Glenoid rim fractures are rare, and a consensus does not exist for the gold standard of treatment. Previous studies have shown favorable outcomes for glenoid rim fractures after open reduction and internal fixation and after arthroscopic treatment with perpendicular fixation. Yet these treatment methods have been associated with neurovascular injury and complications relating to the use of solid suture anchors. In this study, we investigated a novel surgical method for glenoid rim fractures that would address these limitations associated with current treatment methods. We employed two novel approaches: buttress Kirschner wire (K-wire) fixation through arthroscopic portals to reduce neurovascular injury;
and insertion of soft suture anchors as an alternative to solid anchors. The purpose of this technical note is to inform the clinical audience about our novel surgical technique that utilizes buttress K-wires and soft suture anchors for displaced fractures of the anterior glenoid rim.
Keywords: Glenoid rim fracture; Soft suture anchor; K-wire
Arthroscopy-assisted tension band fixation with buttress Kirschner wires and soft suture anchors for glenoid rim fractures
Chang Hyuk Choi, Sung Guk Kim, Jun Ho Nam, Hee Soo Kim, Byung Hoon Kwack
Shoulder and Elbow Joint Service, Department of Orthopedic Surgery, Daegu Catholic University Medical Center, Daegu, Korea
Copyright © 2016 Korean Arthroscopy Society and Korean Orthopedic Society for Sports Medicine. All rights reserved.
CC This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/
by-nc/4.0) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 9, 2016; Revised May 3, 2016; Accepted May 12, 2016
Correspondence to: Byung Hoon Kwack, Department of Orthopedic Surgery, School of Medicine, Catholic University of Daegu, 33 Duryugongwon-ro 17-gil, Nam-gu, Daegu 42472, Korea. Tel: +82-53-650-4054, Fax: +82-53-626-4272, E-mail: kwackbyunghoon@nate.com Arthroscopy and
Orthopedic Sports Medicine
AOSM
INTRODUCTION
Glenoid rim fractures are usually accompanied by an avulsion of the capsulolabral-ligament complex and caused by a traumatic glenohumeral dislocation. Indica- tions for a surgical operation include instability of the shoulders, a displacement of > 5 mm, and a fragment that comprise > 21% of the anterior articular surface or
> 33% of the posterior articular surface [1]. In the past, open reduction and internal fixation (ORIF) has been recommended as the first line of treatment for acute an- terior glenoid rim fractures, but the need for extensive dissection has limited its use. Extensive dissection dur- ing operation has been associated with complications such as subscapularis insufficiency with internal rotation deficit and post-traumatic osteoarthritis [2]. These ORIF- related limitations have necessitated the implementation of studies in search of an alternative method; for this end,
studies have revealed arthroscopy-based methods as the most promising candidate for glenoid rim fractures for their excellent visualization, minimal soft-tissue dissec- tion, anatomical fracture reduction, minimal bleeding, and short operation time.
Several reports have shown favorable outcomes for glenoid rim fractures after arthroscopic treatments, which includes arthroscopy with percutaneous exter- nal Kirschner (K)-wiring or screw fixation, arthroscopic trans-glenoid suture repair, and arthroscopic anchor fixa- tion (single or double-row repair) [3–8]. Yet these reports have shown that the effectiveness of these techniques varies depending on the size and the extent of fragmenta- tion and displacement of the fracture. Further, a perpen- dicular fixation of the glenoid requires a medial approach in terms of portal insertion; and a high risk of damage to the neurovascular structures, such as the cephalic vein, the musculocutaneous nerve, and the inferior branch of
the suprascapular nerve, has been shown to be attributed to this approach [7]. Other postoperative complications are also associated with arthroscopy: arthroscopic fixa- tion with anchors or screws may cause a step-off of the glenoid [8]; and breakage in solid anchors may result in loose bodies, which in turn may potentiate articular car- tilage injury [9]. To compensate for these disadvantages associated with arthroscopic procedures, we sought a novel surgical approach for treatment from a different perspective. We used buttress K-wire fixation through an anteroinferior (AI) arthroscopic portal to minimize neurovascular injury and soft suture anchors as an al- ternative to solid anchors. We fixed bone fragments with buttress K-wires in a tension band fashion and tried to preserve the remnant capsulolabral-ligament complex as much as possible. We recommend this technique for the fixation of small fracture fragments or fragmented frac- tures, where achieving a stable screw fixation is difficult and ascertaining as high a capsulolabral complex stabil- ity as possible is crucial.
