Arthrosc Orthop Sports Med 2017;4(2):81-84 81 Intraosseous ganglion is rarely associated with clinical symptoms because instances of extraosseous extensions are rare;
the periosteum and the cortex of the bone represent a substantial physical barrier for intraosseous extensions of soft tis- sue lesions to intrude into bone. However, we observed a case of a symptomatic intraosseous ganglion located in the ar- ticular capsule of the hip in the inferomedial femoral neck. A 21-year-old woman complained of persistent mild pain and discomfort in the left groin for 18 months. Further, she complained about involuntary movements such as external rota- tion of the hip during full flexion and adduction and inability to kneel down, as well as discomfort during exercise such as yoga. Radiography and computed tomography implied the presence of an intraosseous ganglion in the inferomedial femoral neck. Using an image intensifier, we excised the lesion arthroscopically. The patient’s symptoms resolved imme- diately after surgery. This report describes a case of femoroacetabular impingement caused by an intraosseous ganglion in the femoral neck and evaluates the advantages of arthroscopic procedures for the surgical management of this lesion.
Keywords: Arthroscopy; Bone cysts; Femoroacetabular impingement; Femur neck; Yoga
https://doi.org/10.14517/aosm17006 pISSN 2289-005X·eISSN 2289-0068
Arthroscopic treatment of intraosseous ganglion-induced femoroacetabular impingement in the femoral neck:
a case report
Byung Hoon Lee
1, Yong-Chan Ha
2, Sae Hyun Kang
1, Jin-Kyu Lim
11Department of Orthopedic Surgery, Kangdong Sacred Heart Hospital, Hallym University Medical Center,
2Department of Orthopedic Surgery, Chung-Ang University College of Medicine, Seoul, Korea
Copyright © 2017 Korean Arthroscopy Society and Korean Orthopedic Society for Sports Medicine. All rights reserved.
CC This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/
by-nc/4.0) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received April 26, 2017; Revised June 20, 2017; Accepted June 21, 2017
Correspondence to: Byung Hoon Lee, Department of Orthopedic Surgery, Kangdong Sacred Heart Hospital, Hallym University Medical Center, 150 Seongan-ro, Gangdong-gu, Seoul 05355, Korea. Tel: +82-2-2224-2230, Fax: +82-2-489-4391, E-mail: oselite@naver.com
Case Report
Arthroscopy and Orthopedic Sports Medicine
AOSM
INTRODUCTION
Intraosseous ganglion is a benign cystic lesion that contains a gelatinous material without any epithelial or synovial lining. The intraosseous ganglion, which most often occurs in middle-aged individuals, is thought to be similar to soft tissue ganglia [1,2]. Conservative treat- ment is typically suggested as the first-in-line option for asymptomatic intraosseous ganglia [3]. But we per- formed surgical decompression and excision of the intra- articular lesion because we were presented with a patient with a symptomatic intraosseous ganglion in the femoral neck, which in turn caused femoroacetabular impinge- ment (FAI). We deemed that an arthroscopic intervention would be more advantageous than open capsulotomy because there is less soft tissue injury around the hip but wider visual fields associated with the former [4,5].
This report describes a rare case of an intra-articular and intraosseous ganglion in the inferomedial femoral neck, which we treated arthroscopically using image intensifi- cation.
CASE REPORT
A 21-year-old woman presented with pain, localized to the anterior groin of the left hip. Other predominant symptoms were involuntary movements such as external rotation of the hip during full flexion and adduction and inability to kneel down, as well as discomfort during ex- ercise such as yoga. Physical examination revealed pain- induced restriction in hip motion: internal rotation of less than 10° and flexion of less than 100°. We observed a positive Patrick’s sign and pain during full flexion of the left hip. At admission, the patient’s modified Harris Hip
Byung Hoon Lee, et al. FAI by intraosseous ganglion in the femoral neck
www.e-aosm.org
82
score was 79.
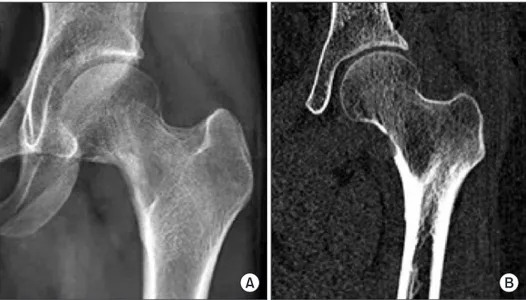
The initial diagnosis of intraosseous ganglion was made on the basis of the anteroposterior pelvic radiograph. The intraosseous ganglion appeared as a well-circumscribed radiolucent lesion that was accompanied by mild sclero- sis (Fig. 1). The computed tomography (CT) scan showed a 0.8-cm-sized circular radiolucent lesion at the infero- medial femoral neck.
