INTRODUCTION
Polyunsaturated fatty acids (PUFAs) have a hydrocarbon chain pos- sessing two or more carbon-carbon double bonds. Essential PUFAs for health are omega-3 (n-3) and omega-6 (n-6), and must be ingested by hu- mans and other animals, since they are not naturally synthesized.1)
The n-3 has a cardio-protective effect and reduces cardiovascular dis- ease (CVD) event.2-5) The American Heart Association (AHA), the American College of Cardiology, and the European Society of Cardiolo- gy have recommended an intake of n-3 fatty acid for the prevention of CVDs.6,7) However, studies have not examined the effects of increased or decreased n-6 levels on CVD clinical endpoints and there is insufficient
Original Article
https://doi.org/10.21215/kjfp.2017.7.4.575 eISSN 2233-9116
Korean J Fam Pract. 2017;7(4):575-580
KJFP
Korean Journal of Family Practice고도불포화지방산의 섭취와 프레밍험 위험도와의 관계:
국민건강영양조사 2013년도 분석을 통한 연구
정석인, 나경민, 주남석*
아주대학교병원 가정의학과
Received July 13, 2016 Revised October 11, 2016 Accepted October 13, 2016
Corresponding author Nam-Seok Joo Tel: +82-31-219-5959, Fax: +82-31-219-5218 E-mail: jchcmc@daum.net
Copyright © 2017 The Korean Academy of Family Medicine
This is an open-access article distributed under the terms of the Creative Commons At- tribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Dietary Polyunsaturated Fatty Acids Intake Is Not Associated with Framingham Risk Score:
Analysis of Korean National Health and Nutrition Examination Survey 2013
Suk-In Jung, Kyung-Min Nah, Nam-Seok Joo*
Department of Family Medicine, Ajou University Hospital, Suwon, Korea
Background: The influence of dietary polyunsaturated fatty acid intake on cardiovascular risk is contested. We explored the relationship of dietary polyunsaturated fatty acid intake with the Framingham risk score (FRS) in Koreans.
Methods: From 8,018 participants in the 2013 Korean National Health and Nutrition Examination Survey, the relevant data of 4,242 participants (1,753 males and 2,489 females) were selected and cross-sectionally analyzed. The FRS was compared by the tertiles of dietary polyunsaturated fatty acids, including daily dietary omega-6 fatty acid intake (n-6), daily dietary omega-3 fatty acid intake (n-3), and the ratio of dietary n-6 and n-3 fatty acid intake (n-6:n-3) after adjustment for relevant variables (age, systolic blood pressure, hypertension, diabetes mellitus, dyslipidemia, myocardial infarction, angina, alcohol consumption, smoking, moderate activity, occupation, waist circumference, body mass index, calorie intake, total cholesterol, and high-density lipoprotein).
Results: Mean age was 44.3 and 46.0 years in males and females, respectively. Dietary n-6 intake in males and females was 11.91 g and 1.89 g, respectively, while dietary n-3 intake in males and females was 8.31 g and 1.42 g, respectively. Mean FRS was 6.6 and 6.1 in males and females, respectively. FRS before adjustment was negatively correlated with dietary n-6 and n-3 intake, but positively correlated with n-6:n-3. However, FRS showed no differences after adjustment.
Conclusion: FRS showed no differences in the comparison according to the tertiles of dietary polyunsaturated fatty acids. This could indicate that dietary polyunsaturated fatty acids were not significantly associated with FRS.
Keywords: Fatty Acids, Polyunsaturated; Fatty Acids, Essential; Cardiovascular Diseases
Suk-In Jung, et al. Dietary PUFAs Is Not Associated with FRS Score
Korean Journal of Family Practice
KJFP
evidence showing the effect of either increased or decreased n-6 intake on CVD risk factors, such as blood lipids and blood pressure, in the Co- chrane review.8) However, the AHA states that n-6 PUFA reduces the risk of coronary heart disease (CHD) relative to lower intakes.9)
The ratio of n-6:n-3 is important. A low ratio is more desirable in re- ducing the risk of many chronic diseases, including CVD.10,11) However, recent studies have not associated n-3 intake with a lower CVD risk.12-14)
The Framingham risk score (FRS) was developed based on data ob- tained from the Framingham Heart Study, and has been used globally to evaluate CVD risk. The FRS is a sex-specific, simple coronary disease prediction algorithm that estimates the 10-year risk of developing CHD using sex, age, total cholesterol (TC), smoking, high-density lipoprotein (HDL), and systolic blood pressure (SBP).15,16) The FRS performs well even in different ethnic groups.17)
In South Korea, as diet has become more westernized, interest has grown in foods that can best aid in disease prevention. Hence, it is im- portant to address the controversy over PUFA consumption. We are in- terested in verifying the efficacy of n-3 and n-6 for CHD prevention in Koreans. To investigate the protective influence of PUFAs on CHD, we explored the relationship of dietary PUFA intake using the FRS on the Korean population after extracting data from Korean National Health and Nutritional Examination Survey (KNHANES).
