Yeungnam Univ J Med 2018;35(1):89-93
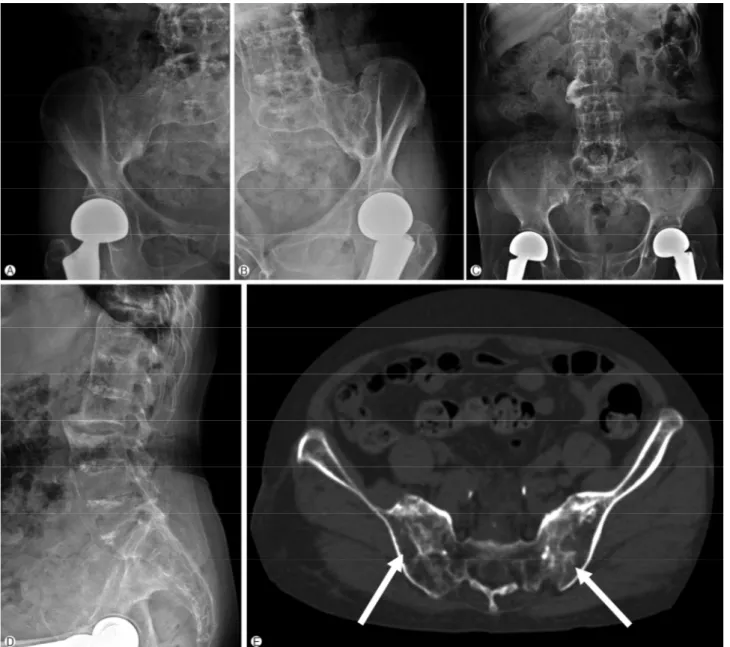
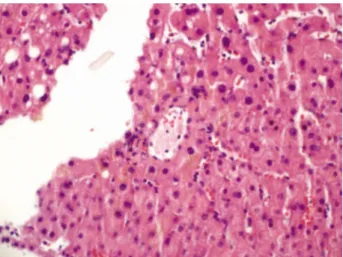
Non-cirrhotic portal hypertension in an ankylosing spondylitis patient
5
0
0
전체 글
(2)
(3)
(4)
(5)
수치
관련 문서
*단어 사이의 공통성과
Think about Secondary Hypertension with any new onset Hypertension or uncontro lled hypertension.. Causes of Resistant Hypertension Improper blood pressure
Channel team management Direct Online enablement Partner Portal Access Deal registration. Webinars
[r]
(Taekwondo, Weight Lifting Players) (90 min × 6 days/week) Warming
[r]
자석 팽이는 볼록한 두 부분에는 고리 자석이 들어 있고, 받침대에는 팽이의 고 리 자석 위치와 일치하는 부분에 삼각형 모양의 자석이 네 개 들어 있다.. 그리고
회원국의 영토밖에서 다른 회원국의 , 영토내에서 회원국의 서비스 소비자에게