대한혈액학회지 : 제 38 권 제 4 호 2003년
□ 증 례 □
267
Pseudomembranous Gastritis due to Aspergillus in a Patient with Relapsed Acute Myelogenous Leukemia
Sung-Han Kim, M.D.1, Hyun-Jung Kim, M.D.1, Hee-Kyung Kim, M.D.2 Chan-Kyu Kim, M.D.1, Nam-Su Lee, M.D.1, Jin-Tae Jeung, M.D.1 Kyu-Taeg Lee, M.D.1, Sung-Kyu Park, M.D.1, Jong-Ho Won, M.D.1 Dae-Sik Hong, M.D.1, So-Young Jin, M.D.2 and Hee-Sook Park, M.D.1
Departments of Internal Medicine1 and Pathology2, Soon Chun Hyang University College of Medicine, Seoul, Korea
Development of pseudomembranes in the gastrointestinal tract during acute inflammatory or vascular disease has been confined to the small and/or large bowel, with rare occurrences in the esophagus. Primary gut involvement by
Aspergillusis a rare and often fatal complication of intensive antileukemic therapy. To our knowledge, there has been only two case reports of pseudomembranous gastritis. We experienced a case of isolated pseudomembranous gastritis due to
Aspergillusafter chemotherapy for relapsed acute myelogenous leukemia. The diagno- sis was made by gastrofiberscopic findings and histologically.
(Korean J Hematol 2003;38:267
~
269)Key Words : Pseudomembranous gastritis, Aspergillosis
1)
Introduction
There are a few reports of Aspergillus infection of the gastrointestinal tract.1~5) The pathologic findings in these cases include ischemic necrosis and vascular thrombosis with ulcerations1~3) or multiple tumor like masses (as- pergilloma).4) Development of pseudomembranes in the stomach associated with Aspergillus infection is very rare.5,6) Pseudomembranous enterocolitis is a serious, often fatal disease that usually follows antimicrobial ther- apy and Clostridium difficile infection.7) Other reported risk factors include cancer, ischemic colitis, leukemia, severe infection, and neonatal necrotizing enterocoli- tis.6,8)
In this report, we describe our observations in a patient with relapsed acute myelogenous leukemia (AML)
접수 : 2003년 9월 24일, 수정 : 2003년 10월 29일 승인 : 2003년 10월 29일
Correspondence : Jong-Ho Won, M.D. Division of Hematology- Oncology, Department of Internal Medicine, Soon Chun Hyang University College of Medicine
Tel : 02)709-9182, Fax : 02)709-9200 E-mail : jhwon@hosp.sch.ac.kr
who developed a pseudomembranous gastritis due to Aspergillus infection during post-chemotherapy aplastic phase.
Case Report
A 37-year-old female patient was diagnosed as AML- M2 in May 2000. She received remission induction chemotherapy including cytosine arabinoside (Ara-C) and idarubicin, and then acquired complete remission. After 2 cycles of consolidation chemotherapy, she was treated by high dose chemotherapy and autologous peripheral blood stem cell transplantation. Conditioning regimen was consisted of busulfan and cyclophosphamide. The leukemia was relapsed 25 months after transplantation.
She underwent salvage chemotherapy with Ara-C (3g/m2 i.v. every 12 hours, day 1, 3, and 5) and idarubicin (12mg/m2 i.v. day 2 and 4). On day 10 after the start of chemotherapy, fever, severe abdominal pain, diarr- hea, and hematemesis were developed. The white blood cell counts was 100/mm3, hemoglobin 8.5g/dL, and platelet counts 10,000/mm3. Blood cultures drawn on
268
Sung-Han Kim, et al. : Pseudomembranous Gastritis due to Aspergillus in a Patient with Relapsed Acute Myelogenous LeukemiaFig. 2. Endoscopic stomach biopsy sections show an inflammatory pseudomembrane with many bacterial colonies and fungal organisms (A, H & E stain, ×40), and thin, septated, and branching fungal hyphae, consistent with Aspergillus species (B, Grocott methenamine and silver stain, × 1,000).