METHODS
1. Participants
KNHANES is an ongoing surveillance system in the Republic of Ko- rea that assesses the health and nutritional status of Koreans, monitors trends in health risk factors and the prevalence of major chronic diseases, and provides data for the development and evaluation of national health policies and programs. Data from the first year of the sixth KNHANES survey that included dietary n-3 and n-6 PUFAs, age, SBP, TC, HDL, and smoking were used in this cross-sectional analysis. The initial number of participants was 8,018 (3,645 males and 4,373 females). Of these, 4,242 participants (1,753 males and 2,489 females) were evaluated after 2,209 participants were excluded due to age (0 to 19 years and over 80 years) not suitable for FRS analysis, and 1,556 participants were excluded due to missing data. All participants provided written informed consent before the survey.
2. Laboratory, Physical, and Nutritional Assessments Blood samples were collected annually after an 8-hour fast. Each sam- ple was immediately processed, refrigerated, and transported in cold storage to the central testing institute (NeoDin Medical Institute, Seoul, Korea) for analysis within 24 hours. Serum TC and HDL concentration were measured enzymatically using a Hitachi Automatic Analyzer 7600 (Hitachi, Tokyo, Japan). Blood pressure was measured by a nurse, using a Baumanometer Wall Unit 33 (W.A. Baum Co., Inc., Copiague, NY, USA);
three measurements were taken, with the average of the second and third measurements reported. Nutrient intake, including total calorie and PU- FAs, was assessed using a 24-hour dietary recall questionnaire, adminis- tered by a dietician.
3. Lifestyle Questionnaires
Current smokers were defined as those who were currently smoking and had smoked more than five packs of cigarettes throughout their life.
Moderate activity was assessed by a questionnaire and categorized as whether occurring or not. In KNHANES, moderate activity means an increased amount of activity compared to activities of everyday living, or activity that causes some shortness of breath, with the activity per- formed once for at least 30 minutes, five days a week or more. Alcohol consumption assessed by a questionnaire was categorized as cumulative alcohol consumption if consumption was at least once a month annually.
4. Assessment of Cardiovascular Disease Risk
The FRS was used to determine CHD. In the Framingham/ATP III criteria, FRS was calculated using scoring of age, TC, smoking, serum HDL, SBP, and use of hypertension (HTN) medication to estimate the 10-year CHD risk. Because scores are known to differ according to sex, sex-specific analysis was performed.
5. Statistical Analyses
The complex sample analysis used for the KNHANES data weighted all values, and followed statistical guidance from the Korea Centers for Disease Control and Prevention. The participants were divided into male and female groups and stratified into three tertiles, according to the amount of dietary PUFA intake (n-3, n-6, and the n-6:n-3 ratio). General characteristics such as age, body mass index (BMI), waist circumference (WC), TC, HDL, low-density lipoprotein (LDL), triglyceride (TG), di- etary PUFA, SBP, diastolic blood pressure (DBP), HTN, diabetes mellitus
정석인 외. 고도불포화지방산의 섭취와 프레밍험 위험도와의 관계 Korean Journal of Family Practice
KJFP
(DM), myocardial infarction (MI), alcohol consumption, and FRS were evaluated by a descriptive method after data weighting. In this study, pre- vious diagnosis and medical prescription was used to define HTN, dia- betes and dyslipidemia while MI, angina was defined following medical diagnoses. ANOVA was used for the comparison of general characteristics between men and women, and for the characteristics comparison among the dietary uptake tertile groups in the sex. We compared FRS according to the daily dietary uptake tertile group, using the ANCOVA test, after adjust- ment for age, SBP, HTN, DM, dyslipidemia, MI, angina, alcohol consump- tion, smoking, moderate activity, occupation, WC, BMI, calorie intake, TC, and HDL after data weighting. The results represented the adjusted FRS.
P<0.05 was considered significantly statistical different. Data was analyzed using IBM SPSS Statistics for Windows, version 22.0 (IBM Corp., Armonk, NY, USA).
RESULTS
All data were analyzed after data weighting. The mean age was 44.3 years in males and 46.0 years in females. Dietary n-6 intake in males and females were 11.91 g and 1.89 g, respectively, while n-3 was 8.31 g and 1.42 g, respectively. The mean FRS was 6.6 in males and 6.1 in females. The general characteristics of the participants are presented in Table 1.
