Korean Journal of HBP Surgery □ 증 례 □
Vol. 14, No. 4, December 2010
A Case of Liver Metastasis of Gastrointestinal Stromal Tumor That Was Resected after Treatment with
Imatinib Mesylate and Sunitinib
A 65-year old man underwent wedge resection for a gastrointestinal stromal tumor (GIST) of the gastric fundus in 1997. In 2003, the abdominal CT and sono-guided biopsy revealed he had a large GIST liver metastasis. He underwent treatment with 400 mg/day of imatinib mesylate.
As a result, the liver metastasis markedly decreased in size. However, focal progression of the liver metastasis was observed on the follow up CT, so we increased the imatinib from 400 mg/day to 800 mg/day. We then performed extended left hepatectomy. We report here on a patient who presented with an isolated metastatic GIST to the liver, and the patient was successfully treated with imatinib therapy and hemihepatectomy.
Gum O Jung, M.D.1, Kwon Mook Chae, M.D.1, Dong Eun Park, M.D.1, Hyeok Shim, M.D.2, Sang Hyun Park, M.D.3, Ki Jung Yun, M.D.4
Departments of 1Surgery,
2Hemato-Oncology, 3Radiology and
4Pathology, Wonkwang University Hospital, Wonkwang University College of Medicine
Corresponding Author Kwon Mook Chae
Department of Surgery, Wonkwang University Hospital, Wonkwang University Collage of Medicine, 344-2, Shinyong-dong, Iksan 570-711, Korea Tel: +82-63-859-1490
Fax: +82-63-855-2389
E-mail: chaekm@wonkwang.ac.kr
*This study was performed with the support of funding of wonkwang university in 2008.
Key Words : Gastrointestinal stromal tumors, Imatinib mesylate, Liver metastasis, Liver resection
Received: 2010. 8. 27.
Accepted: 2010. 10. 1.
Introduction
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors of the gastrointestinal tract.
GISTs can metastasize and recur after a long period of remission. Although complete resection is known to be the treatment of choice, less than half of the patients who have recurrent or metastatic GIST can undergo complete resec-
tion. Imatinib is used for the treatment of recurred or metastatic GISTs, and it has been shown to improve patients survival. However, complete responses of GISTs to imatinib are very rare.1 Some authors have recently reported on the role of neoadjuvant treatment with imatinib as cytoreductive therapy, and this can give a patient the opportunity to undergo resection. We report here on a patient who presented with an isolated metastatic GIST to the liver and the patient successfully underwent hemihe-
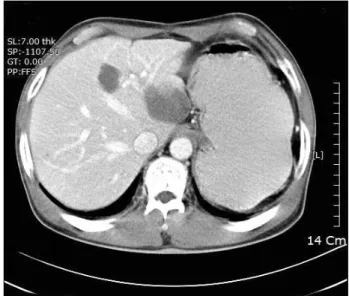
Fig. 1. In April 2003, computerized tomographic scanning of the liver showed a huge inhomogenous mass with multiple daughter masses in segments 7 and 8 and the caudate lobe.
The huge mass in the left lobe ofthe liver was 12.5×9 cm in size and the daughter masses were 1.8×1.0 cm, 2×1.5 cm and 1×1.4 cm, respectively.
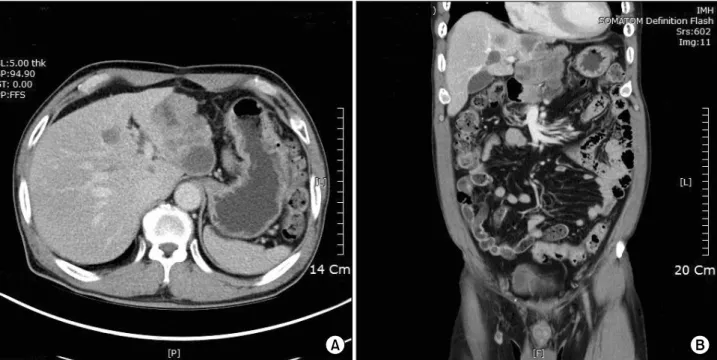
Fig. 2. Imatinib methylate therapy was maintained from April 2003 to March 2005. Follow up CT scanning in 2005 demonstrated that the mass in the left lobe of the liver has decreased in size with respect to the priorstudy and the daughter nodules in segments 7 and 8 showed a complete response on imatinib and so theywere not visible.
patectomy after long term imatinib therapy.
Case Report
A 55 year old man presented to the outpatient depart- ment with melena in July 1999. Esophagogastro-duodeno- scopy (EGD) showed an elevated submucosal mass without ulceration and a bleeding point in the gastric fundus area.