CASE REPORT
A 36-year-old man with an anterior dislocation of the right shoulder, which was incurred whilst playing volley- ball, was admitted to our hospital. Before his admittance the patient’s dislocated shoulder had been reduced at the nearest emergency department and placed in a sling. On the same day, the patient had sustained a second disloca- tion whilst attempting to elevate his arm; his shoulder was reduced again. Despite receiving a reduction treat- ment, the patient’s right shoulder remained unstable, so the patient was admitted to our hospital three days of the initial dislocation. We performed physical and radiologi- cal examinations of the patient. Using plain radiography, we observed a medially displaced glenoid fracture (Fig.
1A). On computed tomography (CT) scans, we demon- strated a displaced AI glenoid rim fracture, which was categorized as a type Ia fracture in accordance to Ide- berg’s classification system (Fig. 1B, C). The proportion of the fragment size in relation to the total glenoid area was
Fig. 1. (A) Plain radiograph shows an articular glenoid fracture (arrows). (B) A computed tomography (CT) scan shows a displaced glenoid fracture with a medial dislocation of 5.4 mm. (C) A three-dimensional CT scan shows a multifragmented fracture of the anterior glenoid rim (arrows). (D) Glenoid height was measured as the distance between the superior pole of the glenoid (12 o’clock position) and the inferior pole (6 o’clock position). (E) The proportion of the fracture encompassing the glenoid surface was 26.3%, which was calculated as the percentage of the area of the bony fragment (area within the dotted line) over the total surface area of the inferior glenoid circle (area within the solid line).
A B C
D E
26.3%, which was calculated as described by Sugaya et al.
[10] (Fig. 1D, E). The fragment was medially dislocation by 5.4 mm (Fig. 1B).
The patient was placed under general anesthesia and in a beach-chair position. Standard posterior and an- terosuperior (AS) portals were established for diagnostic arthroscopy. Diagnostic arthroscopy showed a fracture of the AI glenoid rim that was medially displaced with con- comitant osteochondral defect. The labrum was partially attached to the bone fragment, being detached from the superior to the inferior end of the fragment. After the di- agnostic arthroscopy, we established an AI portal at the upper margin of the subscapularis tendon through which a probe was inserted to mobilize the fracture fragment.
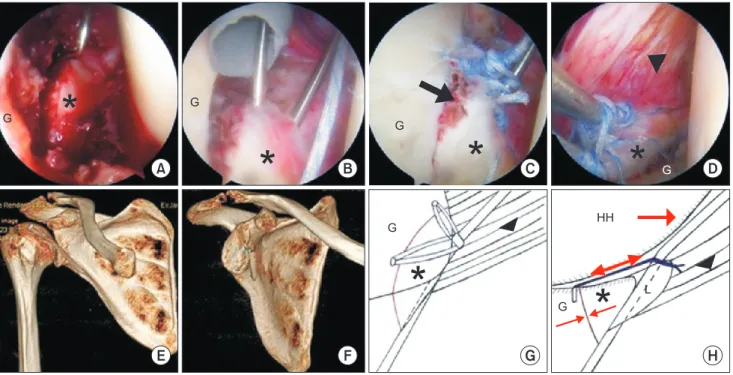
We inserted a 1.2 mm K-wire, which was to be used as a joystick, via the AS portal into the superior end of the fragment, where osteochondral defect due to a small displacement of the fragment existed. Then, the K-wire joystick was used to reduce the fracture (Fig. 2A). After making this provisional reduction, we inserted anothea
1.2 mm K-wire through the AI portal. The K-wire was in- serted through the anterior labrum, the anterior cortex of the fragment, and the glenoid neck (Fig. 2B). We inserted a soft anchor (Y-knot; ConMed Linvatec, Largo, FL, USA) into the articular surface of the inferior margin of the fracture and made an in situ labral repair. This procedure was repeated with a second soft anchor but into the su- perior margin. After we removed the provisional K-wire, we tied the remaining suture strands around the but- tress K-wire in a tension band fashion (Fig. 2C). Through the AS viewing portal, we confirmed that the remaining capsulolabral-ligament complex was well preserved (Fig.
2D). Lastly, the buttress K-wire was cut at the subcutane- ous level. Postoperative radiographs confirmed anatomi- cal reduction of the fracture and a correct placement of the K-wire, which showed slight bending at the glenoid margin presumably induced by the reduction pressure of the humeral head (Fig. 2E–G). The results of CT not only affirmed satisfactory reduction but also K-wire bending and bone defect at the fracture site.