Age was significantly different in males (P for trend <0.001), while age and SBP were significantly different in females (P for trend <0.001 and
Table 1. General characteristics of male and female subjects Characteristic Male
(n=1,753)
Female
(n=2,489) P-value
Age (y) 44.3 (0.5) 46.0 (0.5) 0.002*
BMI (kg/m2) 24.4 (9.6) 23.3 (10.0) <0.001*
WC (cm) 84.0 (0.3) 77.2 (0.3) <0.001*
TC (mg/dL) 187.1 (1.0) 188.5 (0.9) 0.318
HDL (mg/dL) 48.9 (0.3) 55.6 (0.3) <0.001*
LDL (mg/dL) 112.5 (1.8) 120.3 (2.3) 0.007*
TG (mg/dL) 162.5 (4.0) 112.3(1.9) <0.001*
Calorie intake (kcal) 2,490.5 (32.8) 1,775.1 (18.6) <0.001*
n-3 (g) 1.89 (0.06) 1.42 (0.04) <0.001*
n-6 (g) 11.91 (0.30) 8.31 (0.19) <0.001*
n-6:n-3 8.06 (0.15) 7.95 (0.12) 0.531
SBP (mmHg) 119.1(0.4) 113.7(0.5) <0.001*
DBP (mmHg) 78.2 (0.3) 72.88 (0.3) <0.001*
HTN (%) 14.2 (0.9) 15.1 (0.9) 0.402
DM (%) 6.7 (0.7) 5.9 (0.6) 0.327
Dyslipidemia (%) 5.7 (0.5) 8.7 (0.6) <0.001*
MI, angina (%) 2.1 (0.3) 1.5 (0.2) 0.191
Alcohol consumption (%) 75.4 (1.3) 42.6 (1.2) <0.001* Current smoker (%) 41.8 (1.5) 5.2 (0.6) <0.001* Moderate activity (%) 8.7 (0.9) 4.3 (0.4) <0.001*
FRS 6.55 (0.22) 6.06 (0.25) 0.101
Values are presented as weighted mean (standard error).
BMI, body mass index; WC, waist circumference; TC, total cholesterol; HDL, high density lipoprotein; TG, triglyceride; n-3, daily dietary omega-3 fatty acid intake;
n-6, daily dietary omega-6 fatty acid intake; SBP, systolic blood pressure; HTN, hypertension; DM, diabetes mellitus; MI, myocardial infarction; Alcohol con- sumption, monthly alcohol consumption; FRS, Framingham risk score.
Analysis was performed using ANOVA after date weighting following statistical guidance from the Korea Centers for Disease Control and Prevention.
*P<0.05 was considered significantly statistical different.
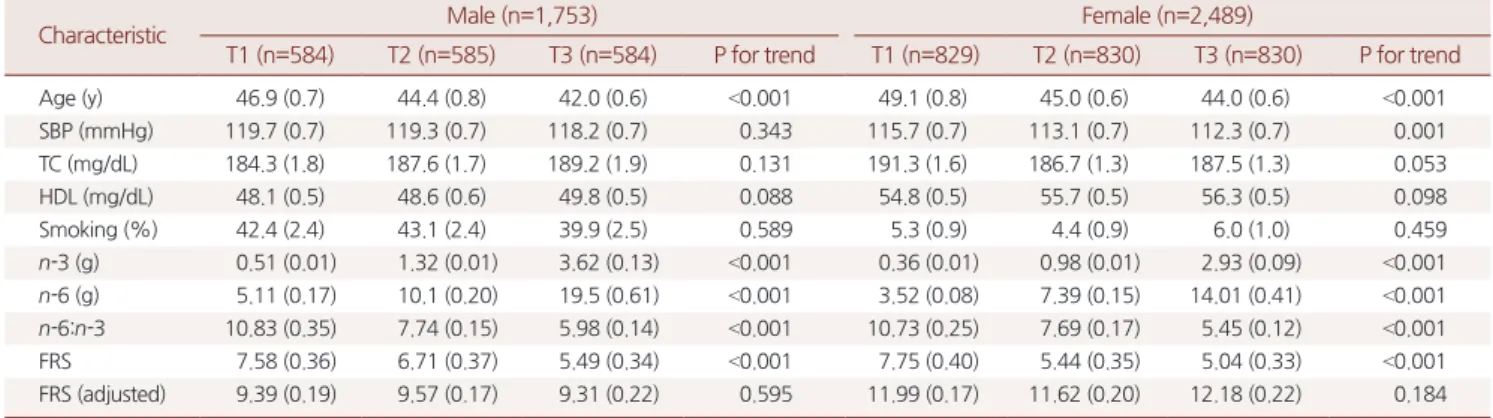
Table 2. General characteristics of subjects by tertile of daily dietary n-3 intake for FRS and correlation of dietary n-3 intake and FRS
