접수일:2009년 12월 10일, 승인일:2009년 12월 18일
책임저자:김 경 희 602-715 부산시 서구 동대신동 3가 1번지 동아대학교 의과대학 진단검사의학교실
TEL: 051) 240-2850, FAX: 051) 255-9366, E-mail: progreen@dau.ac.kr 이 논문은 동아대학교 학술연구비 지원에 의하여 연구되었음.
동종조혈모세포이식에 ABO 부적합성이 미치는 영향에 대한 단일 기관 연구
우광숙ㆍ김지은ㆍ김경은ㆍ김정만ㆍ한진영ㆍ김성현1ㆍ김경희
동아대학교 의과대학 진단검사의학교실, 내과학교실1
= Abstract =
Effect of ABO-incompatibility on Allogeneic Hematopoietic Stem Cell Transplantation - A Single Institute Study
Kwang-Sook Woo, Ji-Eun Kim, Kyung-Eun Kim, Jeong-Man Kim, Jin-Yeong Han, Sung-Hyun Kim1, Kyeong-Hee Kim
Departments of Laboratory Medicine and Internal Medicine1, Dong-A University College of Medicine, Busan, Korea
배경: 동종 조혈모세포이식에서 ABO 부적합은 임상적 결과에 영향을 미치지 않는 것으로 알려져 있다.
하지만 ABO 부적합 이식에서 일부 부작용은 보고되고 있어, 한국인 동종 조혈모세포이식에서 ABO 부적 합이 미치는 임상적 영향을 알아보기 위해 생착 여부, 수혈 요구량, 재발율 등의 자료를 조사하였다.
방법: 1999년 8월부터 2009년 5월까지 동아대학교병원에서 ABO 부적합 동종 조혈모세포이식을 받은 20명과 ABO 적합 동종 조혈모세포이식을 받은 29명을 대상으로 하였다.
결과: 부 ABO 부적합 및 양방향 ABO 부적합 동종 조혈모세포이식을 받은 환자군에서 ABO 적합군에 비해 백혈구 생착이 지연되었다(P=0.0079, P=0.0170). 주 ABO 부적합 및 양방향 ABO 부적합 동종 조혈모 세포이식을 받은 환자군에서 ABO 적합군에 비해 적혈구 수혈 요구량도 더 많았다(P=0.0476, P=0.0132).
재발율은 ABO 적합성에 영향을 받지 않았다.
결론: ABO 부적합 동종 조혈모세포이식군에서 백혈구 생착이 지연되고 적혈구 수혈 요구량은 증가하였 으나, ABO 부적합성이 조혈모세포이식의 재발율에는 영향을 미치지 않음을 보여주었다. 하지만 조혈모 세포이식에 있어서 ABO 부적합의 영향은 아직 확실히 규명되지 않은 부분이 있어, 향후 추가적인 연구 가 필요할 것으로 생각된다. (Korean J Blood Transfus 2009;20:235-241)
Key words: ABO-compatibility, HSCT, Engraftment, Transfusion requirements
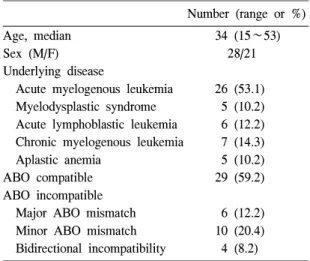
Table 1. Patient characteristics (N=49)
Number (range or %)
Age, median 34 (15∼53)
Sex (M/F) 28/21
Underlying disease
Acute myelogenous leukemia 26 (53.1) Myelodysplastic syndrome 5 (10.2) Acute lymphoblastic leukemia 6 (12.2) Chronic myelogenous leukemia 7 (14.3) Aplastic anemia 5 (10.2)
ABO compatible 29 (59.2)
ABO incompatible
Major ABO mismatch 6 (12.2) Minor ABO mismatch 10 (20.4) Bidirectional incompatibility 4 (8.2)
Introduction
Allogeneic or autologous bone marrow transplan- tation (BMT) or peripheral blood stem cell trans- plantation (PBSCT) have become the treatment of choice for patients with various neoplastic and non-neoplastic disorders.1) In contrast to red blood cell (RBC) transfusion and solid organ transplan- tation, approximately one-third of all allogeneic BMT or PBSCT are performed across the ABO blood group barrier.2,3)
There are three groups of ABO incompatibility:
minor ABO incompatibility (eg from an O-type donor to an A-type recipient), major ABO-incom- patibility (eg from an A-type donor to an O-type recipient) and bidirectional ABO incompatibility (eg A-type donor to a B-type recipient). Most studies indicate that ABO incompatibility has no effect on the clinical outcome after allogeneic hematopoietic stem cell transplantation (allo-HSCT).4,5) However, several complications including increased risks of hemolytic reactions, delayed RBC engraftment, and pure red cell aplasia (PRCA) have been reported in ABO-mismatched transplantation.2,6) In particular, major ABO incompatibility may lead to prolonged destruction of donor-derived RBCs and prolonged transfusion requirements after allo-HSCT.7) For these reasons, clinicians are very interested in determining whether ABO mismatching affects the final outcome of HSCT. Some studies have recently suggested that ABO incompatibility may increase transplant-related morbidity and mortality.7-9)
Up to date, only few studies have systematically addressed the consequences of ABO incompatibility after allo-HSCT in Korea. To explore the effect of
ABO mismatch on clinical characteristics in allo- HSCT, we investigated data on engraftment, trans- fusion requirement and relapse rate according to donor-recipient ABO compatibility.
