대한소화기학회지 2004;44:19-24
Introduction
1)The meaning and the diagnostic criteria of so called
“obscure gastrointestinal bleeding” is not well defined yet.
It is generally accepted as bleeding of unknown cause that persists or recurs after a negative initial or primary endos-
접수: 2004년 1월 26일, 승인: 2004년 6월 12일 연락처: 김영호, 135-710, 서울시 강남구 일원동 50
삼성서울병원 소화기내과
Tel: (02) 3410-3409, Fax: (02) 3410-3849 E-mail: bowelkim@smc.samsung.co.kr
copic (colonoscopy and/or upper endoscopy) result.12)In case that the cause of gastrointestinal bleeding was confirmed after rebleeding, it can be categorized as obscure gastro- intestinal bleeding. Obscure gastrointestinal bleeding can be classified into two categories; (1) obscure-occult gastrointestinal bleeding which manifest as recurrent or persistent iron
Correspondence to: Young-Ho Kim, M.D., Ph.D.
Department of Medicine, Samsung Medical Center 50 Irwon-dong, Gangnam-gu, Seoul 135-710, Korea Tel: +82-2-3410-3409, Fax: +82-2-3410-3849 E-mail: bowelkim@smc.samsung.co.kr
원인 불명의 위장관 출혈 환자에서 재출혈의 발생률과 예측 인자
성균관대학교 의과대학 내과학교실
김종형·김영호·이선영·정현욱·이준행·손희정·이풍렬·김재준·이종철
Rate and Predictive Factors of Rebleeding with Obscure-Overt Gastrointestinal Bleeding
Jong-Hyung Kim, M.D., Young-Ho Kim, M.D., Sun-Young Lee, M.D., Hyun Wook Jung, M.D., Jun Haeng Lee, M.D., Hee Jung Son, M.D., Poong-Lyul Rhee, M.D.,
Jae J. Kim, M.D., and Jong Chul Rhee, M.D.
Department of Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea
Background/Aims: Little information is available on the rate and predictive factors of rebleeding of unknown cause, which is very important in deciding further investigations on obscure-overt gastrointestinal bleeding. The aim of this study was to evaluate the rebleeding rate and related factors in obscure-overt gastrointestinal bleeding patients who revealed normal gastroscopic and colonoscopic findings. Methods: A total of 69 patients with negative first-line gastroscopy and colonoscopy were enrolled in this study as obscure-overt gastrointestinal bleeding cases. The relationships between rebleeding and clinical characteristics were analyzed retrospectively.
Results: The causes of obscure-overt gastrointestinal bleeding were confirmed in 30 cases among the 69 cases.
Small bowel tumors (14 cases) were the most common cause, followed by vascular lesions (6 cases). The mean follow-up period was 28 months and rebleeding was noticed in 19 patients (27.5%). Among these rebleeding patients, 14 cases (73.7%) occurred within 6 months. The past experience of previous bleeding was significantly related with rebleeding (p=0.0009). Conclusions: Close observation and detailed investigations are needed for obscure-overt gastrointestinal bleeding patients with bleeding history, especially during 6 months follow-up.
(Korean J Gastroenterol 2004;44:19-24)
Key Words: Gastrointestinal bleeding; Recurrence; Risk factors; Causes
대한소화기학회지: 제44권 제1호, 2004
deficiency anemia or fecal occult blood test positivity, (2) obscure-overt gastrointestinal bleeding which manifest as repeated visible bleeding. Obscure-overt gastrointestinal bleeding is common, but its rate and predictive factors are not known well. This is very important in clinical fields since most of the additional tests are expensive and quite valueless in patients with negative gastrointestinal endos- copic findings.
First-line gastroscopic and colonoscopic findings are reported to be normal in some patients with overt gastrointestinal bleeding. However, there are few reports about rebleeding rate and predictive factors of rebleeding, which are very important to decide whether we should perform further investigations. The aim of this retrospective study was to evaluate the rebleeding rate and related factors with rebleeding in obscure-overt gastrointestinal bleeding patients who revealed normal gastroscopic and colonoscopic findings.