To perform hip arthroscopy, the patient was placed under general anesthesia and their hip was distracted by 1.5 cm. Routine arthroscopic examination of the hip was performed using standard anterior, anterolateral, and
posterolateral portals. At the initial arthroscopic exami- nation, we observed no abnormal findings. Under C-arm guidance, we then placed an additional viewing portal di- rectly anterior to the hip joint and facing the inferomedial femoral neck. After ascertaining complete visualization of the lesion through partial capsulotomy under a hip- flexed position, we used an image intensifier to locate and excise the lesion. An electrosurgical instrument was used to approach the lesion through the anterior and anterolateral portals. The diagnosis of the intraosseous ganglion was confirmed by the intraoperative finding of a jelly-like material within the lesion, revealed after burring
A B
Fig. 1. Preoperative pelvic anteropos- terior radiograph (A) and preoperative computed tomography scan (B) reveal an intraosseous ganglion in the infero- medial femoral neck as a well-circum- scribed radiolucent lesion accompanied by marginal sclerosis.
A B
C D
Fig. 2. (A, B) Arthroscopic image of bony protrusions of the overlying cortical bone, which were located with a curved probe under image intensification. (C) Arthroscopic image of a jelly-like ma- terial within the lesion, revealed after burring of the overlying cortical bone.
(D) Arthroscopic image of the ganglion lesion and its adjacent rim removed us- ing a curette and a motorized burr.
Byung Hoon Lee, et al. FAI by intraosseous ganglion in the femoral neck
www.e-aosm.org 83
of the overlying cortical bone (Fig. 2). The lesion and its adjacent rims were removed using a curette and a motor- ized burr. The total distraction time given was 15 minutes for the initial joint examination. There were no postop- erative neurological complications.
The lesion was no longer observed on postoperative CT (Fig. 3). Pain disappeared immediately after the operation and the patient was allowed to tolerate weight bearing as much as they could immediately after the opera- tion. Postoperative complications did not appear by the 2-month follow-up, and the range of motion of the hip was restored to normal. At the last follow-up, the patient had returned to full-time employment and was engaged in recreational activities to pre-injury levels. We found that clinical parameters such as the modified Harris Hip score had also improved with treatment to a score of 95.
DISCUSSION
In this study, we found that intraosseous ganglia in the deep inferomedial femoral neck can be treated with ar- throscopic excision. To the best of our knowledge, there has been no report describing a case of FAI resulting from an intraosseous ganglion in the femoral neck [2,6,7].
Cyst formation in the hip joint is a rare clinical problem.
Sometimes they may be coincidentally detected upon clinical inspection or through imaging examinations, such as ultrasound, CT, and magnetic resonance imag- ing [7]. Ganglion cysts are generally believed to originate from myxomatous degeneration of certain fibrous tissue structures without synovial lining [7]. And intraosseous
ganglia rarely produce clinical symptoms; this is because intraosseous extensions of soft tissue ganglions has to pass through a substantive physical barrier encompass- ing the area between the periosteum and cortical bone to become extraosseous [8]. Intraosseous ganglia located within the articular capsule are also rare and often dif- ficult to detect as these ganglia rarely communicate with the joint cavity [8]. However, an asymptomatic isolated lesion would typically be treated conservatively [3].
As one of the methods of surgical intervention, the Smith-Petersen approach to excision has been used for symptomatic femoral neck lesions [9]. In this study, we demonstrated the advantages of arthroscopic procedures as a surgical treatment option for FAI induced by intraos- seous ganglia in the femoral neck. Arthroscopically, the intra-articular lesion, as well as the bony protrusions and the hyperplastic synovium, could be accurately observed and located with the naked eye. We suggest that if each pathological symptom is treated using a minimally in- vasive arthroscopic procedure, the recovery period and rehabilitation of the patient could be expedited.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
A B
Fig. 3. Postoperative pelvic anteropos- terior radiograph (A) and postoperative computed tomography scan (B) show a completely excised lesion and removed bony protrusions.
Byung Hoon Lee, et al. FAI by intraosseous ganglion in the femoral neck
www.e-aosm.org
84
REFERENCES
1. Feldman F, Johnston A. Intraosseous ganglion. Am J Roentgenol Radium Ther Nucl Med 1973;118:328-43.
2. Sakamoto A, Oda Y, Iwamoto Y. Intraosseous Ganglia: a series of 17 treated cases. Biomed Res Int 2013;2013:462730.
3. FISK GR. Bone concavity caused by a ganglion. J Bone Joint Surg Br 1949;31B:220.
4. Kim SJ, Choi NH, Ko SH, Linton JA, Park HW. Arthroscopic treat- ment of septic arthritis of the hip. Clin Orthop Relat Res 2003;
(407):211-4.
5. Stevens MS, Legay DA, Glazebrook MA, Amirault D. The evidence for hip arthroscopy: grading the current indications. Arthroscopy
2010;26:1370-83.
6. Kambolis C, Bullough PG, Jaffe HI. Ganglionic cystic defects of bone. J Bone Joint Surg Am 1973;55:496-505.
7. Yukata K, Nakai S, Goto T, et al. Cystic lesion around the hip joint.
World J Orthop 2015;6:688-704.
8. Schajowicz F, Clavel Sainz M, Slullitel JA. Juxta-articular bone cysts (intra-osseous ganglia): a clinicopathological study of eighty-eight cases. J Bone Joint Surg Br 1979;61:107-16.
9. Ziegler DN, Scheid DK. A method for location of an osteoid-oste- oma of the femur at operation. A case report. J Bone Joint Surg Am 1992;74:1549-52.