Materials and Methods
1. Patients
During August, 1999 to May, 2009, we retrospec- tively reviewed the clinical courses of 20 recipients of allo-HSCT from ABO-incompatible donors and 29 from ABO-compatible donors in Dong-a Univer- sity Hospital. ABO-incompatible group consisted of 6 major, 10 minor and 4 bidirectional ABO- incompatible allo-HSCT. In general, bone marrow was used as the stem cell source, while 8 patients (16.3%) received PBSCT. Patient characteristics are summarized in Table 1.
Table 3. Transfusion requirements until Day +100 after transplantation*
ABO compatible
Minor ABO mismatch
Bidirectional ABO mismatch
Major ABO mismatch
N 29 10 4 6
RBC units transfused (mean) 3.2 3.8 12.8† 10.0†
PLT transfusions received (mean) 11.7 14.3 15.0 15.1
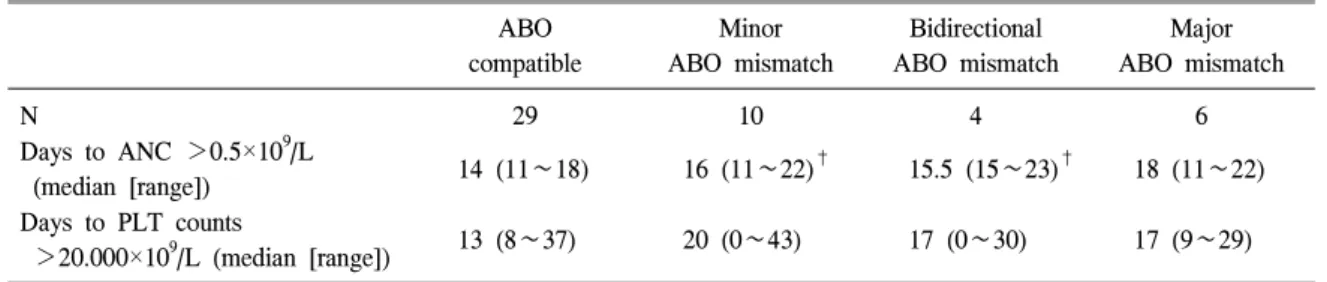
*ABO-incompatible groups were compared to ABO-compatible group, †P<0.05 Table 2. Engraftment according to donor-receptor ABO compatibility*
ABO compatible
Minor ABO mismatch
Bidirectional ABO mismatch
Major ABO mismatch
N 29 10 4 6
Days to ANC >0.5×109/L
(median [range]) 14 (11∼18) 16 (11∼22)† 15.5 (15∼23)† 18 (11∼22) Days to PLT counts
>20.000×109/L (median [range]) 13 (8∼37) 20 (0∼43) 17 (0∼30) 17 (9∼29) Abbreviations: ANC, absolute neutrophil count; PLT, platelet.
*ABO-incompatible groups were compared to ABO-compatible group, †P<0.05.
2. Engraftment and transfusion
Neutrophil engraftment was defined as the first of three consecutive days with an absolute neutrophil count (ANC) of at least 0.5×103/μL. The day of platelet (PLT) engraftment was defined as the first day of 7 consecutive days when an untransfused platelet count exceeded 20×103/μL. The number of transfused PLTs and RBCs were recorded for all patients during 100 days after transplantation.
3. Statistical analysis
Continuous variables in the two groups were compared using Student-t test. Statistical analysis was performed using MediCalc version 9.3 (MedCalc Software, Mariakerke, Belgium). P-value of less than 0.05 was considered as significant.