Materials and Methods
1. Patients
We reviewed the patients who were admitted to Samsung Medical Center from 1996 to 2002 because of visible gastrointestinal bleeding such as hematochezia or melena.
One hundred thirty-three patients who revealed negative in first-line gastroscopic and colonoscopic findings were retrieved among these patients. Forty-three patients with doubtful bleeding cause such as ulceration without definite evidence of recent bleeding and mild degree of hemorrhoid were excluded from the study. Twenty-one patients who were not available for follow-up were also excluded. Finally, 69 patients with obscure-overt gastrointestinal bleeding were involved in the study. Age, gender, initial hemoglobin level, underlying disease such as hypertension and cerebrovascular disease, medications such as aspirin and NSAIDs, past history of bleeding and the number of episodes were investigated.
2. Diagnostic investigations
After a negative first-line gastroscopy and colonoscopy, patients underwent evaluation for obscure-overt gastrointestinal bleeding by means of repeated endoscopy, small bowel series or enteroclysis, nuclear scan, angiography, computed tomography and/or intraoperative enteroscopy.
3. Follow-up for rebleeding
If the cause of bleeding was unclear even after further investigations, the patients were discharged and followed up in outpatient department for the possibility of rebleeding during mean period of 28 months. If there was an evidence of rebleeding, the source of rebleeding was investigated by additional methods as described above. The relationship between rebleeding and baseline characteristics such as age, gender, initial hemoglobin level, amount of transfusion, underlying disease, medications, past history of bleeding were analyzed.
4. Statistics
Data were analyzed by using Fisher's examination, Mann- Whitney test, and multiple logistic regression test. P-value less than 0.05 was considered statistically significant.
Results
1. Basal characteristics of the patients
The mean follow up period was 28 (3~76) months. The clinical data of 69 patients are summarized in table 1. The patients were composed of 44 males and 25 females with the mean age of 56.3 (17~88) year-old.
2. Findings of diagnostic investigations
The source of bleeding was documented only in 18 cases by additional studies during the first admission, and 12 cases were diagnosed by further evaluation after rebleeding.
Positive findings related with bleeding sources were found in 13 patients (26.5%) of 49 patients received small bowel radiography, 4 patients (21.1%) of 19 patients received radionuclide bleeding scan, 7 patients (41.2%) of 17 patients received mesenteric angiography, 12 patients (25.0%) of 48 patients received computed tomography, and both patients (100%) received intraoperative enteroscopy.
3. Source of obscure-overt gastrointestinal bleeding
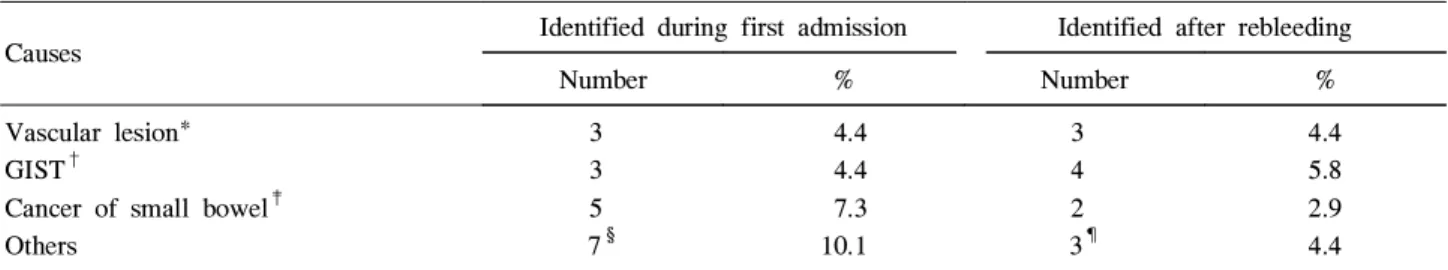
The source of obscure-overt gastrointestinal bleeding was documented in 30 cases among 69 cases. The most common cause was small bowel tumors (14 cases) and the second most common cause was vascular lesions (6 cases) (Table 2).