Characteristic Male (n=1,753) Female (n=2,489)
T1 (n=584) T2 (n=585) T3 (n=584) P for trend T1 (n=829) T2 (n=830) T3 (n=830) P for trend
Age (y) 46.9 (0.7) 44.4 (0.8) 42.0 (0.6) <0.001 49.1 (0.8) 45.0 (0.6) 44.0 (0.6) <0.001
SBP (mmHg) 119.7 (0.7) 119.3 (0.7) 118.2 (0.7) 0.343 115.7 (0.7) 113.1 (0.7) 112.3 (0.7) 0.001
TC (mg/dL) 184.3 (1.8) 187.6 (1.7) 189.2 (1.9) 0.131 191.3 (1.6) 186.7 (1.3) 187.5 (1.3) 0.053
HDL (mg/dL) 48.1 (0.5) 48.6 (0.6) 49.8 (0.5) 0.088 54.8 (0.5) 55.7 (0.5) 56.3 (0.5) 0.098
Smoking (%) 42.4 (2.4) 43.1 (2.4) 39.9 (2.5) 0.589 5.3 (0.9) 4.4 (0.9) 6.0 (1.0) 0.459
n-3 (g) 0.51 (0.01) 1.32 (0.01) 3.62 (0.13) <0.001 0.36 (0.01) 0.98 (0.01) 2.93 (0.09) <0.001
n-6 (g) 5.11 (0.17) 10.1 (0.20) 19.5 (0.61) <0.001 3.52 (0.08) 7.39 (0.15) 14.01 (0.41) <0.001
n-6:n-3 10.83 (0.35) 7.74 (0.15) 5.98 (0.14) <0.001 10.73 (0.25) 7.69 (0.17) 5.45 (0.12) <0.001
FRS 7.58 (0.36) 6.71 (0.37) 5.49 (0.34) <0.001 7.75 (0.40) 5.44 (0.35) 5.04 (0.33) <0.001
FRS (adjusted) 9.39 (0.19) 9.57 (0.17) 9.31 (0.22) 0.595 11.99 (0.17) 11.62 (0.20) 12.18 (0.22) 0.184
Values are presented as weighted mean (standard error).
SBP, systolic blood pressure; TC, total cholesterol; HDL, high density lipoprotein; smoking, current smoker; n-3, daily dietary omega-3 fatty acid intake; n-6, daily dietary omega-6 fatty acid intake; FRS, Framingham risk score.
FRS (adjusted) was adjusted by age, systolic blood pressure, diastolic blood pressure, hypertension, diabetes mellitus, hyperlipidemia, myocardial infarction, angina, alco- hol consumption, smoking, moderate activity, employment, waist circumference, body mass index, calorie intake, total cholesterol, high-density lipoprotein, low-density lipoprotein, and triglyceride.
Analysis was performed using ANOVA and ANCOVA (for adjusted FRS) after date weighting following statistical guidance from the Korea Centers for Disease Control and Prevention.