Results
Hematologic recovery data on engraftment accor- ding to donor-recipient ABO compatibility are shown in Table 2. In ABO minor and bidirectional incompatible group, the time of neutrophil recovery after HSCT was delayed as compared with ABO- compatible group (P=0.0079, P=0.0170 respectively).
Time to PLT engraftment was not different among major, minor, and bidirectional ABO-incompatible group with the ABO compatible group (P>0.05).
1. Transfusion requirements
Table 3 showed transfusion requirements until Day +100 after transplantation. In major and bidirectional ABO-incompatible group, more RBC transfusions were required as compared with
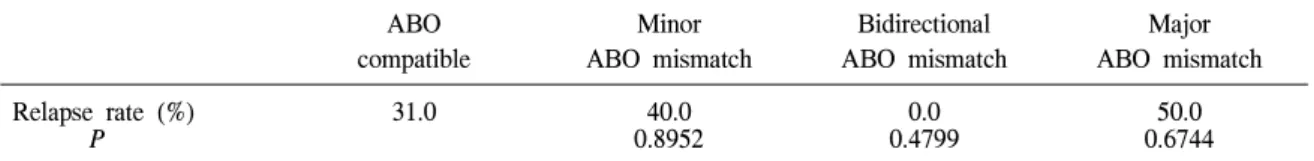
Table 4. Relapse rate according to donor-receptor ABO compatibility*
ABO compatible
Minor ABO mismatch
Bidirectional ABO mismatch
Major ABO mismatch
Relapse rate (%) 31.0 40.0 0.0 50.0
P 0.8952 0.4799 0.6744
*ABO-incompatible groups were compared to ABO-compatible group.
ABO-compatible group (P=0.0476, P=0.0132 re- spectively).
2. Relapsed patients
As shown in Table 1, the majority of patients were malignant diseases. Nine patients of ABO- compatible group and seven patients of ABO- incompatible group relapsed. The relapse rate was not influenced by ABO compatibility (Table 4).
Discussion
Most studies indicate that ABO incompatibility has no effect on the clinical outcome after allo- HSCT although it carries additional risks of hemo- lytic reactions, delayed RBC engraftment.4,5) In contrast, recent reports show conflicting data on the impact of ABO incompatibility for transplant related complications, mortality and survival.7-11) Transfu- sion requirements may also vary among ABO- compatible versus ABO-incompatible HSCTs, which might result in increased iron overload. Iron overload has been shown to be a parameter with a negative impact on transplant-related mortality, late effects, and overall survival (OS).12,13)
In this study, we evaluated data on engraftment, transfusion requirement and relapse rate according to donor-recipient ABO compatibility. The percentage
of major (14%), minor (20%), or bidirectional (8%) donor-recipient ABO incompatibility observed in our study was similar to other reports.6,7,14) As expected, we found that there were no association between ABO-incompatibilty and relapse rate, which was consistent with previous reports. Stussi G, et al reported that the relapse rate was not influenced by ABO compatibility.14) Ozkurt ZN, et al also showed that there were no differences among ABO-compatible versus ABO-incompatible patients in early post- transplantation complication and rejection rates.9) In a study including more than 1,200 ABO-compatible and ABO-incompatible transplants confirmed no adverse association between any ABO incompati- bility and survival.15) However, Stussi G, et al showed an impaired survival after bidirectional ABO-incompatible HSCT.14) Recent studies also showed the adverse effect of ABO incompatibility for transplant related complications, mortality and survival.8,10,11,14,16) A study for Korean patients who had received allogeneic BMT also showed that primary graft failure, rejection, delayed immune hemolytic anemia and persisting erythroid hypo- plasia had developed in ABO-incompatible group.17) In this study, neutrophil engraftment was delayed in minor and bidirectional ABO-incompatible allo- HSCT and PLT engraftment was not influenced by ABO-incompatibility. Delayed neutrophil and/or PLT
engraftment in ABO-incompatible allo-HSCT have also been reported in previous reports.7,9,18-21)
Roz- man P, et al reported that there were no differences between ABO-compatible and ABO- incompatible groups for relapse incidence, risk of graft versus host disease (GVHD) and overall survival. However, in all three cohorts of ABO- incompatible patients, a delayed recovery of neutrophils was recorded as compared to the ABO compatible group, and they hypothesized that immune complexes formed after ABO-incompatible transplantation can cause a pseudo-delay in neutrophil engraftment because immune complexes can be constantly recognized by the Fc receptors on immune cells, including neutrophils, which are subsequently removed from circulation.22) Some authors reported delayed RBC engraftment in ABO-incompatible allo-HSCT.14) Others observed delayed RBC engraftment in major ABO-incompatible allo-HSCT while neutrophil and PLT recoveries were not different.7,14) But we did not evaluate time of RBC engraftment. As expected, more RBC transfusions were required in major ABO-incompatible allo-HSCT in our study which was consistent with past reports.7,9,23) We found that bidrectional ABO-incompatibililty also increased RBC requirement after transplantation.
