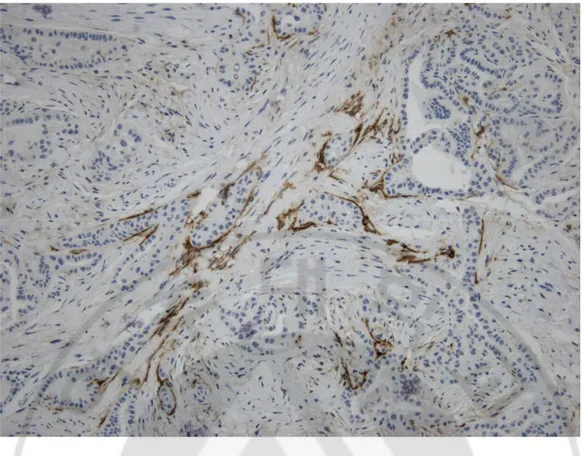
Fig. 2.Immunostain for peritumoral area.D2-40 immunostain showed positive for
lymphatic spaces in peritumoral area (immunohistochemical staining with DAB, X400). LVD was defined as a single endothelial cell or a cluster of endothelial cells positive for D2-40, located near a visible lumen clearly separate from adjacent micro-vessels and other connective tissue components.
- 8 -
The lymphatic molecular marker VEGFR-3 was analyzed in all 126 cases and instances of positive expression of VEGFR-3 were assessed. Micro-vessel counts were performed by one pathologist, blinded to the patient’s pathologic and clinical status. The mean value of micro-vessel densities was calculated for each patient blindly. The following grading system was used: Grade 1 (<30%); 1, Grade 2 (30-60%); Grade 3 (>60%). The number of VEGFR3-positive structures per millimeter squared of the stained area was evaluated by the image analysis system(Fig. 3).
- 9 -
Fig. 3.VEGFR-3 Immunostain.VEGFR-3 immunostain showed diffuse cytoplasmic
- 10 - 4. Imaging and Imaging Analysis
A board-certified radiologist with 11 years of experience in thyroid US performed preoperative US examinations of the thyroid lesions and cervical lymph nodes, using a Logiq 9 (General Electric, Milwaukee, WI, USA) with a high-frequency 13 MHz linear transducer.US images were taken using the scanning protocol and in all cases included both transverse and longitudinal real-time imaging of the thyroid nodules with the use of representative Digital Imaging and Communications in Medicine images. Analysis of the US images includedcomparisons of echogenicity, orientation, shape, margin, and calcifications. Echogenicity of the solid portion was classified as hypoechogenicity or marked hypoechogenicity. Markedhypoechogenicity was defined as decreased echogenicity as compared to the strap muscles and hypoechogenicity was defined as decreased echogenicity compare to the thyroid parenchyma (Kim et al., 2002). Orientation was categorized as non-parallel (greater in its anteroposterior dimension than transverse dimension) or non-parallel. The shape of the nodule was categorized as ovoid to round or irregular (when a nodule was not ovoid to round). Margins were classified as well-defined smooth, microlobulated or spiculated, and indistinct (Moon et al., 2008). “Well defined smooth margin” was categorized when line could be followed along the margin of nodule, and “microlobulated” was categorized when more than 80% of the margin was defined with small lobulations less than 4mm in size, and “speculated” was defined by having jagged edge with sharp demarcation. “Indistinct” was categorized when the tumor was not clearly defined from surrounding parenchyma (Moon et al., 2008; Moon et al., 2009; Park et al., 2009; Moon et al., 2011). Calcifications were noted whenhyperechoic foci without acousticshadows were
- 11 -
present regardless of size. Also each US feature was analyzed for malignant nodules that are smaller than 1cm and larger sized nodules (>1 cm).
5.Statistical Analysis
The statistical significance of differences between Group 1 and Group 2 were determined using t-tests and chi-square tests. Comparisons between the two groups were analyzed for nodule size, multiplicity, and extrathyroid extension state using chi-square tests and t-tests. The odds ratios (ORs) and 95% confidence intervals (CIs) of each factor and immunochemical stain were calculated using logistic regression analysis. US features of main thyroid malignant nodule were compared between the groups. Multivariate logistic regression analysis was done to assess the independent associations of cervical LNM with statistically significant predictive factors in univariateanlaysis with adjustments for various prognostic factors. Statistical analyses were performed using Stata version 11 (StataCorp LP, College Station, TX, USA). All reported P values are 2-tailed, and statistical significance was set at P <0.05.