20
김종형 외 8인. 원인 불명의 위장관 출혈 환자에서 재출혈의 발생률과 예측 인자
4. Rebleeding
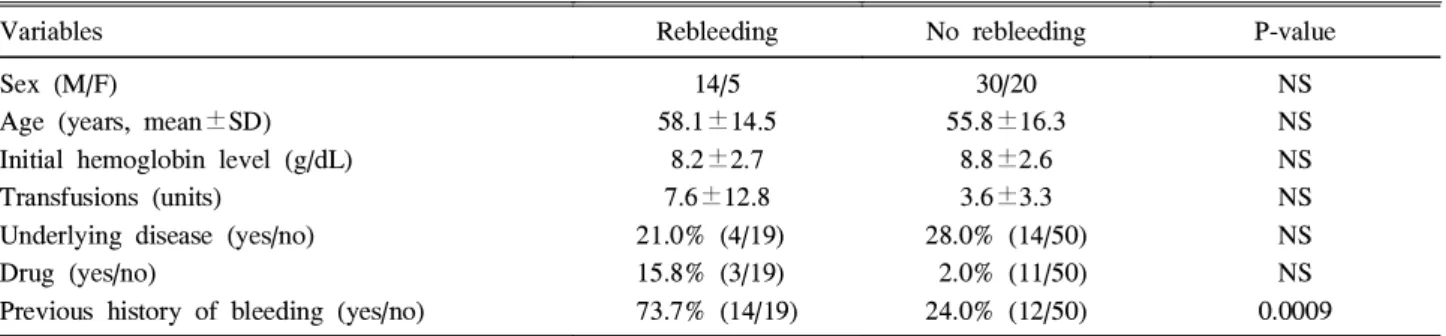
Recurrence of bleeding was noticed in 19 patients (27.5%), and among them, 14 cases (73.7%) occurred within 6 months (Fig. 1). The past experience of previous bleeding was significantly related with rebleeding (p=0.0009).
Although there was no significant difference, the number of previous bleeding episodes was higher in the patients with
rebleeding than in the patients without rebleeding (2.6±1.4 and 1.7±0.9, respectively). Other clinical factors could not predict rebleeding (Table 3).
Discussion
In the present study, we analyzed only the obscure-overt bleeding cases which manifested as repeated visible bleeding, not the obscure-occult gastrointestinal bleeding cases which manifested as recurrent or persistent iron deficiency anemia or fecal occult blood test positivity.
There are several methods available for obscure-overt gastrointestinal bleeding patients who revealed negative in first-line gastroscopy and colonoscopy. The efficacy of small bowel series is less than 10% in obscure gastrointestinal bleeding patients,2 and the yield of positive studies is about 10% in small bowel enteroclysis despite of considerable radiation exposure and discomforts.3,4 The diagnostic yield of push enteroscopy in obscure gastrointestinal bleeding is variable from 24% to 75%.5-7 This is also a complicated method and the entire small bowel cannot be examined.
Sonde enteroscopy which permits direct endoscopic visualization of small bowel by using a thin endoscope propelled through the small bowel by peristalsis, also has a similar clinical yield.8,9 However, when compared to push enteroscopy, Sonde enteroscopy is not widely used due to following limitations. First, the therapeutic endoscopy is not available. Second, longer procedure time is needed. Third, patients complain of severe discomfort during the study.
Although intraoperative enteroscopy is known to identify specific mucosal abnormalities in 70~100% of the cases,10-15 these results are confined to severe gastrointestinal bleeding cases that require repeated transfusions. In addition, general anesthesia is always needed in intraoperative enteroscopy.