Small sample sizes, heterogenous disease, various transplant methods, differences for defining success- ful engraftment and various follow-up periods might limit our interpretation. We did not evaluate time of RBC engraftment. As descrived in previous reports, the day of reticulocyte engraftment was defined as the first day when the percentage of reticulocytes in peripheral blood exceeded 1 percent.7,24) Moreover, impact of ABO-incompatibility on overall survival
(OS) and transplant-related complication such as graft-versus-host disease (GVHD) did not evaluated in this study.
In conclusion, our study that ABO-incompatibility has no adverse effect on the relapse rate of HSCT, although neutrophil engraftment was delayed in minor and bidirectional ABO-incompatible allo- HSCT and RBC transfusions were required in major and bidrectional ABO-incompatible allo-HSCT as compared with ABO-compatible group. However, the impact of ABO incompatibility on the conse- quences of the HSCT remains controversial. To explain the association between ABO incompati- bility and the consequences of the HSCT, further studies for impact of ABO-incompatibility on over- all survival and transplant-related complication including graft-versus-host disease and iron overload related increasing RBC requirement are warranted.
Moreover, considering that RBC engraftment pre- ceded myeloid engraftment, further evaluations for RBC engraftment as early indicator of hematopoietic engraftment also will be necessary.
Summary
Background: Most studies have indicated that ABO incompatibility has no effect on clinical outcome after allogeneic hematopoietic stem cell transplan- tation (allo-HSCT). However, several complications have been reported in ABO-mismatched transplan- tation. To explore the effect of ABO mismatch on clinical characteristics in allo-HSCT, we investigated data relating to engraftment, transfusion requirements, and relapse rate according to donor-recipient ABO compatibility.
Methods: From August, 1999 to May, 2009, we retrospectively reviewed the clinical courses of 20 recipients of allo-HSCT from ABO-incompatible donors and 29 from ABO-compatible donors at Dong-a University Hospital.
Results: In the ABO minor and bidirectional incompatible group, the time of neutrophil recovery after HSCT was delayed as compared with the ABO-compatible group (P=0.0079, P=0.0170, re- spectively). In the major and bidirectional ABO- incompatible group, more RBC transfusions were required as compared with the ABO-compatible group (P=0.0476, P=0.0132, respectively). Finally, relapse rates were not influenced by ABO com- patibility.
Conclusion: Requirements of RBC transfusion increased and neutrophil engraftment was delayed in the ABO-incompatible group; however, ABO-incom- patibility had no adverse effect on the relapse rate of HSCT. The impact of ABO incompatibility on the consequences of the HSCT remains controversial and further study is therefore necessary.
References
1. Thomas E, Storb R, Clift RA, Fefer A, Johnson FL, Neiman PE, et al. Bone marrow trans- plantation (first of two parts). N Engl J Med 1975;292:832-43
2. Klumpp TR. Immunohematologic complica- tions of bone marrow transplantation. Bone Marrow Transplant 1991;8:159-70
3. Lasky LC, Warkentin PI, Kersey JH, Ramsay NK, McGlave PB, McCullough J. Hemothe- rapy in patients undergoing blood group incompatible bone marrow transplantation.
