2008;22:262-266 □ 증 례 □
262
책임저자:유영경, 서울시 서초구 반포동 505
가톨릭대학교 강남성모병원 간담췌외과, 137-701 Tel: 02-590-2686, Fax: 02-590-1406
E-mail: yky602@catholic.ac.kr
접수일:2008년 9월 30일, 게재승인일:2008년 11월 4일
Living-Donor Liver Transplantation with Transient Portacaval Shunt and Splenectomy in a Patient with Small-for-Size Graft and Bleeding Gastric Fundal Varices: A Case Report
Department of Hepato-Biliary-Pancreas-Surgery, The Catholic University of Korea College of Medicine, Seoul, Korea Young Kyoung You, M.D., Sang Kuon Lee, M.D., Jung Hyun Park, M.D. and Kyung Keun Lee, M.D.
위전정부 정맥류 출혈환자의 생체부분 간이식에서 작은 이식편에 대한 일시적인 문맥-하대정맥간의 우회로 형성 및 비장절제술 1예
가톨릭대학교 의과대학 강남성모병원 간담췌외과 유영경ㆍ이상권ㆍ박정현ㆍ이경근
생체부분 간이식에서 간문맥으로부터의 과도한 혈류는 작은 이식 편을 손상시키는 주요한 요인으로 지목되고 있 다. 문맥-하대정맥간의 우회로를 만들어서 간문맥 혈류의 일부를 우회시킴으로써 작은 이식 편 증후군을 예방하는 방법들이 보고되고 있다. 또한 비장 절제술은 간문맥의 혈 류를 감소시킬 뿐 아니라 위 전정부 정맥류 출혈의 치료 법이 된다. 저자들은 내시경으로 지혈하기 어려운 위 전정 부 정맥류 출혈을 하는 B형 간염에 의한 간 경화 환자에 서 작은 이식 편을 이용한 생체부분 간이식을 시행하였으 며, 일시적인 문맥-하대정맥간의 우회로 형성 및 비장절 제술을 하였다. 환자는 50세 남자이었으며 공여자는 환자 의 배우자로 이식 편 대 체중의 비가 0.64이었다. 이식 수 술 중 좌 간문맥을 하대정맥에 문합하였고, 우 간 문맥을 이식 편에 문합하였다. 모든 혈관 문합을 종료한 후 endoloop (OpenLoop
Ⓡ, SJM, Paju, Korea)을 문맥-하대정맥 우회로에 걸어 놓고 매듭을 조이지 않은 채로 매듭 조임 막대를 실라스틱 배액관을 통해 복부외부로 유치하였다.
수술 중 비장 절제술을 시행하였으며, 이식 수술을 종료한 지 24 시간 후에 복부 외부로 유치한 매듭 조임 막대를 이용하여 마취 없이 문맥-하대정맥 우회로를 폐쇄하였다.
환자는 이식수술 26일 째 좋은 상태로 회복하여 퇴원하였 다. 생체부분 간이식에서 일시적인 문맥-하대정맥간의 우 회로 형성 및 비장절제술은 작은 이식 편과 위 전정부 정 맥류 출혈환자에서 행할 수 있는 치료법이라 할 수 있다.
(대한이식학회지 2008;22:262-266)
중심 단어: 생체부분 간이식, 일시적인 간문맥-하대 정맥 우회로, 작은 이식편, 비장절제술
INTRODUCTION
In the era of living-donor liver transplantation, most liver graft volume would be inevitably small-for-size. In general, patients with graft-to-recipient body weight ratio (GRWR) larger than 0.8% have been recovered without problem associated with small-for-size graft volume.(1) Possible mechanism underlying hazard of the small-for-size liver graft comes from the ische- mia-reperfusion injury exaggerating portal hyperperfusion in- jury to the graft.(2) To avoid excessive portal venous inflow, promising partial diversion of the portal flow to the systemic circulation through a portacaval or mesocaval shunt in the small-for-size liver graft was reported recently.(3-5) Permanent portacaval shunt might steal the portal inflow paradoxically, so the shunt needs to be occluded.(3) Taniguchi et al.(6) recently reported innovative surgical technique of transient portacaval shunt with Endoloop, which can be occluded in the late period of transplantation without laparotomy. For reducing portal per- fusion and pressure, splenic artery ligation or splenectomy is proposed as one of the solution.(7) However, splenectomy is seldom recommended because it has the risk of portal vein thrombosis in some circumstances. In contrast, in patients with gastric fundal variceal bleeding, splenectomy has been one of the best surgical procedures to solve the problem.