Suk-In Jung, et al. Dietary PUFAs Is Not Associated with FRS Score
Korean Journal of Family Practice
KJFP
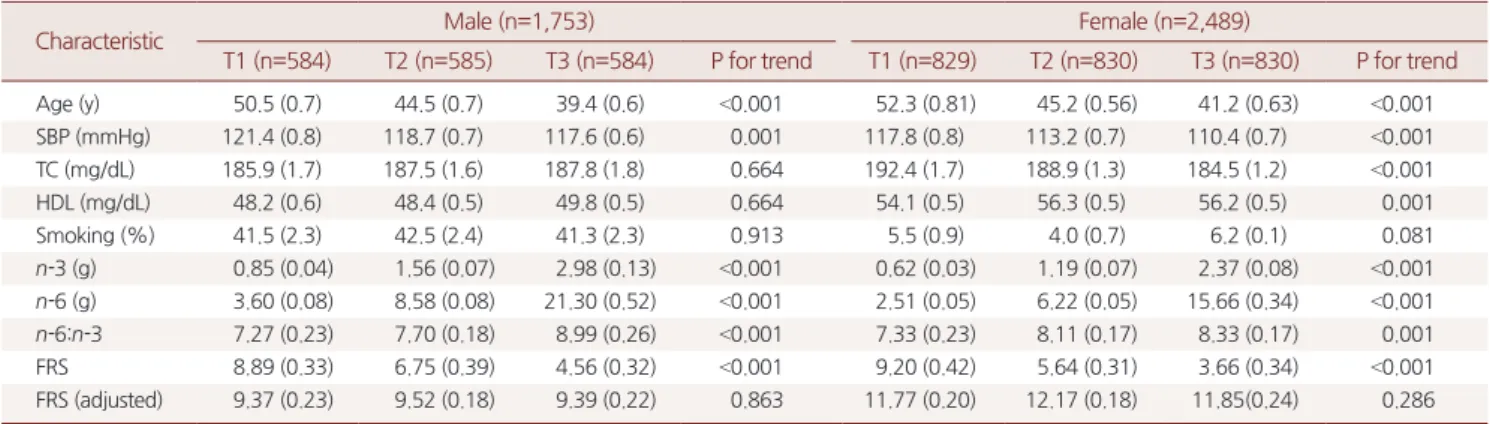
<0.001, respectively) within data required for the calculation of FRS from the n-3 tertile. Significant negative relationships were evident between FRS and tertile group of dietary n-3 PUFA intake in males and females (P for trend <0.001; Table 2). Age and SBP differed significantly for the calculation of the FRS in the n-6 tertile of males and in the n-6:n-3 tertile of both sexes. However, for the n-6 tertile of females, age, SBP, TC, and HDL were significantly different (P for trend <0.01). There were signifi- cant negative relationships between FRS and the n-6 tertile (P for trend
<0.001), but significant positive relationships between FRS and the n-
6:n-3 tertile in both males and females (Tables 3, 4).
After adjustments for age, SBP, DBP, HTN, DM, hyperlipidemia, MI, angina, alcohol consumption, smoking, moderate activity, employment, WC, BMI, caloric intake, TC, HDL, LDL, and TG, there was no signifi- cant relationship between FRS and the n-3, n-6, and n-6:n-3 tertile groups in both sexes (Tables 2–4).
Table 3. General characteristics of subject by tertile of daily dietary n-6 intake for FRS and correlation of dietary n-6 intake and FRS
Characteristic Male (n=1,753) Female (n=2,489)
T1 (n=584) T2 (n=585) T3 (n=584) P for trend T1 (n=829) T2 (n=830) T3 (n=830) P for trend
Age (y) 50.5 (0.7) 44.5 (0.7) 39.4 (0.6) <0.001 52.3 (0.81) 45.2 (0.56) 41.2 (0.63) <0.001
SBP (mmHg) 121.4 (0.8) 118.7 (0.7) 117.6 (0.6) 0.001 117.8 (0.8) 113.2 (0.7) 110.4 (0.7) <0.001
TC (mg/dL) 185.9 (1.7) 187.5 (1.6) 187.8 (1.8) 0.664 192.4 (1.7) 188.9 (1.3) 184.5 (1.2) <0.001
HDL (mg/dL) 48.2 (0.6) 48.4 (0.5) 49.8 (0.5) 0.664 54.1 (0.5) 56.3 (0.5) 56.2 (0.5) 0.001
Smoking (%) 41.5 (2.3) 42.5 (2.4) 41.3 (2.3) 0.913 5.5 (0.9) 4.0 (0.7) 6.2 (0.1) 0.081
n-3 (g) 0.85 (0.04) 1.56 (0.07) 2.98 (0.13) <0.001 0.62 (0.03) 1.19 (0.07) 2.37 (0.08) <0.001
n-6 (g) 3.60 (0.08) 8.58 (0.08) 21.30 (0.52) <0.001 2.51 (0.05) 6.22 (0.05) 15.66 (0.34) <0.001
n-6:n-3 7.27 (0.23) 7.70 (0.18) 8.99 (0.26) <0.001 7.33 (0.23) 8.11 (0.17) 8.33 (0.17) 0.001
FRS 8.89 (0.33) 6.75 (0.39) 4.56 (0.32) <0.001 9.20 (0.42) 5.64 (0.31) 3.66 (0.34) <0.001
FRS (adjusted) 9.37 (0.23) 9.52 (0.18) 9.39 (0.22) 0.863 11.77 (0.20) 12.17 (0.18) 11.85(0.24) 0.286
Values are presented as weighted mean (standard error).
SBP, systolic blood pressure; TC, total cholesterol; HDL, high density lipoprotein; smoking, current smoker; n-3, daily dietary omega-3 fatty acid intake; n-6, daily dietary omega-6 fatty acid intake; FRS, Framingham risk score.