Fig. 2. Arthroscopic findings of the right shoulder from the posterior portal. (A) The fracture fragment of the anterior glenoid rim is displaced medially.
Inserted via the anterosuperior (AS) portal, the provisional Kirschner wire (K-wire) was used as a joystick to reduce the fracture. (B) The anterior glenoid rim fracture was reduced with the provisional K-wire. The buttress K-wire, which is inserted via the anteroinferior portal, was passed through the an- terior labrum, the anterior cortex of the fragment, and the glenoid neck. (C) After removing the provisional K-wire, the remaining suture strands were threaded onto the inferior and superior poles of the K-wire in a tension band fashion. Minimal osteochondral defect (arrow) remained despite strong fixation of the fracture. (D) The remnant capsulolabral-ligament complex, viewed from the AS portal, was preserved. (E, F) Three-dimensional comput- ed tomography scans show slight bending at the glenoid margin that is induced by reduction pressure of the humeral head. (G) A schematic illustration of our novel arthroscopy-assisted tension band fixation with buttress K-wires and soft anchors. (H) A schematic illustration of the tension band effect wherein the distraction force of the remnant capsulolabral-ligament complex and the humeral head volume converts into a compression force at the fracture site. Asterisks, glenoid rim fracture; G, glenoid; arrowheads, capsulolabral-ligament complex; HH, humeral head; L, labrum.
* *
G
G
L HH
E F G H
A B C D
G
*
* * *
G
G
G
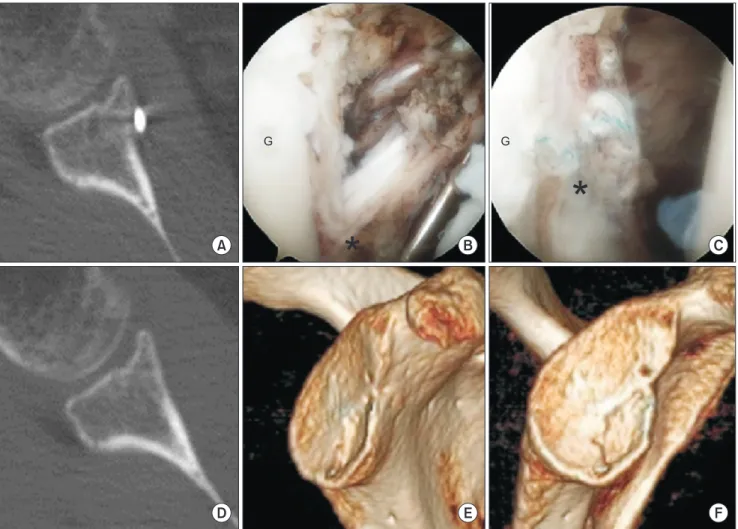
Postoperatively, we encouraged the patient to wear an abduction brace for six weeks. The patient was admin- istered with the following postoperative rehabilitation protocol: simple exercises were started after two postop- erative weeks; the abduction pillow was removed after four weeks; and pendulum exercises and passive ranges of motion were begun after four weeks. Results of CT showed satisfactory bone healing by the third postopera- tive month, but minimal bone defect remained at the articular surface (Fig. 3A). The patient showed a range of motion of 80o of elevation, 0o of external rotation, and L5 internal rotation. We performed a second-look arthros- copy to remove the K-wire and attempted adhesiolysis to promote rapid rehabilitation.
We established standard posterior and AS portals in the patient, who was under interscalene regional anesthesia,
as before and performed second-look arthroscopy. We observed that the initial fracture site was covered by thick granulation tissue and hypertrophic synovium (Fig. 3B).
The buried suture strands of the soft anchors were left as it were after we removed the buttress K-wire. The original site of bone defect was covered with cartilage, and ad- ditional adhesiolysis was applied (Fig. 3C). The patient was begun on postoperative passive and active range of motion exercises straight after the operation. On the fifth postoperative month, the patient presented with the following clinical and radiological findings, which were derived through physical examination and CT, respec- tively: an excellent range of motion (150o of elevation, 30o of external rotation, and L2 internal rotation); a return to daily activities; an anatomically restored glenoid; and an absence of osteoarthritic changes (Fig. 3D–F).