- 12 - II. RESULTS
1. Univariate analysis
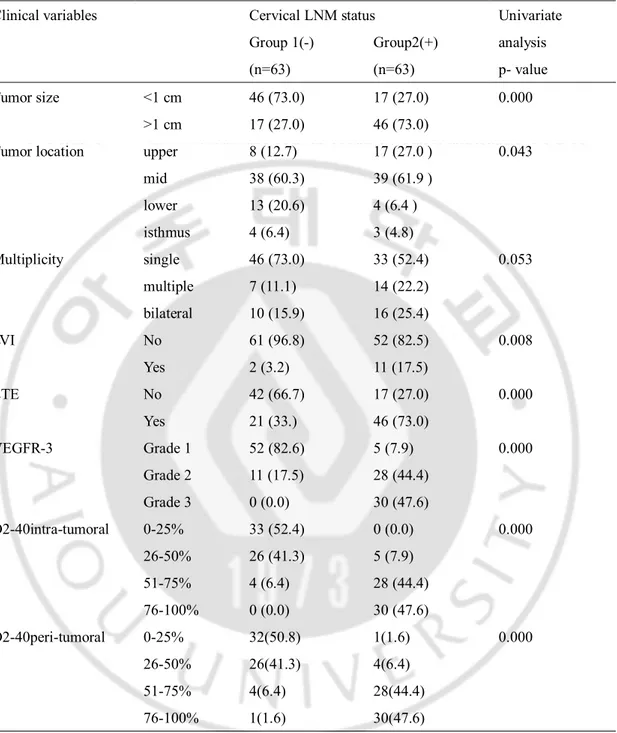
Table 1 summarizes comparisons of the two groups for each factor. Larger tumor size, upper location, lymphovascular invasion, and extrathyroid extension were all significantly more common in group 2 (p<0.001) than in group 1. D2-40 and VEGFR-3 were positive in the endothelial cells of lymph vessels and identified tumor emboli in lymph vessels, though D2-40 did not react with the endothelium of blood vessels. For group 1, the median percentage of VEGFR-3 was 20 (0-30) and D2-40 was 13 (7-23), while for group 2 the median percentage of VEGFR-3 was 80 (70-90) and D2-40 was 78 (54-114). When VEGFR staining was analyzed according to nodule size, the infracentimetric nodules of group 1 showed a higher percentage of absent or weak staining whereas larger nodules in group 2 more frequently showed moderate to strong intensities of VEGFR staining. For the quantification of lymphatic vessel staining for VEGFR, the lower quantile was significantly more frequent in group 1 and the higher quantile was more frequently seen in group 2 (26% vs. 73.68% P<0.001). Intratumoral D2-40 staining was present at the higher quantile in group 2 (22% vs.77.4% p<0.001) and similar results were foundin a comparison of the 2 quantiles with peritumoral D2-40 staining in the two groups (20.6% vs 79.4% p=0.000). The number of VEGFR3-positive structures calculated in thyroid malignant nodules with LNM was significantly higher (p<0.001) than that calculated for a nodule without LNM.
- 13 -
Table 1. Distribution of clinical and pathological risk factors of patients with no cervical LNM (Group1) compared to patients with LNM (Group 2) in age-sex matched patients
Clinical variables Cervical LNM status Univariate
analysis p- value Group 1(-) (n=63) Group2(+) (n=63) Tumor size <1 cm 46 (73.0) 17 (27.0) 0.000 >1 cm 17 (27.0) 46 (73.0)
Tumor location upper 8 (12.7) 17 (27.0 ) 0.043