FRS (adjusted) was adjusted by age, systolic blood pressure, diastolic blood pressure, hypertension, diabetes mellitus, hyperlipidemia, myocardial infarction, angina, alco- hol consumption, smoking, moderate activity, employment, waist circumference, body mass index, calorie intake, total cholesterol, high-density lipoprotein, low-density lipoprotein, and triglyceride.
Analysis was performed using ANOVA and ANCOVA (for adjusted FRS) after date weighting following statistical guidance from the Korea Centers for Disease Control and Prevention.
Table 4. General characteristic of subject by tertile of daily dietary n-6:n-3 intake for FRS and correlation of dietary n-6:n-3 intake and FRS
Characteristic Male (n=1,753) Female (n=2,489)
T1 (n=584) T2 (n=585) T3 (n=584) P for trend T1 (n=829) T2 (n=830) T3 (n=830) P for trend
Age (y) 49.7 (0.7) 42.7 (0.8) 41.3 (0.6) <0.001 49.9 (0.6) 44.7 (0.7) 43.6 (0.6) <0.001
SBP (mmHg) 121.1 (0.7) 118.3 (0.7) 118.1 (0.6) <0.001 115.3 (0.8) 113.8 (0.7) 112.0 (0.7) 0.004
TC (mg/dL) 188.3 (1.7) 188.0 (1.8) 185.3 (1.7) 0.403 189.7 (1.4) 187.9 (1.5) 188.0 (1.4) 0.597
HDL (mg/dL) 48.4 (0.6) 48.9 (0.5) 49.1 (0.5) 0.642 54.8 (0.4) 55.9 (0.5) 56.1 (0.5) 0.101
Smoking (%) 38.8 (2.3) 44.0 (2.3) 42.0 (2.4) 0.233 4.1 (0.9) 4.5 (0.9) 7.1 (1.2) 0.109
n-3 (g) 2.73 (0.16) 1.88 (0.07) 1.16 (0.06) <0.001 2.17 (0.11) 1.39 (0.04) 0.75 (0.03) <0.001
n-6 (g) 8.49 (0.39) 13.80 (0.54) 12.99 (0.58) <0.001 6.34 (0.23) 9.98 (0.29) 8.56 (0.35) <0.001 n-6:n-3 3.63 (0.07) 7.31 (0.03) 12.68 (0.28) <0.001 3.49 (0.06) 7.22 (0.32) 12.81 (0.19) <0.001
FRS 8.49 (0.34) 6.02 (0.35) 5.38 (0.33) <0.001 7.82 (0.34) 5.42 (0.37) 5.04 (0.35) <0.001
FRS (adjusted) 9.53 (0.21) 9.18 (0.19) 9.58 (0.16) 0.302 11.93 (0.19) 11.72 (0.19) 12.14 (0.21) 0.372 Values are presented as weighted mean (standard error).
SBP, systolic blood pressure; TC, total cholesterol; HDL, high density lipoprotein; smoking, current smoker; n-3, daily dietary omega-3 fatty acid intake; n-6, daily dietary omega-6 fatty acid intake; FRS, Framingham risk score.
FRS (adjusted) was adjusted by age, systolic blood pressure, diastolic blood pressure, hypertension, diabetes mellitus, hyperlipidemia, myocardial infarction, angina, alco- hol consumption, smoking, moderate activity, employment, waist circumference, body mass index, calorie intake, total cholesterol, high-density lipoprotein, low-density lipoprotein, and triglyceride.
Analysis was performed using ANOVA and ANCOVA (for adjusted FRS) after date weighting following statistical guidance from the Korea Centers for Disease Control and Prevention.
정석인 외. 고도불포화지방산의 섭취와 프레밍험 위험도와의 관계 Korean Journal of Family Practice
KJFP
DISCUSSION
In this cross-sectional analysis, the intake of n-3 and n-6 PUFAs and the n-6:n-3 intake ratio was significantly related to the FRS prior to ad- justment, but not after adjustment, in both sexes.
Both the negative correlation of n-3 and n-6 intake with FRS, and the positive correlation of the n-6:n-3 intake ratio with FRS in both sexes, re- spectively, prior to adjustment was consistent with previous studies that reported on the relationship of PUFAs with CVD, except for n-6. Co- chrane review studies have not examined the effects of either increased or decreased n-6 on CVD risk.8) After adjustments, we did not observe any correlations between PUFA intake and FRS that was consistent with previous studies.8,12-14,18)
Sohn et al.19) performed a cross-sectional study with participants who underwent an annual health examination and voluntarily participated in a dietary modification program conducted at Bundang Seoul National University Health Promotion Center and Iksan Public Health Center in 2012. In this study, the relationship of FRS and PUFAs was analyzed, us- ing the same Framingham/ATP III criteria as Sohn et al.,19) to calculate the FRS. Before adjustment, dietary PUFAs displayed negative relation- ships with FRS, and these were maintained after adjustment for dietary factors and interleukin 6 (IL-6). These differences likely reflect the factors used for correction. To determine the precise relationship between di- etary PUFA and FRS, more than two control variables may be necessary, as in the present study.
