Journal of Korean Spine Surg.
Vol. 6, No. 1, pp 146~150, 1999
Address reprint requests to Ki Ser Kang, M.D.
Department of Orthopaedic Surgery, College of Medicine, Chung-Ang University
# 82-1, Pil-dong-2-ga, Chung-ku, Seoul, 100-272, Korea Tel : 82-2-2260-2163, Fax : 82-2-2271-1710
Intraradicular Lumbosacral Disc Herniation
-A Case Report And Review of the Literature-
Ki-Ser Kang, M.D., Eun-Woo Lee, M.D., Soo-Yong Kang, M.D., Eui-Chan Jang, M.D., Ho-Sung Ryu, M.D., Jong-Sik Suk, M.D.*
Departments of Orthopaedic Surgery and Neurosurgery*, College of Medicine, Chung-Ang University, Seoul, Korea
– Abstract –
Intraradicular disc herniation is a very rare form of disc herniation because the disc should migrate distally and laterally to enter the nerve root sheath. No case has been diagnosed before surgery. We descibe a 72-year-old woman who has an intraradicular disc herniation into the S1 nerve root and summarize the common features of the past reported 12 cases and this one. MRI showed enlarged nerve sleeve simulating root cyst at the S1 body level. At surgery, fusiform swelling of S1 nerve root adhered to anterior structure was seen and root tumor was suspected. Through the incised opening of the root sheath, two pieces of disc fragment were removed and final diagnosis of intraradicular disc herniation was made. Biopsy of extracted frag- ments revealed degenerative collagenous tissue. Patient’s symptom was relieved almost immediately after surgery. An unusual form of intraradicular disc herniation is presented with review of the English language literatures.
Key Words: Disc herniation, Intraradicular, Intervertebral
INTRODUCTION
There have been more than 79 reports of intradural disc herniation since Dandy in 1942 initially described i t5, 11). Intraradicular disc herniation is an unusual form of disc herniation because disc material should migrate its way downward and laterally to invade the nerve root sheath. Barbera in 1984 first reported intraradicu- lar disc herniation2 ). Since then, eight authors reported one of each1, 4, 6, 7, 9, 10, 12, 13) and Jackson added three c a s e s 8 ). We searched the English language literature and found that there were 12 cases reported till 1997.
We present an another patient with intraradicular lumbosacral disc herniation and review the past reported 12 cases in the English language literature.
CASE REPORT
A 72-year-old woman presented with a 14-month history of intermittent low back pain. Two months before her hospitalization, the sciatica which radiated to the buttock and posterior aspect of her right lower limb developed and worsened after exertion and did not subside with conservative treatment.
Neurologic examination on admission elicited Laseque sign at 60°on the right and 90°on the left.
The power of big toe dorsiflexion was normal on both side, but decreased sensation in the right S1 derma- tome and absent right ankle reflex were found.