Table 2. Causes of Obscure-Overt Gastrointestinal Bleeding
Causes Identified during first admission Identified after rebleeding
Number % Number %
Vascular lesion*
GIST†
Cancer of small bowel‡ Others
3 3 5 7§
4.4 4.4 7.3 10.1
3 4 2 3¶
4.4 5.8 2.9 4.4
*Angiodysplasia or arteriovenous malformation; †GIST, gastrointestinal stromal tumor; ‡Duodenal cancer or other small bowel cancer; §Crohn's disease, intestinal tuberculosis, small bowel ulcer, ischemic colitis, pancreatic cancer, portal vein thrombosis, and vitamin K deficiency; ¶Gastric ulcer or gastric cancer (2 cases).
Table 1. Basal Characteristics of the Patients
Variables No. of cases (%)
or mean values Sex
Male Female
44 cases (63.7%) 25 cases (36.3%) Age (mean±SD)
Male Female
57.6±5.8 54.1±15.6 Type of bleeding
Melena Hematochezia
Melena+Hematochezia
42 cases (60.9%) 17 cases (24.6%) 10 cases (14.5%) Hypertension or CVA 18 cases (26.1%) Aspirin or NSAIDs 14 cases (20.3%) Previous history of bleeding
Number of patients Number of episodes
26 cases (37.7%) 2.2 times (1~5 times) Initial hemoglobin level 8.6 g/dL (3.0~16.1 g/dL) Amount of transfusion 4.7 units (0~54 units) Follow-up period 28.0 months (3~76 months) Period to rebleeding 7.2 months (1~37 months) CVA, cerebrovascular accident; NSAIDs, non-steroidal anti- inflammatory drugs.
21
The Korean Journal of Gastroenterology: Vol. 44, No. 1, 2004
Recently, capsule endoscopy is introduced as a new, wireless, endoscopic examination of the small intestine,16 and diagnostic accuracy of this method is reported to be higher than previous methods.17 However, capsule endoscopy is expensive and large scaled studies are not reported yet.
The diagnostic accuracy of angiography which is an invasive study, depends on bleeding situation of the patient.
Therefore it is often considered valuable only when the patient is actively bleeding.18Tagged red blood cell (TRBC) scan, a kind of radionuclear scan, also depends on bleeding situation of the patient. False localizations appear too high to routinely accept a positive TRBC scan for definite localization of the bleeding site. It has been recommended that further combined investigations are needed with TRBC scan hence surgical resection should not be based solely on TRBC scan results.19
As described above, most of the studies are incomplete and have a lot of limitations. Therefore, to perform these investigations more effectively in obscure-overt gastrointestinal bleeding patients, we must consider the rate and predictive factors of rebleeding along with clinical situation. However, such parameters have been rarely reported. Rebleeding rate was reported to be 30% during a mean 19 month follow-up
after intraoperative enteroscopy in patients with obscure gastrointestinal bleeding. On the other hand, rebleeding occurred in 3 patients (75%) among 4 patients who revealed negative in intraoperative enteroscopy.20In a study, recurrent bleeding occured in one-third of patients who underwent push enteroscopy because of obscure gastrointestinal bleeding.21 Even though it was not statistically significant, they reported that there is a trend toward frequent rebleeding in patients with arteriovenous malformations, past history of frequent bleeding, and higher requirement of transfusion.
Besides, there was no significant difference between overt and occult bleeding in their study. Longstreth has reported that during 34 months follow-up, only 1 patient rebleeded among 26 lower gastrointestinal hemorrhage patients with uncertain cause.22 However, this study is composed of a population-based data on the epidemiology, and the recurrence rate of hemorrhage was 25% at 4 years in 83 patients who diagnosed as diverticulosis.
In this study, most common cause of obscure-overt gastrointestinal bleeding was small bowel tumors. Compared with previous studies,1,2,23 the incidence of small bowel tumors was higher. Probably, the reason for that was limitation of retrospective study.