A biopsy was performed though EGD and the pathologic diagnosis of the mass was gastrointerstinal stromal tumor (GIST). Computerized tomography showed a 2 cm sized hypoenhanced solid mass. The patient received gastric wedge resection without lymphadenectomy and the patho- logic result of frozen biopsy showed negative microscopic surgical margins. The pathologic result after the operation revealed a 1.5×2 cm sized, well circumference gastric GIST and its mitotic counter was more than 10 per 50 high power fields (HPFs). Since 1999, he was lost to follow up loss.
In April 2003, he revisited at emergency room presenting with right lower abdominal pain. A CT scan revealed a huge liver mass lesion (Fig. 1) and acute appendicitis. After
appendectomy, ultrasonography guided liver biopsy was performed in order to evaluate the liver mass, and the mass was confirmed as GIST liver metastasis. CT demonstrated a huge mass in the left lobe of the liver and multiple daughter nodules in segments 7 and 8 and the caudate segment. We performed an indocyanin green (ICG-R15) test to evaluate the liver reservoir function, and the result of the ICG R-15 was 38%. We started imanitib mesylate (400 mg/day) due to the unresectable state of the GIST liver metastasis. From August 2003 to March 2005, he received therapy with imatinib mesylate. During imatinib treatment, the GIST liver metastasis showed progressively decreasing size (Fig. 2). We kept treating the patient with imatinib with CT follow up every 6 month. In Feb. 2008, a focal progression of the GITS liver was found on the follow up CT scan, and then we started to administer high dose imatinib (800 mg/day) for 12 month. However, there was still focal progression of disease with a slowly increasing size even though a high dose of imatinib was administered.
We suspected that the tumor had developed resistance to imatinib and so we switched from imatinib to sunitinib.
한국간담췌외과학회지:제14권 4호 2010
Fig. 3. Computerized tomography (A) and (B); the mass in the left lobe of the liver has progressively increased in size with another exophytic mass in the left lateral section. Focally increased enhancement of the contrast media within the mass was also seen.
However, result of sunitinib therapy was not up to our expectations, although there was a decreasing size of lesion (Fig. 3). We decided to perform surgical resection. He received extended left hemihepatectomy with caudate segmentectomy. On the gross findings of the lesion, the masses showed smooth, glistening and multinodular external surfaces, with the dimensions of the largest mass being 10×12 cm (Fig. 4A). In addition, a 1 cm sized mass was found also in the caudate segment of the liver. No gross residual tumor remained in the operation filed. The gross finding of all the tumor in the resected specimen was active lesion in all the tumor territory with little necrosis.
Pathologically, the tumors in the liver were malignant GISTs that consisted of spindle cells and they showed high mitotic features (45/50 HPFs) with strong immunohistochemical positivity for c-kit (Fig. 4B, C). After resection, he dischar- ged without postoperative complication on the 9th posto- perative day.
Discussion
Gastrointestinal stromal tumors (GISTs) were first descri- bed in 1983 as a tumor in the gastrointestinal tract and mesentery. It is the most common mesenchymal neoplasm of the GI tract. Although these tumors can arise anywhere in the gastrointestinal tract, they are most frequently located in the stomach (60%), small bowel (30%) and colorectal area (10∼15%). These tumors have occurred at a median age of 60 years in most series, with a slight male predo- minance.
GISTs are characterized by a specific histological and immunohistochemical pattern. Gain-of-function mutations in the KIT proto-oncogene, which encodes a tyrosine kinase that functions as the receptors for stem cell factor, are present in 85% of GISTs.2 These findings have led to the remarkable development of new molecularly targeted drug therapy with imatinib mesylate (GleevecⓇ), which targets and inhibits the activated KIT tyrosine kinase
Fig. 4. (A) Gross findings of the specimen. Three masses with relatively define margins between the mass and the liver parenchyme were observed on the cut surface. The largest tumor was 9 cm in diameter. (B) The histological feature of the tumor showed mitotic features of more than 10 per 50 high power fields (hematoxylin and eosin staining) (C) Immunohistochemical staining of the tumor showed strong positivity for c-kit.
receptor.3
Though localized GISTs are treated with complete resec- tion, a relatively high incidence of recurrence and metas- tasis has been reported. Further, GISTs can metastasize and recur after a long term remission period. Twenty to 25%
of gastric stromal tumors and 40∼50% of small bowel stromal tumors undergo metastasis, and more than half of THE patients experience tumor recurrence within a median time ranging from 18 to 24 months.4 The most common site for metastasis is the liver and peritoneal cavity, and patients with recurrence have resectable disease in 26 to 30% of the cases.