The n-3 fatty acids may reduce the risk for CVD through reduced sus- ceptibility of the heart to ventricular arrhythmia and through an anti- thrombogenic effect. The n-3 PUFA has fasting and postprandial hypo- triglyceridemic effects and is mildly hypotensive.2) These effects may slow the growth of atherosclerotic plaque by reducing adhesion molecule ex- pression, reducing platelet-derived growth factors, and promoting an an- ti-inflammatory effect. Considering these mechanisms, intake of n-3 PUFA may aid in the prevention of CVD. In regards to anti-inflammato- ry properties, a study on vascular endothelial cells demonstrated that n-6 fatty acids suppressed all key mediators of the atherosclerotic process20); while higher plasma n-6 was correlated to decreased serum pro-inflam- matory markers, including IL-6 and IL-1 receptor antagonist, and in- creased anti-inflammatory marker, transforming growth factor-beta.21) There is concern that a n-6 enriched fatty acid diet may be more influen- tial than n-3 in the production of 2-series prostaglandins (PG) (such as
PGE2 and PGI2), thromboxane A2, and 4-series leukotrienes (such as leukotriene 4). Because 2- and 4-series PGs have a potent pro-inflamma- tory effect, an n-6 PUFA enriched diet may be more atherogenic. There- fore, the dietary n-6:n-3 ratio is increasingly recognized as being more important than absolute intake.22)
A question arises as to why n-3 PUFA has been effective in the past, given the absence of correlation in recent studies, including the present study. Kromhout et al.23) suggested one possibility. Recent results have been affected by improvement in cardio-protective drug treatment, such as the use of statins. The authors opined that statin use might reduce the beneficial effect of n-3. In our study, 7.8% of participants were taking medication for hyperlipidemia. Because the FRS is calculated using TC and HDL, the results could have been affected by hyperlipidemia treat- ment.
The n-3 PUFA was reported to increase mortality in angina patients than decreasing malignant arrhythmia during regional myocardial isch- emia.14) In heart failure patients, n-3 is elevated in red blood cells and can aid in predicting the risk of ventricular arrhythmias.24) Men diagnosed with angina who are advised to eat oily fish particularly those taking fish oil capsules are reported to have a higher risk of cardiac death.25) PUFAs are typically consumed by eating fish. Men in Eastern Finland, who con- sume a large amount of fish, have an exceptionally high CHD mortality.
Salonen et al.26) explained this was due to the high mercury content in fish. When considering these results, increasing the intake of n-3 PUFA may not necessarily be beneficial in preventing CVDs. Our study results are also consistent with a prior finding that dietary n-3 and n-6 PUFAs are not significantly associated with FRS after adjustment for relevant variables.
There are some limitations in our study. First, this study was cross- sectional and not prospective. Secondly, KNHANES data for one year (2013) were used instead of data from multiple years. Thirdly, dietary n-3 and n-6 PUFAs were assessed using a one-day dietary questionnaire.
Nonetheless, this is the first study to evaluate the association of dietary n-3 and n-6 PUFAs and FRS in Koreans. The results provide preliminary data for more detailed research into the relationship of dietary n-3 and n-6 PUFAs and CV risk factor assessments, such as FRS.
In conclusion, FRS showed no differences in the comparison accord- ing to the tertiles of dietary n-3 and n-6 PUFAs. Dietary PUFAs may not be significant in the association with FRS.
Suk-In Jung, et al. Dietary PUFAs Is Not Associated with FRS Score
Korean Journal of Family Practice
KJFP
REFERENCES
1. Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR. Modern nutrition in health and disease. 11th ed. Philadelphia: Lippincott Williams & Wilkins;
2014. p. 65-87.
2. Kris-Etherton PM, Harris WS, Appel LJ; American Heart Association. Nu- trition Committee. Fish consumption, fish oil, omega-3 fatty acids, and car- diovascular disease. Circulation 2002; 106: 2747-57.
3. Hu FB, Bronner L, Willett WC, Stampfer MJ, Rexrode KM, Albert CM, et al.
Fish and omega-3 fatty acid intake and risk of coronary heart disease in women. JAMA 2002; 287: 1815-21.
4. Marik PE, Varon J. Omega-3 dietary supplements and the risk of cardiovas- cular events: a systematic review. Clin Cardiol 2009; 32: 365-72.