Fig. 3. (A) A computed tomography (CT) scan taken on the third postoperative month shows satisfactory bone healing. (B) A view of the buttress Kirschner wire on the right shoulder after adhesiolysis. (C) The original site of bone defect is covered with granulation tissue and cartilage between the 2 o’clock region and the 6 o’clock region. CT (D) and three-dimensional CT (E, F) scans taken on the fifth postoperative month shows an anatomically restored glenoid and an absence of osteoarthritic changes. Asterisks, glenoid rim fracture; G, glenoid.
G
*
*
G
A B C
D E F
DISCUSSION
A bony fragment or a displacement large enough to trig- ger instability is an indication for an operative treatment [1]. Findings of biomechanical cadaveric studies have shown that a reduction of fractures resulting from glenoid bone loss and chondral-labral defect is essential in order to prevent subsequent instability of the shoulders [1,11].
Nakagawa et al. [12] found that the major of patients ex- hibit severe absorption of bone fragment within a year of primary traumatic shoulder dislocation. In addition, Porcellini et al. [4] reported that arthroscopic treatment of acute bony Bankart lesions is more successful than of chronic ones. Thus, the interest in the treatment of dis- placed glenoid rim fractures through arthroscopic means has been growing.
The limitations of using arthroscopy to stabilize glenoid fractures are depicted by many studies. In their biochem- ical study on cadavers, Marsland and Ahmed [7] reported that inserting percutaneous screws and K-wires inferior to the coracoid through the anterior portal was associated with a substantial risk of damaging the cephalic vein, the musculocutaneous nerve, or the inferior branch of the suprascapular nerve. Further, they suggested that an an- terior percutaneous fixation for the glenoid may increase the risk of neurovascular injury since it requires a more medial approach than a portal insertion into the joint.
Dhawan et al. [9] advised that potential postoperative complications of using bioabsorbable suture anchors, such as foreign body reactions, osteolysis, synovitis, chondrolysis, and implant failure, should be kept in mind when evaluating a differential diagnosis in patients who suffer from persistent pain and from mechanical symp- toms. Using bioabsorbable and metal suture anchors in an arthroscopic Bankart repair, Park et al. [13] ascribed anchor-induced osteolysis to glenoid rim fractures. Simi- larly, using anchors and bioabsorbable compression screws in arthroscopic reduction and fixation, Scheibel et al. [8] observed through radiological evaluation a postop- erative step-off of the glenoid averaging 2 mm (range, 1–3 mm) in seven patients. Barber and Herbert [14] tested the biomechanical analysis of the pullout strengths of vari- ous suture anchors containing a Y-knot; they found that the stiffness of the Y-knot is not significantly different to those of other glenoid anchors.
In our report, we described the use of two novel ap- proaches for the treatment of glenoid rim fractures. We used buttress K-wire fixation through the AI portal to
reduce neurovascular injury and to minimize step-off of the glenoid and soft suture anchors as an alternative to solid suture anchors. Succinctly, we made a provisional reduction of the fragment with a joystick K-wire. Then, we inserted a buttress K-wire into the anterior labrum, the anterior cortex of the fracture fragment, and the glenoid neck. Finally, we used a soft anchor tension band repair approach to stabilize the buttress K-wire. The repair was made on the articular surface of the superior and inferior margins of the fracture. In our novel technique, we sug- gest that a powerful reduction force, which reinforces the buttress effect, is generated by the humeral head volume pushing against the K-wire. Our suggestion follows the argument that the distraction force against the K-wire, exerted by the remnant capsulolabral-ligament complex and by the humeral head volume, converts into a com- pression force at the fracture site, which facilitates the recovery (Fig. 2H).
Our technique is not without potential pitfalls: only one K-wire can be fixed because the number of portals that can be established is limited; and the technique can be used only when the capsulolabral-ligament complex is able to be conserved because the tension band effect ex- erted by the buttress K-wire is dependent on the integrity of this structure.
A precise measurement of the fracture size is essential to determine the most optimal approach for arthroscopic fixation. This is because when sufficient fixation area cannot be ascertained on small fractures the options for treatment becomes limited; for instance, screw fixation is difficult on small bony fragments and suture repairs or simple K-wire fixation is difficult on multifragmented fractures. Giles et al. [15] proposed a CT-based correlative technique that predicts the width of the intact glenoid de- rived solely from the glenoid height (glenoid width = 2/3
× glenoid height + 5 mm for men; + 3 mm for women).