mid 38 (60.3) 39 (61.9 ) lower 13 (20.6) 4 (6.4 ) isthmus 4 (6.4) 3 (4.8) Multiplicity single 46 (73.0) 33 (52.4) 0.053 multiple 7 (11.1) 14 (22.2) bilateral 10 (15.9) 16 (25.4) LVI No 61 (96.8) 52 (82.5) 0.008 Yes 2 (3.2) 11 (17.5) ETE No 42 (66.7) 17 (27.0) 0.000 Yes 21 (33.) 46 (73.0) VEGFR-3 Grade 1 52 (82.6) 5 (7.9) 0.000 Grade 2 11 (17.5) 28 (44.4) Grade 3 0 (0.0) 30 (47.6) D2-40intra-tumoral 0-25% 33 (52.4) 0 (0.0) 0.000 26-50% 26 (41.3) 5 (7.9) 51-75% 4 (6.4) 28 (44.4) 76-100% 0 (0.0) 30 (47.6) D2-40peri-tumoral 0-25% 32(50.8) 1(1.6) 0.000 26-50% 26(41.3) 4(6.4) 51-75% 4(6.4) 28(44.4) 76-100% 1(1.6) 30(47.6)
LVI; lymphovascular invasion, ETE; extrathyroid extension,
- 14 -
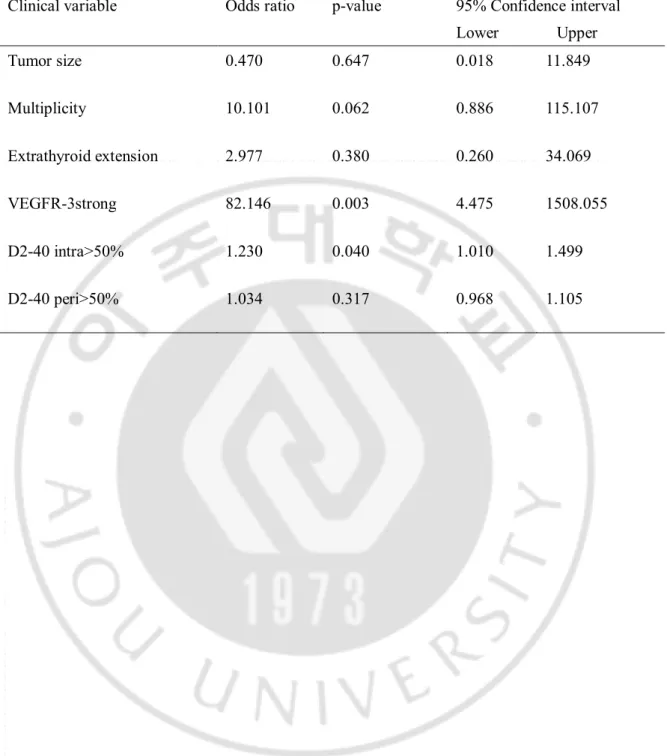
2. Multivariate analysis
Multivariate logistic analysis was performedto assess the independent associations of lateral LNM with statistically significant predictive factors in univariate analysis with adjustment for various established clinico-pathological prognostic factors (larger tumor size, upper location, lymphovascular invasion, and extrathyroid extension) in age sex matched pair patients. Table 2 summarizes the odds ratios and confidence intervals of the factorswhich showed statistical significance in univariateanlaysis. The presence of intratumorallymphatics using D2-40 higher than 50% remained associated with the presence of nodal metastases at presentation (odds 1.23, CI 1.01 -1.499, P =0.04) and VEGFR-3>30% remained significant with odds ratio of 82.146, confidence interval of 4.475-1508.055, p value of 0.003.
- 15 -
Table 2.Multivariate anlaysis of risk factors for cervicallymph node metastasis.
Clinical variable Odds ratio p-value 95% Confidence interval Lower Upper Tumor size 0.470 0.647 0.018 11.849 Multiplicity 10.101 0.062 0.886 115.107 Extrathyroid extension 2.977 0.380 0.260 34.069 VEGFR-3strong 82.146 0.003 4.475 1508.055 D2-40 intra>50% 1.230 0.040 1.010 1.499 D2-40 peri>50% 1.034 0.317 0.968 1.105
- 16 -
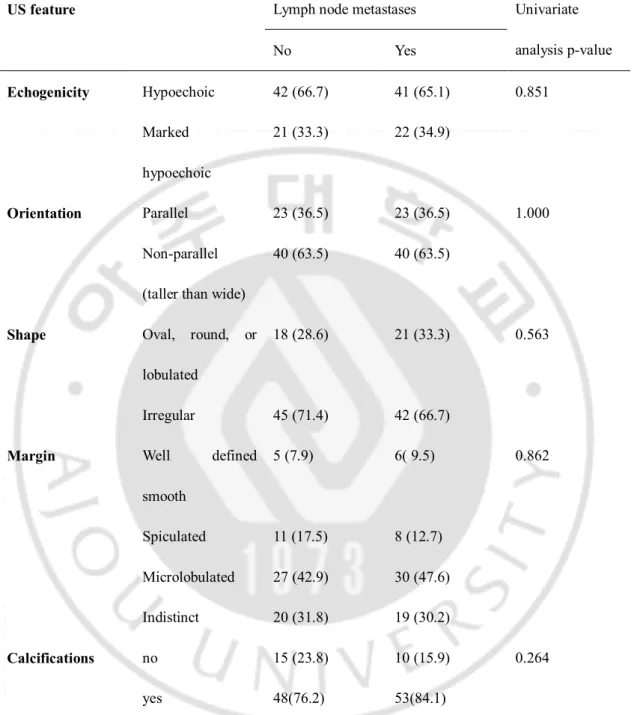
3. Imaging analysis
There were no significant differences between groups 1 and 2 for US features including echogenicity, orientations, shape, and margin. Although calcifications were found to be higher in group 2, (84% vs. 76% p=0.264) the difference was not statistically significant. The comparisons of various US features are summarized in table 3
.