Fig. 1. Cumulative rate of rebleeding.
Table 3. Predictive Factors of Rebleeding
Variables Rebleeding No rebleeding P-value
Sex (M/F)
Age (years, mean±SD) Initial hemoglobin level (g/dL) Transfusions (units)
Underlying disease (yes/no) Drug (yes/no)
Previous history of bleeding (yes/no)
14/5 58.1±14.5
8.2±2.7 7.6±12.8 21.0% (4/19) 15.8% (3/19) 73.7% (14/19)
30/20 55.8±16.3
8.8±2.6 3.6±3.3 28.0% (14/50)
2.0% (11/50) 24.0% (12/50)
NS NS NS NS NS NS 0.0009 NS, not significant.
22
Kim JH, et al. Rate and Predictive Factors of Rebleeding with Obscure-Overt Gastrointestinal Bleeding
In conclusion, we tried to confine the rebleeding rate and predictive factors related with rebleeding in obscure gastrointestinal bleeding patients who visited because of hematochezia or melena but revealed normal in first-line gastroscopy and colonoscopy. The rebleeding rate was 27.5% in this study and closely related with previous bleeding history. Therefore, we must be careful and perform more detail investigations in patients with previous bleeding history. Moreover, close observation is needed especially during 6 months follow-up since the majority of rebleeding occurred within this period.
요 약
목적: 위장관 출혈로 내원하여 시행한 상부위장관내 시경과 대장내시경검사에서 출혈 원인을 찾지 못하는 경 우를 종종 경험하는데, 아직 이들 환자에 대한 임상적 고 찰은 거의 보고된 바가 없다. 이에 저자들은 위장관 출혈 로 내원한 환자들 중 상부위장관내시경과 대장내시경검 사에서 출혈 원인을 찾지 못한 환자들의 재출혈률 및 위 험인자를 알아보고자 하였다. 대상 및 방법: 육안으로 확인할 수 있는 위장관 출혈을 주소로 내원한 환자들 중 상부위장관내시경과 대장내시경검사에서 원인을 찾지 못한 환자 69명을 대상으로, 후향적 분석을 통하여 재출 혈률과 재출혈 예측 인자에 대하여 조사하였다. 결과:
상부위장관내시경과 대장내시경검사에서 원인을 찾지 못한 위장관 출혈 환자 69명 중 추가 검사를 통하여 원 인이 밝혀진 경우는 30명이었다. 출혈 원인 중 소장 종양 이 14예로 가장 많았고 혈관성 병변이 6예였다. 평균 추 적관찰 기간은 28개월이었으며 재출혈은 19명(27.5%)에 서 발생하였다. 재출혈 환자들 중 14명(73.7%)이 6개월 이내에 발생하였다. 재출혈은 과거 출혈의 병력과 유의 한 상관관계가 있었다(p=0.0009). 결론: 상부위장관내시 경과 대장내시경검사에서 원인을 찾지 못한 위장관 출혈 환자에서 6개월 이내에 출혈의 과거력이 있는 경우 원인 을 찾기 위한 적극적인 노력과 주의 깊은 추적관찰이 요 구된다.
색인단어: 위장관 출혈, 재발, 위험 인자, 출혈 원인
REFERENCES
1. Zuckerman GR, Prakash C, Askin MP, Lewis BS. AGA technical review on the evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology
2000;118:201-221.
2. Van Gossum A. Obscure digestive bleeding. Best Pract Res Clin Gastroenterol 2001;15:155-174.
3. Rex DK, Lappas JC, Maglinte DD, Malczewski MC, Kopecky KA, Cockerill EM. Enterocolysis in the evaluation of suspected small intestinal bleeding. Gastroenterology 1989;97:58-60.
4. Antes G, Neher M, Hiemeyer V, Burger A. Gastrointestinal bleeding of obscure origin: role of enteroclysis. Eur Radiol 1996;6:851-854.