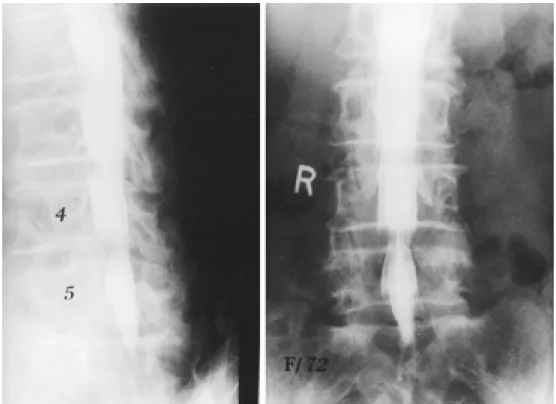
Plain radiographs revealed degenerative bone spur and grade-I spondylolisthesis at L4-5 level. Lumbar myelography on admission showed a right extradural defect at L4-5 with blunting of the right S1 root sleeve(Fig. 1). On clinical examination the patient had
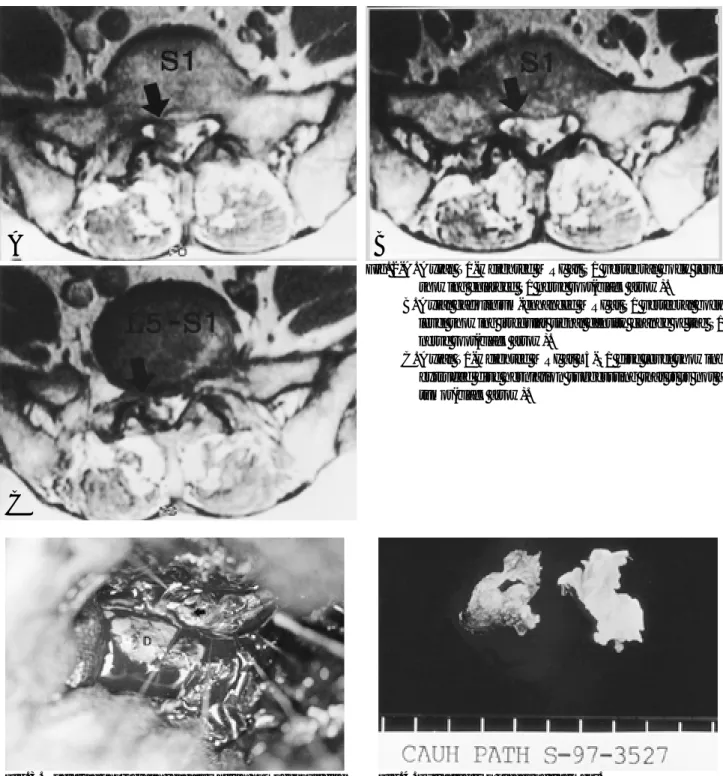
a right S1 radiculopathy. MRI showed enlarged right S1 nerve root on T1 weighted image(Fig. 2a) and irregular signal intensity change in gadolinium enhancement image at S1 vertebral body level sug- gesting scarring or inflammation(Fig. 2b). Also MRI on T1 weighted image at L5-S1 disc level revealed extruded disc herniation which suggested no tumorous condition(Fig. 2c). Radiologist’s impression was ectatic nerve sleeve or root cyst and no other tumorous con- dition was suspected.
At surgery, a right L5-S1 hemilaminectomy was per- formed. A 1.5×2㎝ sized spindle-shaped bulge of S1 nerve root was tightly adhered to the back of S1 verte- bral body and almost impossible to retract. However, the bulge was apparently 8mm distal to the right S1 nerve root. At that time S1 nerve root tumor was suspected and laminectomy was extended to expose the right S1 nerve root completely. Under the surgical microscope, the S1 radicular sheath was opened longitudinally (Fig. 3) and two pieces of fragment which occupied the inside of root sheath were extirpated(Fig. 4) exposing a small opening in the anterior wall of radicular sheath. Operative finding was drawn schematically in Fig. 5. After then, S1 nerve root was freely movable with little tension.
There was no CSF leak.
The longitudinal incision of the root sheath was closed with interrupted stitches and the remainder of the L5-S1 intervertebral disc material was removed.
Posterolateral fusion between L4-L5 was performed for the prevention of instability due to grade-I spondylolisthesis and total laminectomy. The wound was closed in the usual manner. Pathologic finding of intraradicular fragment was reported as degenerative collagenous tissue.
Postoperatively, the patient had complete relief of her radicular pain and paresthesias. Two year follow- ing surgery, she has no complaints.
DISCUSSION
Intradural herniation of the intervertebral disc is a rare condition which was initially described by Dandy in 19425 ). Since that time, more than 79 cases have been reported1 1 ). Intraradicular disc herniation was first reported by Barbera in 19842 ). Since then, 11 addi- tional cases have been reported sporadically as shown in Table 1. Our case might be the thirteenth reported
Fig. 1. Lumbar myelogram of a 72-year-old woman showing incomplete filling defect of the right S1 nerve root sleeve.
in the English language literature.