- 17 -
Table 3. Comparisons of US features of patients with cervical neck lymph node metastasis and those of patients with no LNM in age-sex matched patients (n=126).
US feature Lymph node metastases Univariate
analysis p-value No Yes Echogenicity Hypoechoic 42 (66.7) 41 (65.1) 0.851 Marked hypoechoic 21 (33.3) 22 (34.9) Orientation Parallel 23 (36.5) 23 (36.5) 1.000 Non-parallel
(taller than wide)
40 (63.5) 40 (63.5)
Shape Oval, round, or lobulated
18 (28.6) 21 (33.3) 0.563
Irregular 45 (71.4) 42 (66.7)
Margin Well defined
smooth 5 (7.9) 6( 9.5) 0.862 Spiculated 11 (17.5) 8 (12.7) Microlobulated 27 (42.9) 30 (47.6) Indistinct 20 (31.8) 19 (30.2) Calcifications no 15 (23.8) 10 (15.9) 0.264 yes 48(76.2) 53(84.1)
- 18 -
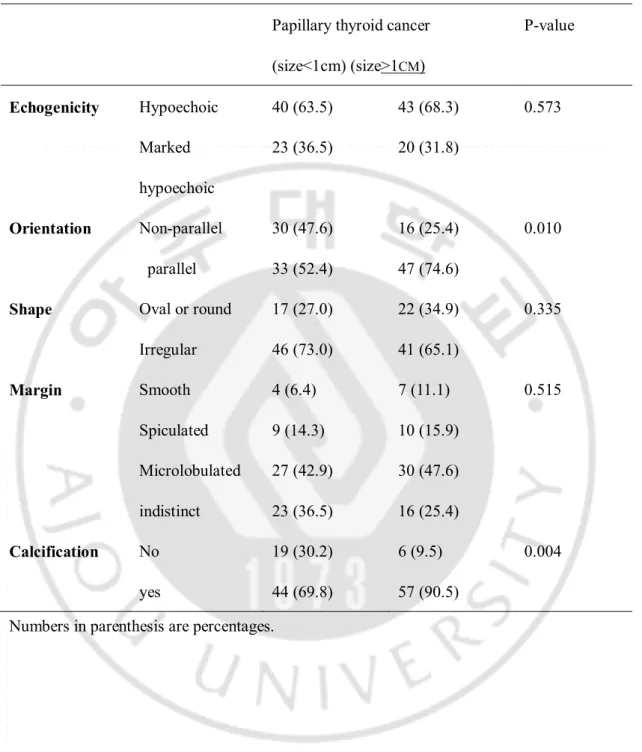
Orientations and calcifications were significantly different (p=0.001) in malignancies with size less than 1cm. Smaller nodules more frequently showed a taller than wide feature whereas larger nodules more frequently showed parallel orientations (Table 4).Furthermore, calcifications were much more frequent in the larger group which had rates upto 90% with p=0.004. Others showed no statistically significant differences.
- 19 -
Table 4.Comparisons of US features suggesting malignancy between PMC and PTC in age-sex matched patients.
Papillary thyroid cancer (size<1cm) (size>1CM) P-value Echogenicity Hypoechoic 40 (63.5) 43 (68.3) 0.573 Marked hypoechoic 23 (36.5) 20 (31.8) Orientation Non-parallel 30 (47.6) 16 (25.4) 0.010 parallel 33 (52.4) 47 (74.6)
Shape Oval or round 17 (27.0) 22 (34.9) 0.335 Irregular 46 (73.0) 41 (65.1) Margin Smooth 4 (6.4) 7 (11.1) 0.515 Spiculated 9 (14.3) 10 (15.9) Microlobulated 27 (42.9) 30 (47.6) indistinct 23 (36.5) 16 (25.4) Calcification No 19 (30.2) 6 (9.5) 0.004 yes 44 (69.8) 57 (90.5)
- 20 -
Ⅳ
. DISCUSSION
PTC is a curable, treatable disease, but occasionally causes recurrences and cervical LNM. In an attempt to establish a reliable prognostic scoring system, most published studies have primarily considered clinical factors such as age and sex, tumor size, and extra thyroidal extensions. Younger patients less than 16 years old, patients older than 45 years, and patients with PTC subtypes such as tall-cell, columnar-cell, and diffuse sclerosing variant types are known to have higher risks for recurrences (Schlumberger, 1998; Beasley et al., 2002a) and additionally, bilateral LNM may be a risk factor for lung metastasis (Lee et al., 2011). The biological behaviors of well differentiated thyroid malignant nodules were not considered when selecting a treatment strategy. Furthermore, the way in which tumors spread via the lymphatic system is not fully understood.