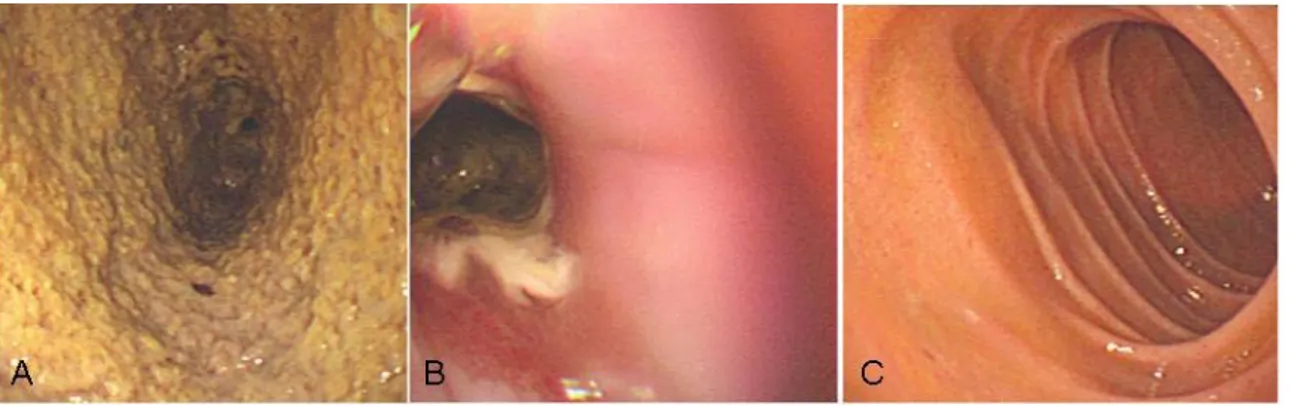
Fig. 1. A) Endoscopic examination of the stomach reveals the mucosa to be covered by thick yellowish exudates forming the pseudomembrane. B, C) Pseudomembrane extends to esophagogastric junction, but esophagus and duodenum are spared.
day 10 grew Aeromonas hydrophila and cefepime Hcl was administered at a dose of 2g twice a day.
Endoscopic examination of the stomach revealed the mucosa to be covered by thick yellowish exudates that formed the pseudomembrane. The pseudomembrane was extended through the total gastric wall but esophagus and duodenum were not involved by pseu- domembrane (Fig. 1). Biopsy of pseudomembrane showed thick septated branching hyphae coexisting Aspergillus species and gram positive cocci with necrotizing tissue (Fig. 2), but tissue culture was not performed. She was treated with intravenous am- photericin B at a dose of 1mg/kg/day. The patient expired due to sepsis on day 21 after the start of chemotherapy.
Discussion
In patients with hematologic malignancies, invasive
fungal infections are mainly produced by Candida and Aspergillus.9) Of these, incidence of the invasive aspergillosis is increased despite of a lot of effort.10) The main localizations are the lung and cranial sinuses;
secondary dissemination to the brain, gut, liver, kid- ney, thyroid, bone, eye, skin, and heart has been re- ported.11) Well-known risk factors for invasive asper- gillosis include prolonged, severe and recurrent neu- tropenia, graft versus host disease, nasal colonization, air pollution from building construction inside or near the hospital, and the absence or pollution of air fil- ters.3,12) Also enteric mucosa damage caused by cyto- toxic drugs could allow Aspergillus to spread into blood vessels.11) Antemortem diagnosis of intestinal fungal invasion is rare because symptoms of abdominal pain and gastrointestinal hemorrhage are not specific, and radiological and echographic studies are not charac- teristic.3)
The first description of pseudomembranous lesions in
대한혈액학회지 : 제 38 권 제 4 호 2003년
269
the stomach was by Yong et al. in 2000.6) The patient was a 36-year-old woman who received bone marrow transplantation and had a graft versus host disease.
Postmortem examination of the stomach revealed the mucosa to be covered by a thick pseudomembrane that contained fibrin, mucus, neutrophils, and fungal hy- phae.