They showed that this method can not only reduce radia- tion dose exposed to the patient but also eliminate the need to purchase expensive postprocessing software.
Sugaya et al. [10] introduced on-face three-dimensional (3D) CT method with humeral head subtraction—a reli- able and noninvasive method to detect morphology of the glenoid rim. They calculated the percentage fragment size (%) by dividing the area of the bony fragment by the total area of the inferior glenoid circle. We measured the glenoid height of our patient (Fig. 1D) and calculated the width by substituting the value into the formula devised by Giles et al. [15]. Taking this width, we calculated the
area of the assumed outer-fitting circle and thereby the area of the fracture through the on-face 3D CT method.
According to this calculation based on Sugaya et al.’s method [10], we found that the area encompassed by the fracture was 26.3% of the total glenoid area (Fig. 1E).
But we surmised that our calculated area was an under- estimate of the actual area since the way we defined the area of defect did not overlap entirely with that that was arthroscopically determined to be an area of defect. In addition, we thought that the recurrent dislocation was caused by the bone and cartilage defect.
In sum, we found that our novel arthroscopic approach for displaced anterior glenoid rim fractures is associated
with favorable clinical outcomes at short-term follow-up.
Our novel approach has addressed limitations of preex- isting techniques such as postoperative neurovascular injury and intra-articular problems; therefore, our results showing this support the applicability of this technique as a viable alternative to treat displaced anterior glenoid rim fractures.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
1. van Oostveen DP, Temmerman OP, Burger BJ, van Noort A, Rob- inson M. Glenoid fractures: a review of pathology, classification, treatment and results. Acta Orthop Belg 2014;80:88-98.
2. Maier D, Izadpanah K, Bayer J, et al. Influencing factors and complications in open treatment of acute anterior glenoid rim fractures. Unfallchirurg 2016 Jan 14 [Epub]. http://dx.doi.
org/10.1007/s00113-015-0129-1.
3. Carro LP, Nuñez MP, Llata JI. Arthroscopic-assisted reduction and percutaneous external fixation of a displaced intra-articular gle- noid fracture. Arthroscopy 1999;15:211-4.
4. Porcellini G, Paladini P, Campi F, Paganelli M. Long-term out- come of acute versus chronic bony Bankart lesions managed arthroscopically. Am J Sports Med 2007;35:2067-72.
5. Bauer T, Abadie O, Hardy P. Arthroscopic treatment of glenoid fractures. Arthroscopy 2006;22:569.e1-6.
6. Spiegl UJ, Smith SD, Todd JN, Coatney GA, Wijdicks CA, Millett PJ.
Biomechanical comparison of arthroscopic single- and double- row repair techniques for acute bony bankart lesions. Am J Sports Med 2014;42:1939-46.
7. Marsland D, Ahmed HA. Arthroscopically assisted fixation of glenoid fractures: a cadaver study to show potential applications of percutaneous screw insertion and anatomic risks. J Shoulder Elbow Surg 2011;20:481-90.
8. Scheibel M, Hug K, Gerhardt C, Krueger D. Arthroscopic reduc-
tion and fixation of large solitary and multifragmented anterior glenoid rim fractures. J Shoulder Elbow Surg 2016;25:781-90.
9. Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ. Complica- tions of bioabsorbable suture anchors in the shoulder. Am J Sports Med 2012;40:1424-30.
10. Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am 2003;85:878-84.
11. Yamamoto N, Itoi E, Abe H, et al. Effect of an anterior glenoid de- fect on anterior shoulder stability: a cadaveric study. Am J Sports Med 2009;37:949-54.
12. Nakagawa S, Mizuno N, Hiramatsu K, Tachibana Y, Mae T. Ab- sorption of the bone fragment in shoulders with bony Bankart lesions caused by recurrent anterior dislocations or subluxations:
when does it occur? Am J Sports Med 2013;41:1380-6.
13. Park JY, Lee SJ, Oh SK, Oh K, Noh Y, Suh KT. Glenoid rim frac- ture through anchor points after arthroscopic Bankart repair for shoulder instability. Int Orthop 2015;39:241-8.
14. Barber FA, Herbert MA. Cyclic loading biomechanical analysis of the pullout strengths of rotator cuff and glenoid anchors: 2013 update. Arthroscopy 2013;29:832-44.
15. Giles JW, Owens BD, Athwal GS. Estimating glenoid width for instability-related bone loss: a CT evaluation of an MRI formula.
Am J Sports Med 2015;43:1726-30.