Since PTC can metastasize via the lymphatic channel to a regional cervical lymph node (Shushanov et al., 2000; Yasuoka et al., 2005; Yu et al., 2005; Longatto-Filho et al., 2008; Moriya et al., 2011), and increased LVD is assumed to be one of the most important parameters associated with the aggressive behavior of a malignant tumor (Longatto-Filho et al., 2008), we hypothesized that nodules with more lymphatic vessel systems would have an increased risk of LNM. We do not know whether the existing tumor induces lymphangiogenesis or invades peritumoral vessels so, in addition to D2-40, we also analyzed VEGFR-3. Vascular endothelial growth factor -C, known to be a key factor in lymphatic vessel sprout, is involved in the proliferation and migration of endothelial cells, increased
- 21 -
vascular permeability, and lymphangiogenesis(Byrne et al., 2005; Yamazaki and Morita, 2006) and its receptor, VEGFR-3, was shown to be essential to lymphatic vessel development in embryos and in the maintenance of lymphatic endothelial cells in adults (Shushanov et al., 2000). There are relatively few reports about LVD and the expression of Vascular endothelial growth factor -D in malignant thyroid nodules and the relationships of intratumoral LVD and peritumoral LVD with LNM have not been previously published, to the best of our knowledge. In this study, we quantitated both lymphatic markers intratumorally and peritumorally since published reports have shown contradicting results. Some reports claim that there are relationships between increased intratumorallymphatics and an association with the spread of tumors to regional lymph nodes (Beasley et al., 2002b; Hall et al., 2003; Giorgadze et al., 2005; Petersson et al., 2009), while, in contrast, there are also published data showing that there are no relationships between the intratumoral LVD related to LNM or distant metastasis in breast cancer (Britto et al., 2009). A study by Garcia et al. showed that peritumoral LVD was not correlated with LNM, along with other published reports showing that LVD is more strongly associated with a good prognosis (de la Torre et al., 2006; Garcia et al., 2010). This result showed contradicting results suggesting that higher LVD of PTC nodules shows significantly increased cervical LNM. In this study, intratumoral LVD as well as peritumoral LVD showed high correlations with cervical LNM making it an important factor indicating tumor aggressiveness. Few authors suggested that peritumoral LVD was related to higher capsular invasion (p=0.045), along with other studies, and that it is the peritumoral, not the intratumoral, LVD that is related with aggressive cancer behavior (Giorgadze et al., 2005; Gombos et al., 2005; Garcia et al., 2010). In an age-
- 22 -
and sex-adjusted univariate setting, both factors were highly associated with cervical LNM and when we analyzed these factors in a multivariate setting, both were independent factors among the tumor size, multiplicity, bilaterality, and extrathyroid extension. Thus, this data indicates that expression levels of VEGFR3 and D2-40 should be considered with respect to tumor aggressiveness and cervical LNM. Although lymphovascular invasion (LVI) seen with H-E staining did show statistically significant differences between the two groups, 52 cases (82.5%) in group 2 did not show LVI with H-E staining whereas a higher percentage of VEGFR-3 and more than 50% of intratumoral D2-40 stained vessels were visualized in group 2 nodules. We did not evaluate the LVI seen with these two markers and correlated with cervical LNM, but we quantitated the LVD with cervical LNM state because this study was initially designed to compare the LVD in the two groups with correlations to US features. Pathological features such as larger size, extra-thyroid extension, and positive immunostaining for D2-40 and VEGFR-3 to evaluate the LVD can be used as strong predictive prognostic markers and have the potential to play significant roles in pathological routine workup of thyroid cancer with cervical LNM.
Thyroid cancer with cervical LNM, showing strong VEGFR-3 staining and increased LVD with D2-40 staining did not show any correlations with assorted US features such as echogenicity, orientation, shape, margin, and calcifications. None of these factors showed any significant differences between the two study groups. Our hypothesis when designing this study was that since water or vessels can show low echogenicity compared to solid mass comprised of compact cells, a tumor with higher LVD would be correlated with low or marked echogenicity, but the observed effect was not statistically significant. We also
- 23 -
hypothesized that spiculation or ill defined margins would be seen more often with an aggressive tumor with increased peritumoral LVD invasion, but the results for this factor were also not significant. However, Ito et al. reported that ill defined edges were positively associated with a more aggressive thyroid cancer frequently showing lateral LNM (Ito et al., 2005) and that the feature may be used as a marker of a more aggressive cancer. In contrast, in this study we observed that nodules with spiculation or irregular shapes occurred more frequently in group 1 with no statistical significance. This findings show that US features vary according to the size of the malignant nodule, rather than the aggressiveness of the tumor, showing more frequent “taller than wide” appearance in microcarcinoma (p=0.010) and more associated calcifications in PTCs larger than 1 cm. We attempted to identify US features associated with aggressive malignant features but none of the features examined were associated with cervical LNM and were, instead, more strongly associated with features of microcarcinoma. Calcifications were frequently involved in aggressive thyroid cancers with moderate staining of the lymphatic vessels.