Transfusion 1983;23:277-85
4. Bensinger WI, Buckner CD, Thomas ED, Clift RA. ABO-incompatible marrow transplants. Trans- plantation 1982;33:427-9
5. Goldman J, Liesveld J, Nichols D, Heal J, Blumberg N. ABO incompatibility between donor and recipient and clinical outcomes in allogeneic stem cell transplantation. Leuk Res 2003;27:489-91
6. Worel N, Greinix HT, Schneider B, Kurz M, Rabitsch W, Knöbl P, et al. Regeneration of erythropoiesis after related- and unrelated- donor BMT or peripheral blood HPC trans- plantation: a major ABO mismatch means problems. Transfusion 2000;40:543-50
7. Canals C, Muñiz-Díaz E, Martínez C, Martino R, Moreno I, Ramos A, et al. Impact of ABO incompatibility on allogeneic peripheral blood progenitor cell transplantation after reduced intensity conditioning. Transfusion 2004;44:
1603-11
8. Rozman P, Kosir A, Bohinjec M. Is the ABO incompatibility a risk factor in bone marrow transplantation? Transpl Immunol 2005;14:
159-69
9. Ozkurt ZN, Yegin ZA, Yenicesu I, Aki SZ, Yagci M, Sucak GT. Impact of ABO-incom- patible donor on early and late outcome of hematopoietic stem cell transplantation. Trans- plant Proc 2009;41:3851-8
10. Raimondi R, Soli M, Lamparelli T, Bacigalupo A, Arcese W, Belloni M, et al. ABO-incom- patible bone marrow transplantation: a GITMO survey of current practice in Italy and com- parison with the literature. Bone Marrow Transplant 2004;34:321-9
11. Kimura F, Sato K, Kobayashi S, Ikeda T, Sao H, Okamoto S, et al. Impact of ABO-blood group incompatibility on the outcome of recipients of bone marrow transplants from
unrelated donors in the Japan marrow donor program. Haematologica 2008;93:1686-93 12. Majhail NS, Lazarus HM, Burns LJ. Iron
overload in hematopoietic cell transplantation.
Bone Marrow Transplant 2008;41:997-1003 13. Tomás JF, Pinilla I, García-Buey ML, García A,
Figuera A, Gómez-García de Soria VGG, et al.
Long term liver dysfunction after allogeneic bone marrow transplantation: clinical features and course in 61 patients. Bone Marrow Trans- plant 2000;26:649-55
14. Stussi G, Muntwyler J, Passweg JR, Seebach L, Schanz U, Gmür J, et al. Consequences of ABO incompatibility in allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2002;30:87-93
15. Kanda J, Ichinohe T, Matsuo K, Benjamin RJ, Klumpp TR, Rozman P, et al. Impact of ABO mismatching on the outcomes of allogeneic related and unrelated blood and marrow stem cell transplantations for hematologic mali- gnancies: IPD-based meta-analysis of cohort studies. Transfusion 2009;49:624-35
16. Worel N, Kalhs P, Keil F, Prinz E, Moser K, Schulenburg A, et al. ABO mismatch increases transplant-related morbidity and mortality in patients given nonmyeloablative allogeneic HPC transplantation. Transfusion 2003;43:1153-61 17. Lim GT, Kim DW, Jin JY, Lee JW, Han CW,
Min WS, et al. Revisiting anemia after ABO- mismatched allogeneic bone marrow transtan- tation. Korean J Hematol 1991;26:13-21 18. Seebach JD, Stussi G, Passweg JR, Loberiza FR
Jr, Gajewski JL, Keating A, et al. ABO blood group barrier in allogeneic bone marrow transplantation revisited. Biol Blood Marrow
Transplant 2005;11:1006-13
19. Rozman P, Kosir A, Bohinjec M. Is the ABO incompatibility a risk factor in bone marrow transplantation? Transpl Immunol 2005;14:159- 69
20. Helbig G, Stella-Holowiecka B, Wojnar J, Krawczyk M, Krzemien S, Wojciechowska- Sadus M, et al. Pure red-cell aplasia following major bi-directional ABO-incompatible allogeneic stem-cell transplantation: recovery of donor- derived erythropoiesis after long-term treat- ment using different strategies. Ann Hematol 2007;86:677-83
21. Remberger M, Watz E, Ringdén O, Mattsson J, Shanwell A, Wikman A. Major ABO blood group mismatch increases the risk for graft failiure after unrelated donor hematopoetic stem cell transplantation. Biol Blood Marrow Transplant 2007;13:675-82
22. Rozman P, Kosir A, Bohinjec M. Is the ABO incompatibility a risk factor in bone marrow transplantation? Transpl Immunol 2005;14:159- 69
23. Weissinger F, Sandmaier BM, Maloney DG, Bensinger WI, Gooley T, Storb R. Decreased transfusion requirements for patients receiving nonmyeloablative compared with conventional peripheral blood stem cell transplants from HLA-identical siblings. Blood 2001;98:3584-8 24. Mueller RJ, Stussi G, Odermatt B, Halter J,
Schanz U, Seebach JD. Major ABO-incompa- tible hematopoietic stemcell transplantation:
study of post-transplant pure red cell aplasia and endothelial cell chimerism. Xenotrans- plantation 2006;13:126-32