5. Mozaffarian D, Wu JH. Omega-3 fatty acids and cardiovascular disease: ef- fects on risk factors, molecular pathways, and clinical events. J Am Coll Car- diol 2011; 58: 2047-67.
6. Smith SC Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, et al.
AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation 2006; 113: 2363-72.
7. De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dal- longeville J, et al. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J 2003; 24: 1601-10.
8. Al-Khudairy L, Hartley L, Clar C, Flowers N, Hooper L, Rees K. Omega 6 fatty acids for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 2015; (11): CD011094.
9. Harris WS, Mozaffarian D, Rimm E, Kris-Etherton P, Rudel LL, Appel LJ, et al. Omega-6 fatty acids and risk for cardiovascular disease: a science adviso- ry from the American Heart Association Nutrition Subcommittee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Car- diovascular Nursing; and Council on Epidemiology and Prevention. Circu- lation 2009; 119: 902-7.
10. Simopoulos AP. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed Pharmacother 2002; 56: 365-79.
11. Simopoulos AP. Evolutionary aspects of diet, the omega-6/omega-3 ratio and genetic variation: nutritional implications for chronic diseases. Biomed Pharmacother 2006; 60: 502-7.
12. Rizos EC, Ntzani EE, Bika E, Kostapanos MS, Elisaf MS. Association be- tween omega-3 fatty acid supplementation and risk of major cardiovascular disease events: a systematic review and meta-analysis. JAMA 2012; 308:
1024-33.
13. Kwak SM, Myung SK, Lee YJ, Seo HG; Korean Meta-analysis Study Group.
Efficacy of omega-3 fatty acid supplements (eicosapentaenoic acid and docosahexaenoic acid) in the secondary prevention of cardiovascular dis-
ease: a meta-analysis of randomized, double-blind, placebo-controlled trials.
Arch Intern Med 2012; 172: 686-94.
14. Billman GE. The effects of omega-3 polyunsaturated fatty acids on cardiac rhythm: a critical reassessment. Pharmacol Ther 2013; 140: 53-80.
15. Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circu- lation 1998; 97: 1837-47.
16. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cho- lesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evalua- tion, and treatment of high blood cholesterol in adults (Adult treatment panel III). JAMA 2001; 285: 2486-97.
17. D’Agostino RB Sr, Grundy S, Sullivan LM, Wilson P; CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 2001; 286:
180-7.
18. Writing Group for the AREDS2 Research Group, Bonds DE, Harrington M, Worrall BB, Bertoni AG, Eaton CB, et al. Effect of long-chain ω-3 fatty acids and lutein + zeaxanthin supplements on cardiovascular outcomes: results of the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial.
JAMA Intern Med 2014; 174: 763-71.
19. Sohn C, Kim J, Bae W. The framingham risk score, diet, and inflammatory markers in Korean men with metabolic syndrome. Nutr Res Pract 2012; 6:
246-53.
20. De Caterina R, Liao JK, Libby P. Fatty acid modulation of endothelial activa- tion. Am J Clin Nutr 2000; 71(1 Suppl): 213S-23S.
21. Ferrucci L, Cherubini A, Bandinelli S, Bartali B, Corsi A, Lauretani F, et al.
Relationship of plasma polyunsaturated fatty acids to circulating inflamma- tory markers. J Clin Endocrinol Metab 2006; 91: 439-46.
22. Russo GL. Dietary n-6 and n-3 polyunsaturated fatty acids: from biochem- istry to clinical implications in cardiovascular prevention. Biochem Phar- macol 2009; 77: 937-46.
23. Kromhout D, Giltay EJ, Geleijnse JM; Alpha Omega Trial Group. n-3 fatty acids and cardiovascular events after myocardial infarction. N Engl J Med 2010; 363: 2015-26.
24. Wilhelm M, Tobias R, Asskali F, Kraehner R, Kuly S, Klinghammer L, et al.
Red blood cell omega-3 fatty acids and the risk of ventricular arrhythmias in patients with heart failure. Am Heart J 2008; 155: 971-7.
25. Burr ML, Ashfield-Watt PA, Dunstan FD, Fehily AM, Breay P, Ashton T, et al.
Lack of benefit of dietary advice to men with angina: results of a controlled trial. Eur J Clin Nutr 2003; 57: 193-200.
26. Salonen JT, Seppänen K, Nyyssönen K, Korpela H, Kauhanen J, Kantola M, et al. Intake of mercury from fish, lipid peroxidation, and the risk of myocar- dial infarction and coronary, cardiovascular, and any death in eastern Finn- ish men. Circulation 1995; 91: 645-55.