One limitation of this study is that we analyzed clinical and pathological data retrospectively. We used age- and sex-matched pair data in order to concentrate on pathological factors and it was not possible to perform staining procedures for all the surgical specimens. Furthermore, it is possible that a considerable amount of selection bias may have affected this study by comparing patients with no cervical LNM in the final pathology group with a cervical LNM-positive group that included both central and lateral LNM-positive patients. We also excluded patients with central LNM because a considerable number of cases showed micrometastasis to the central lymph nodes and such cases have
- 24 -
little clinical impact due to the routine surgical removal of the ipsilateral central lymph nodes, but it may be considered as another form of selection bias. We did not follow up the patients with high risk factors to track recurrences since this study was not designed to use a prospective cohort and it was not focused on how LVD relates to survival, but specifically how it is related to cervical LNM state. In the future, it would be worthwhile to investigate the relationship between LVD and patient survival. Quantitation of intratumoral LVD and peritumoral LVD by a counting method revealed an association (P= 0.027) between high intratumoral LVD (highest tertile) and LNM in PTC, but in this experimental setting, we were unable to conclude if this was newly developed lymphangiogenesis or if existing lymphatic vessel density caused this result. To overcome this problem VEGFR-3 was also stained to confirm the presence of existing lymphatic channels. Quantifications were obtained but due to the generally weak, moderate, or strong nature of the staining for VEGFR-3, it was difficult to compare the association between the existing vasculature and newly developed lymphangiogenesis.
- 25 -
Ⅴ
. CONCLUSION
In predicting the outcome, prognosis, and recurrence of thyroid papillary cancer, not only the clinical factors should be considered but also lymphangiogenesis of thyroid nodules since it shows a strong clinical relevance in cervical LNM. D2-40 or VEGFR3 staining can be a predictor of LNM and cases with high D2-40 staining should be carefully followed for lymph node recurrence. No specific US feature was found to be related with cervical LNM.
- 26 -
REFERENCES
1. Baek SK, Jung KY, Kang SM, Kwon SY, Woo JS, Cho SH, Chung EJ: Clinical risk factors associated with cervical lymph node recurrence in papillary thyroid carcinoma. Thyroid 20: 147-152, 2009
2. Beasley NJ, Lee J, Eski S, Walfish P, Witterick I, Freeman JL: Impact of nodal metastases on prognosis in patients with well-differentiated thyroid cancer. Arch
Otolaryngol Head Neck Surg 128: 825-828, 2002a
3. Beasley NJ, Prevo R, Banerji S, Leek RD, Moore J, van Trappen P, Cox G, Harris AL, Jackson DG: Intratumoral lymphangiogenesis and lymph node metastasis in head and neck cancer. Cancer Res 62: 1315-1320, 2002b
4. Britto AV, Schenka AA, Moraes-Schenka NG, Alvarenga M, Shinzato JY, Vassallo J, Ward LS: Immunostaining with D2-40 improves evaluation of lymphovascular invasion, but may not predict sentinel lymph node status in early breast cancer. BMC
Cancer 9: 109, 2009
5. Byar DP, Green SB, Dor P, Williams ED, Colon J, van Gilse HA, Mayer M, Sylvester RJ, van Glabbeke M: A prognostic index for thyroid carcinoma. A study of the E.O.R.T.C. Thyroid Cancer Cooperative Group. Eur J Cancer 15: 1033-1041, 1979
6. Byrne AM, Bouchier-Hayes DJ, Harmey JH: Angiogenic and cell survival functions of vascular endothelial growth factor (VEGF). J Cell Mol Med 9: 777-794, 2005 7. Cappelli C, Castellano M, Braga M, Gandossi E, Pirola I, De Martino E, Agosti B,
Rosei EA: Aggressiveness and outcome of papillary thyroid carcinoma (PTC) versus microcarcinoma (PMC): a mono-institutional experience. J Surg Oncol 95: 555-560, 2007