5. Landi B, Tkoub M, Gaudric M, et al. Diagnostic yield of push-type enteroscopy in relation to indication. Gut 1998;
42:421-425.
6. Chak A, Koehler MK, Sundaram SN, Cooper GS, Canto MI, Sivak MV Jr. Diagnostic and therapeutic impact of push enteroscopy: analysis of factors associated with positive findings. Gastrointest Endosc 1998;47:18-22.
7. Zaman A, Katon RM. Push enteroscopy for obscure gastrointestinal bleeding yields a high incidence of proximal lesions within reach of a standard endoscope. Gastrointest Endosc 1998;47:372-376.
8. Berner JS, Mauer K, Lewis BS. Push and Sonde enteroscopy for the diagnosis of obscure gastrointestinal bleeding. Am J Gastroenterol 1994;89:2139-2142.
9. Morris AJ, Wasson LA, MacKenzie JF. Small bowel enteroscopy in undiagnosed gastrointestinal blood loss. Gut 1992;33:887-889.
10. Ress AM, Benacci JC, Sarr MG. Efficacy of intraoperative enteroscopy in diagnosis and prevention of recurrent, occult gastrointestinal bleeding. Am J Surg 1992;163:94-99.
11. Whelan RL, Buls JC, Goldberg SM, Rothenberger DA.
Intra-operative endoscopy. University of Minnesota experience.
Am Surg 1989;55:281-286.
12. Lopez MJ, Cooley JS, Petros JG, Sullivan JG, Cave DR.
Complete intraoperative small-bowel endoscopy in the evaluation of occult gastrointestinal bleeding using the Sonde enteroscope. Arch Surg 1996;131:272-277.
13. Flickinger EG, Stanforth AC, Sinar DR, MacDonald KG, Lannin DR, Gibson JH. Intraoperative video panendoscopy for diagnosing sites of chronic intestinal bleeding. Am J Surg 1989;157:137-144.
14. Desa LA, Ohri SK, Hutton KAR, Lee H, Spencer J. Role of intraoperative enteroscopy in obscure gastrointestinal bleeding of small bowel origin. Br J Surg 1991;78:192-195.
15. Lau WY. Intraoperative enteroscopy - indications and limit- ations. Gastrointest Endosc 1990;36:268-271.
16. Lewis B, Goldfarb N. Review article: the advent of capsule 23
대한소화기학회지: 제44권 제1호, 2004
endoscopy a not-so-futuristic approach to obscure gastro- intestinal bleeding. Aliment Pharmacol Ther 2003;17:
1085-1096.
17. Mylonaki M, Fritscher-Ravens A, Swain P. Wireless capsule endoscopy: a comparison with push enteroscopy in patients with gastroscopy and colonoscopy negative gastro- intestinal bleeding. Gut 2003;52:1122-1126.
18. Rollins ES, Picus D, Hicks ME, Darcy MD, Bower BL, Kleinhoffer MA. Angiography is useful in detecting the source of chronic gastrointestinal bleeding of obscure origin. AJR Am J Roentgenol 1991;156:385-388.
19. Zuckerman GR, Prakash C. Acute lower intestinal bleeding:
part 1: clinical presentation and diagnosis. Gastrointest Endosc 1998;48:606-617.
20. Douard R, Wind P, Panis Y, et al. Intraoperative enteroscopy for diagnosis and management of unexplained gastrointestinal bleeding. Am J Surg 2000;180:181-184.
21. Landi B, Cellier C, Gaudric M, et al. Long-term outcome of patients with gastrointestinal bleeding of obscure origin explored by push enteroscopy. Endoscopy 2002;34:355-359.
22. Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol 1997;92:419- 424.
23. Kim JP, Han DS, Lee HL, et al. Clinical features of obscure-overt gastrointestinal bleeding. Korean J Gastro- enterol 2003;42:27-34.
24