Surgery as therapeutic strategy is the mainstay of therapy
for patients with GISTs and whose primary lesion is considered to be resectable. DeMatteo and colleagues reported the median survival for patients with primary disease and who underwent complete resection was 66 months compared with 22 months for those who under- went incomplete resection or whose tumor was unresec- table.5 However, surgery in patients with advanced GIST and recurrent or metastatic GISTs is usually not sufficient.
Conventional systemic chemotherapy and radiation therapy have shown an insufficient therapeutic effect.
Imatinib mesylate (GleevecⓇ) is a selective inhibitor of tyrosine kinase, and this is a novel drug for managing GISTs. Rankin et al.6 reported on a phase III trial of
한국간담췌외과학회지:제14권 4호 2010
imatinib mesylate in GISTs and it showed that 45 to 48%
of the patients showed a partial response, 32% showed stable disease, 5% showed complete response and 44 to 53% showed progression free survival for 2 years. The high response rate of advanced and metastatic GISTs to imatinib may give patients the opportunity for complete resection.
The optimal timing of surgery in relation to imatinib therapy for patients with advanced GIST remains to be determined. Resistance to imatinib commonly occurs with prolong use. The median time to progression during primary treatment with imatinib is approximately 2 years and the best tumor response is achieved within a median of 4 months, but optimal responses were still observed at 12 months. Haller and colleagues recently suggested that imatinib-treated patients can be considered for surgery when stagnation of tumor shrinkage is observed.7 Some authors suggest that focal progression signifies the presence of cumulative genetic damage in other seemingly quiescent tumors, and particularly as a result of the prolonged use of imatinib.8 Therefore, a reasonable time to consider surgery is at 12 months after starting imatinib treatment for patients with responsive disease.9 Some authors reported that debulking surgery for focal progressive disease in patients on imatinib resulted in prolonged postoperative progression free survival, if complete resection was performed.10 In this case, the pathologic findings after resection showed viable tumor with small areas of lesion necrosis and high mitotic features. We also experienced that resistance to imatinib occurred with prolonged use.
Since starting imatinib, our case showed a partial response (PR) with a decreasing mass size for 18 month and then “stagnation of tumor shrinkage” was observed for 2 years with imatinib treatment. Focal progression of the lesion was observed during follow-up. The lesion did not show any more response in spite of high dose imatinib, so we decided to perform surgical resection. We report here
on a patient who presented with an isolated metastatic GIST to the liver, and the patient successfully underwent hemihepatectomy after long term imatinib therapy.
References
1. Blanke CD, Demetri GD, von Mehren M, et al. Long-term results from a randomized phase II trial of standard- versus higher-dose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT.
J Clin Oncol 2008;26:620-625.
2. Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors.
Science 1998;279:577-580.
3. Heinrich MC, Griffith DJ, Druker BJ, et al. Inhibition of c-kit receptor tyrosine kinase activity by STI 571, a selective tyrosine kinase inhibitor. Blood 2000;96:925-932.
4. Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differ- ential diagnosis. Arch Pathol Lab Med 2006;130:1466-1478.
5. DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors:
recurrence patterns and prognostic factors for survival. Ann Surg 2000;231:51-58.
6. Rankin C, von Mehren M, Blanke C, et al. Dose effect of imatinib (IM) in patients (pts) with metastatic GIST - a phase III sarcoma group study S0033. Proc Am Soc Clin Oncol 2004;Abstract 9005.
7. Haller F, Detken S, Schulten HJ, et al. Surgical management after neoadjuvant imatinib therapy in gastrointestinal stromal tumours (GISTs) with respect to imatinib resistance caused by secondary KIT mutations. Ann Surg Oncol 2007;14:
526-532.
8. Sym SJ, Ryu MH, Lee JL, et al. Surgical intervention following imatinib treatment in patients with advanced gastrointestinal stromal tumors (GISTs). J Surg Oncol 2008;98:27-33.
9. Bonvalot S, Eldweny H, Péchoux CL, et al. Impact of surgery on advanced gastrointestinal stromal tumors (GIST) in the imatinib era. Ann Surg Oncol 2006;13:1596-1603.
10. DeMatteo RP, Maki RG, Singer S, Gonen M, Brennan MF, Antonescu CR. Results of tyrosine kinase inhibitor therapy followed by surgical resection for metastatic gastrointestinal stromal tumor. Ann Surg 2007;245:347-352.