8. de la Torre NG, Buley I, Wass JA, Turner HE: Angiogenesis and lymphangiogenesis in thyroid proliferative lesions: relationship to type and tumour behaviour. Endocr Relat Cancer 13: 931-944, 2006
- 27 -
9. DeGroot LJ, Kaplan EL, McCormick M, Straus FH: Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metab 71: 414-424, 1990 10. Frates MC, Benson CB: Ultrasonographically guided thyroid biopsy. J Ultrasound
Med 20: 1261-1262, 2001
11. Garcia EA, Simoes K, Wakamatsu A, Ressio RA, Alves VA, Longatto-Filho A, Camargo RS: Lymphatic vessel density and VEGF-C expression are significantly different among benign and malignant thyroid lesions. Endocr Pathol 21: 101-107, 2010
12. Giorgadze TA, Baloch ZW, Pasha T, Zhang PJ, Livolsi VA: Lymphatic and blood vessel density in the follicular patterned lesions of thyroid. Mod Pathol 18: 1424-1431, 2005
13. Gombos Z, Xu X, Chu CS, Zhang PJ, Acs G: Peritumoral lymphatic vessel density and vascular endothelial growth factor C expression in early-stage squamous cell carcinoma of the uterine cervix. Clin Cancer Res 11: 8364-8371, 2005
14. Hall FT, Freeman JL, Asa SL, Jackson DG, Beasley NJ: Intratumoral lymphatics and lymph node metastases in papillary thyroid carcinoma. Arch Otolaryngol Head
Neck Surg 129: 716-719, 2003
15. Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS: Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery 114: 1050-1057; discussion 1057-1058, 1993
16. Ito Y, Fukushima M, Tomoda C, Inoue H, Kihara M, Higashiyama T, Uruno T, Takamura Y, Miya A, Kobayashi K, Matsuzuka F, Miyauchi A: Prognosis of patients with papillary thyroid carcinoma having clinically apparent metastasis to the lateral compartment. Endocr J 56: 759-766, 2009
- 28 -
17. Ito Y, Kihara M, Takamura Y, Kobayashi K, Miya A, Hirokawa M, Miyauchi A: Prognosis and prognostic factors of papillary thyroid carcinoma in patients under 20 years. Endocr J 29:1007-1011, 2012a
18. Ito Y, Kobayashi K, Tomoda C, Uruno T, Takamura Y, Miya A, Matsuzuka F, Kuma K, Miyauchi A: Ill-defined edge on ultrasonographic examination can be a marker of aggressive characteristic of papillary thyroid microcarcinoma. World J
Surg 29: 1007-1011; discussion 1011-1002, 2005
19. Ito Y, Kudo T, Kihara M, Takamura Y, Kobayashi K, Miya A, Miyauchi A: Prognosis of low-risk papillary thyroid carcinoma patients: Its relationship with the size of primary tumors. Endocr J 59: 119-125, 2012b
20. Ito Y, Miyauchi A, Kihara M, Takamura Y, Kobayashi K, Miya A: Relationship between prognosis of papillary thyroid carcinoma patient and age: A retrospective single-institution study. Endocr J, 2012c
21. Jeong JJ, Lee YS, Lee SC, Kang SW, Chung WY, Chang HS, Seo WY, Song KJ, Park CS: A scoring system for prediction of lateral neck node metastasis from papillary thyroid cancer. J Korean Med Sci 26: 996-1000, 2011
22. Kahn HJ, Marks A: A new monoclonal antibody, D2-40, for detection of lymphatic invasion in primary tumors. Lab Invest 82: 1255-1257, 2002
23. Kawaura K, Fujii S, Murata Y, Hasebe T, Ishii G, Itoh T, Sano Y, Saito N, Ochiai A: The lymphatic infiltration identified by D2-40 monoclonal antibody predicts lymph node metastasis in submucosal invasive colorectal cancer. Pathobiology 74: 328-335, 2007
24. Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, Yoo HS: New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol 178: 687-691, 2002
- 29 -
25. Kukk E, Lymboussaki A, Taira S, Kaipainen A, Jeltsch M, Joukov V, Alitalo K: VEGF-C receptor binding and pattern of expression with VEGFR-3 suggests a role in lymphatic vascular development. Development 122: 3829-3837, 1996
26. Kuo SF, Chao TC, Hsueh C, Chuang WY, Yang CH, Lin JD: Prognosis and risk stratification in young papillary thyroid carcinoma patients. Endocr J 55: 269-275, 2008
27. Kwak JY, Kim EK, Kim MJ, Son EJ, Chung WY, Park CS, Nam KH: Papillary microcarcinoma of the thyroid: predicting factors of lateral neck node metastasis.