Pseudomembranous colitis has been reported in cases not associated with antibiotic therapy.8) A lot of risk factors identified include intestinal obstruction, colon cancer, leukemia, severe burns, hemolytic-uremic syn- drome, ischemic cardiovascular disease, ischemic coli- tis, neonatal necrotizing enterocolitis, Crohn disease, and Hirschsprung disease. Pseudomembranous colitis have been reported in individuals without identifiable risk factors. Pseudomembrane formation of the stomach has been reported in patients with chronic erosions and hyperchlorhydria of the stomach (diffuse varioliform gastritis).13) Biopsy specimens of the erosions showed volcano-like lesions covered by pseudomembranes.
They concluded that ischemia and increased gastric secretion were responsible for the lesions.
In our case, pseudomembranous changes were associated with an Aspergillus infection. The reason for the isolated gastric lesions without any other organ involvement is unknown. The mucositis induced by cytotoxic chemotherapy, prolonged neutropenia, and gastric hyperchlorhydria might contribute to infection risk.
Our experience may have implications for the risk of the gastrointestinal tract fungal infections in patients received intensive chemotherapy for hematologic ma- lignancies and for early use of amphotericin in the patients who have gastrointestinal symptoms during the neutropenic periods.
요 약
급성 염증 또는 혈관 질환이 있을 경우, 소화관에 위막 (pseudomembrane)의 발현은 소장과 대장, 극히 일부분 에서 식도에 국한된다. Aspergillus 감염에 의해 위막을 형 성하는 일차성 위장관 질환은 극히 드물며 위에 발생한 위 막성 위염 2례가 보고 된 바 있다.
이에 저자들은 재발성 급성골수성백혈병에서 항암화학 요법 후 Aspergillus 감염에 의한 위막성 위염을 보인 1례
를 경험하였기에 문헌고찰과 함께 보고하는 바이다.
References
1) Franciosi CM, Romano F, Caprotti R, Uggeri F : Multiple gastric perforations in an immunode- pressed child. Surgery 131:685-686, 2002
2) Konstantopoulos K, Agapitos E, Komninaka V, Kritsova V, Meletis J, Delaveris E, Loukopoulos D : Acute aspergillosis gastritis in a case of fatal aplastic anemia. Scand J Infect Dis 34:148-149, 2002
3) Catalano L, Picardi M, Anzivino D, Insalobato L, Notoro R, Rotoli B : Small bowel infarction by Aspergillus. Haematologica 82:182-183, 1997 4) Prescott RJ, Haboubi NY, Burton IE : Gastrointe-
stinal tract aspergilloma: possible cause of malab- sorption. J Clin Pathol 47:170-171, 1994
5) Sanders DL, Pfeiffer RB, Hashimoto LA, Subra- mony C, Chen F : Pseudomembranous gastritis : a complication from Aspergillus infection. Am Surg 69:536-538, 2003
6) Yong S, Attal H, Chejfec G : Pseudomembranous gastritis : a novel complication of Aspergillus infection in a patient with bone marrow transplan- tation and graft versus host disease. Arch Pathol Lab Med 124:619-624, 2000
7) Borriello SP : Pathogenesis of Clostridium difficile infection of the gut. J Med Microbiol 33:207-215, 1990
8) Wald A, Mendelow H, Bartlett JG : Nonantibiotic- associated pseudomembranous colitis due to toxin- producing Clostridia. Ann Intern Med 92:798-799, 1980
9) Bodey G, Bueltmann B, Duguid W, Gibbs D, Hanak H, Hotchi M, Mall G, Martino P, Meunier F, Milliken S : Fungal infections in cancer patients: An international autopsy survey. Eur J Clin Microbiol Infect Dis 11:99-109, 1992
10) Cohen J : Clinical Manifestations and management of aspergillosis in the compromised patient. In Warmock DW, Richardson MD, eds. Fungal infec- tion in the compromised patient. 2nd ed. Chiche- ster. John Willy & Sons, 1991, pp117-152
11) Young RC, Bennett JE, Vogel CL, Carbone PP, DeVita VT : Aspergillosis: the spectrum of the disease in 98 patients. Medicine 49:263-265, 1970 12) Uzun O, Anaissie EJ : Antifungal prophylaxis in
patients with hematologic malignancies : a reapprai- sal. Blood 86:2063-2072, 1995
13) Franzin G, Manfrini C, Musola R : Chronic erosions of the stomach: a clinical, endoscopic and histolo- gical evaluation. Endoscopy 6:1-5, 1984