Clinical data regarding the reported patients of intraradicular disc herniation are summarized in Table 1. The age distribution of intraradicular disc hernia- tion is between 30 and 74 years and averages one or two decades higher than that of the usual disc herni-
ation. 11(84%) of the 13 patients were in male. Radi- cular symptom became worse before admission acute- ly or subacutely in 8 patients(61%) at which time the disc material might invade the nerve root sheath.
Interestingly, S1 nerve root was involved most com- monly in 10(77%) of 13 patients. Straight leg raising test was positive in 10(77%) of 13 patients. All patients(100%) recovered their symptom immediately Fig. 2-A. Axial T1-weighted MRI at S1 vertebral body level
showing enlarged S1 nerve root(black arrow).
Fig. 2-B. Axial gadolinium-enhanced MRI at S1 vertebral body level showing irregular signal density change of the S1 nerve root(black arrow).
Fig. 2-C. Axial T1-weighted MRI at L5-S1 disc level showing extruded disc herniation suggessting that it is not a tumor(black arrow).
Fig. 3. Operative photograph reveals whitish homogenous disc material in the longitudinally opened and retracted S1 nerve root sheath(black arrow). Multiple white shapes are artifacts. D=dura mater of cauda equina.
Fig. 4. Extracted two pieces of fragment.
A B
C
after surgery.
The pathogenesis of intradural or intraradicular disc herniation is not known with certainty. But the
mechanism underlying intraradicular herniation might not be different from those described for intradural herniation, with the exception that the disc material subsequently migrates its way to the nerve root1 0 ). Most commonly suggested etiologic factor of intradural or intraradicular herniation is dense adhesions between the ventral dura or the nerve root sheath and the anterior wall of the spinal canal. The adhesions could be caused by congenital origin, disc protrusion, osteo- phyte, inflammatory process, trauma or previous s u r g e r y 2, 3, 9, 12). Previous surgery was described to be the cause of adhesion in 3(23%) of 13 patients.
However it is unclear whether the adhesions were already present when the herniation occurred or developed later because of irritation from the disc her- niation itself8 ).
In review of reported literature, dense adhesions were present in 11(84%) of 13 patients although there were no comment on the adhesion in 2 patients.
In addition, the diagnosis was made during surgery in all 13 patients(100%). Although myelogram and MRI did not give definite diagnostic clue preoperatively, high index of suspicion is very important for the pre- operative diagnosis of intraradicular disc herniation if we can see the cut-off sign of nerve root in myelo- gram and enlarged swelling of nerve root and associ- ated intervertebral disc herniation in MRI.
Fig. 5. Schematic drawing of intraradicular lumbosacral disc herniation.
Table 1. Reported Cases of Intraradicular Disc Herniation.
Symptom, History of Time of
Series(Ref. No) Age(yr)/Sex Sudden(S) or Location *S.L.R. previous diagnosis,
Adhesion Results
Gradual(G) surgery during
surgery
Barbera, 1984(2) 34/M S S1 + no yes yes excellent
Lesion, 1984(9) 44/M S S1 n.c no yes yes excellent
Açikgöz, 1986(1) 30/M n.c S1 + yes yes n.c excellent
Ergungör, 1987(6) 44/F S S1 + no yes yes excellent
Tsuji, 1991(13) 38/M G S1 + yes yes yes excellent
Nassal, 1995(10) 62/M G L5 + no yes yes excellent
Cusimano, 1995(4) 42/M S L3 n.c no yes n.c excellent
Finkel, 1997(7) 46/M S S1 + yes yes yes good
Jackson, 1997(8) 74/M G L5 - no yes yes excellent
36/M S S1 + no yes yes excellent
53/M S S1 + no yes yes excellent
Süzer, 1997(12) 41/M G S1 + no yes yes excellent
Author 72/F S S1 + no yes yes excellent
* S.L.R = straight leg raising n.c = no comment in the report
herniated disc
S1 root
It is recommended that the diagnosis of intrara-dic- ular disc herniation should be highly suspected during surgery if the enlarged nerve root is tightly adhered to the anterior wall of the spinal canal.