Ann Surg Oncol 16: 1348-1355, 2009
28. Lee YS, Lim YS, Lee JC, Wang SG, Kim IJ, Son SM, Lee BJ: Clinical implications of bilateral lateral cervical lymph node metastasis in papillary thyroid cancer: a risk factor for lung metastasis. Ann Surg Oncol 18: 3486-3492, 2011
29. Longatto-Filho A, Pinheiro C, Ferreira L, Scapulatempo C, Alves VA, Baltazar F, Schmitt F: Peritumoural, but not intratumoural, lymphatic vessel density and invasion correlate with colorectal carcinoma poor-outcome markers. Virchows Arch 452: 133-138, 2008
30. Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, Kwak JY, Lee JH, Lee YH, Na DG, Park JS, Park SW: Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean
J Radiol 12: 1-14, 2011
31. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, Kim J, Kim HS, Byun JS, Lee DH: Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology 247: 762-770, 2008
32. Moon WJ, Kwag HJ, Na DG: Are there any specific ultrasound findings of nodular hyperplasia ("leave me alone" lesion) to differentiate it from follicular adenoma?
- 30 -
33. Moriya H, Ohbu M, Kobayashi N, Tanabe S, Katada N, Futawatari N, Sakuramoto S, Kikuchi S, Okayasu I, Watanabe M: Lymphatic tumor emboli detected by D2-40 immunostaining can more accurately predict lymph-node metastasis. World J Surg 35: 2031-2037, 2011
34. Nam-Goong IS, Kim HY, Gong G, Lee HK, Hong SJ, Kim WB, Shong YK: Ultrasonography-guided fine-needle aspiration of thyroid incidentaloma: correlation with pathological findings. Clin Endocrinol (Oxf) 60: 21-28, 2004
35. Park JY, Lee HJ, Jang HW, Kim HK, Yi JH, Lee W, Kim SH: A proposal for a thyroid imaging reporting and data system for ultrasound features of thyroid carcinoma. Thyroid 19: 1257-1264, 2009
36. Petersson F, Diwan AH, Ivan D, Gershenwald JE, Johnson MM, Harrell R, Prieto VG: Immunohistochemical detection of lymphovascular invasion with D2-40 in melanoma correlates with sentinel lymph node status, metastasis and survival. J
Cutan Pathol 36: 1157-1163, 2009
37. Riemann B, Kramer JA, Schmid KW, Dralle H, Dietlein M, Schicha H, Sauerland C, Frankewitsch T, Schober O: Risk stratification of patients with locally aggressive differentiated thyroid cancer. Results of the MSDS trial. Nuklearmedizin 49: 79-84, 38. Schlumberger MJ: Papillary and follicular thyroid carcinoma. N Engl J Med 338:
297-306, 1998
39. Sebastian SO, Gonzalez JM, Paricio PP, Perez JS, Flores DP, Madrona AP, Romero PR, Tebar FJ: Papillary thyroid carcinoma: prognostic index for survival including the histological variety. Arch Surg 135: 272-277, 2000
40. Shushanov S, Bronstein M, Adelaide J, Jussila L, Tchipysheva T, Jacquemier J, Stavrovskaya A, Birnbaum D, Karamysheva A: VEGFc and VEGFR3 expression in human thyroid pathologies. Int J Cancer 86: 47-52, 2000
41. Tennvall J, Biorklund A, Moller T, Ranstam J, Akerman M: Is the EORTC prognostic index of thyroid cancer valid in differentiated thyroid carcinoma?
- 31 -
Retrospective multivariate analysis of differentiated thyroid carcinoma with long follow-up. Cancer 57: 1405-1414, 1986
42. Weidner N, Semple JP, Welch WR, Folkman J: Tumor angiogenesis and metastasis--correlation in invasive breast carcinoma. N Engl J Med 324: 1-8, 1991
43. Yamazaki Y, Morita T: Molecular and functional diversity of vascular endothelial growth factors. Mol Divers 10: 515-527, 2006
44. Yasuoka H, Nakamura Y, Zuo H, Tang W, Takamura Y, Miyauchi A, Nakamura M, Mori I, Kakudo K: VEGF-D expression and lymph vessels play an important role for lymph node metastasis in papillary thyroid carcinoma. Mod Pathol 18: 1127-1133, 2005
45. Yu XM, Lo CY, Chan WF, Lam KY, Leung P, Luk JM: Increased expression of vascular endothelial growth factor C in papillary thyroid carcinoma correlates with cervical lymph node metastases. Clin Cancer Res 11: 8063-8069, 2005
- 32 - -국문 요약-