REFERENCES
01) Acikgöz B, zcan OE, Iplikcioglu C and Salglam S : I n t r a r a - dicular disc herniation. Neurosurgery, 19:673-674, 1986.
02) Barbera J, Gonzalez-Darder J and Garcia-Vazquez F : Intraradicular herniated lumbar disc: Case report. J Neuro- surgery, 60:858-860, 1984.
03) Blikra G : Intradural herniated lumbar disc. J Neurosur- gery, 31:676-679, 1969.
04) Cusimano MD, Bukala B and Bilbao J : Extreme lateral disc herniation manifesting as nerve sheath tumor: Case report. J Neurosurgery, 82:654-656, 1995.
05) Dandy WE : Serious complications of ruptured interverte- bral disks. JAMA, 119:474-477, 1942.
06) Ergüngör MF and Kars HZ : Intraradicular herniation of a lumbar disc: A case report. Neurosurgery, 21:909-911, 1987.
07) Finkel HZ : Intraradicular, intervertebral disc herniation.
Spine, 22:1028-1029, 1977.
08) Jackson RP and Kornblatt MD : Report of three cases.
Orthopedics, 20:980-985. 1997.
09) Lesoin F, Duquennoy B, Rousseaux M, Servato R and Jo- min M : Report of three cases with review of the literature.
Neurosurgery, 14:728-731, 1984.
10) Nazzal MM, Croissant PD, Ali A and Kaidi AA : A case report and review of the literature. J Spinal Disord, 8:86- 88, 1995.
11) Reina EG, Calonge ER and Heriot RM : T r a n s d u r a l lumbar disc herniation. Spine, 19:617-619, 1994.
12) Süzer T, Tahta K and Co kun E : Intraradicular lumbar disc herniation.: Case report and review of the literature.
Neuro-surgery, 41:956-959, 1997.
13) Tsuji H, Maruta K and Maeda A : Postoperative intraradi- cular intervertebral disc herniation. Spine, 16:998-1000, 1 9 9 1 .
신경초내 추간판 탈출증 - 증례 보고 1례 및 문헌고찰 -
강기서・이은우・강수용・장의찬・류호성・석종식*
중앙대학교 의과대학 정형외과학교실, 신경외과학교실*
파열된 섬유륜을 통해 수액이 신경초내로 탈출하는 신경초내 추간판 탈출증은 매우 희귀하며, 수술전에 진단하기 어려운 특징을 지닌 질환이다.
본 증례의 경우 수술전 자기 공명 영상에서 우측 제 1 천추 신경근이 반대측에 비해 상당히 팽윤되어 신경초 낭 종과 유사한 소견을 보였으나, 수술시 우측 제 1 천추 신경근이 방추상으로 팽윤되고 전벽에 유착되어있는 소견을 나타내었다. 저자들은 신경초 종양 의심 하에 수술 현미경하에서 신경초막을 수직 절개하고 신경근을 압박하고 있 는 두 개의 종물을 제거하였고 조직 검사상 퇴행성 변성이 있는 추간판 물질로 판명되어 신경초내 추간판 탈출증 을 확진할 수 있었다
환자는 수술 후 증상이 곧 호전되었고 일상 생활로 복귀하는 좋은 결과를 보였기에 문헌 고찰과 함께 보고하는 바이다.
색인단어 : 추간판 탈출증, 신경초내 탈출증, 요추
국 문 초 록
※ 통신저자 : 강 기 서
서울특별시 중구 필동 2가 82-1
중앙대학교 의과대학 필동병원 정형외과학교실 Tel : 82-2-2260-2163, Fax : 82-2-2271-1710