Herein, we describe living-donor liver transplantation with
transient portacaval shunt and splenectomy for a patient with
small-for-size graft and bleeding gastric fundal varices.
Fig. 1. Living-donor liver transplantation using right lobe. A portacaval shunt was made using recipient’s left portal venous end anastomosing to inferior vena cava in end-to-side fashion (black arrow). Middle hepatic vein was reconstructed using Dacron interposition graft to the graft right hepatic vein to make a large single hole (black arrow).
Fig. 2. Baseline portal pressure was 45 cm H20 and after portacaval shunt formation portal pressure decreased to 30 cm H20. After liver graft reperfusion, it was decreased around 25 cm H20. After subsequent splenectomy and focal devascularization procedure at the gastric fundal area, portal pressure still maintained around 23 cm H20.
Throughout the procedure central venous pressure was maintained between 6 to 10 cm H20.
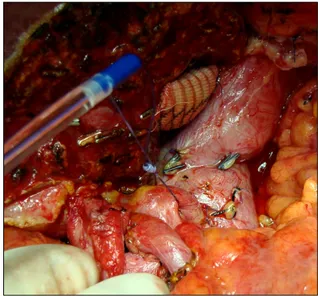
Fig. 3. An endoloop (OpenLoopⓇ, SJM, Paju, Korea) was placed around portacaval shunt without tightening.
CASE REPORT
A 50 year-old male (178 cm, 89 kg) had been diagnosed with liver cirrhosis related to hepatitis B virus for over 10 years.
Liver function had gradually deteriorated and clinically man- ifested as gastric fundal variceal bleeding, which was not ame- nable to be controlled with repeated endoscopic trials (MELD score ; 18). Living-donor liver transplantation using the right hemiliver (570 gram, graft-to-body weight ratio : 0.64) from his spouse (158 cm, 48 kg) was performed.
Operative Procedure & Postoperative Course
At surgery, cirrhotic liver, splenomegaly and huge engorged collateral veins were found in the perigastric area and gigantic subserosal venous collaterals were focused at the gastric fundus.
Throughout the procedure, portal pressure was monitored via superior mesenteric vein catheterization using 4 Fr. Nutricath
Ⓡ(Vygon, Ecouen, France). A portacaval shunt was made using recipient’s left portal vein end to the inferior vena cava (IVC) and total hepatectomy with preservation of IVC was performed as usual manner (Fig. 1). Recipient’s right portal vein was pre- pared for the anatomosis to the graft portal vein. A right hepatic lobe graft was harvested from his 42 year-old wife. At back table, the main right hepatic vein of the graft and the middle
hepatic vein was anastomosed using a 10-mm in diameter
Dacron interposition graft to make a large single hole for the
anastomosis. There was an additional inferior right hepatic vein,
about 11 mm in diameter. Then, the liver graft was placed or-
thotopically and all of the graft hepatic veins were anastomosed
to the inferior vena cava. The graft portal vein was anasto-
mosed to the recipient main portal vein trunk. The clamps ap-
plied to the hepatic venous outflows and portal inflow were re-
Fig. 4. The knot pusher was brought out through abdominal wall introduced in a silastic drain tube.
Fig. 5. Twenty-four hours after transplantation, the endoloop placed around portacaval shunt was tightened as a bedside procedure.
moved, and the liver graft was reperfused. The cold and warm ischemic time was 70 min and 35 min, respectively. The liver was reperfused promptly from the blood flow through the portal vein. Using microsurgical technique, the arterial anastomosis was performed. Baseline portal pressure was 45 cm H
20, and after portacaval shunt formation, portal pressure decreased to 30 cm H
20. After liver graft reperfusion, it was decreased around 25 cm H
20. After subsequent splenectomy and focal de- vascularization procedure at the gastric fundal area, portal pres- sure still maintained around 23 cm H
20. Throughout the proce- dure central venous pressure was maintained between 6 to 10
cm H
20 (Fig. 2). An endoloop (OpenLoop
Ⓡ, SJM, Paju, Korea) was placed around portacaval shunt without tightening, and the knot pusher was brought out through abdominal wall introduced in a silastic drain tube (Fig. 3, 4). Then, duct-to-duct biliary re- construction was done. Adequate blood flow in the intrahepatic portal vein, hepatic artery and hepatic veins were detected on intraoperative Doppler ultrasonography before abdominal wall closure. Twenty-four hours after transplantation, the loop placed around portacaval shunt was tightened as a bedside procedure (Fig. 5). The recipient had an uneventful postoperative course and was discharged with normal graft function 26 days after transplantation.
DISCUSSION
In living-donor liver transplantation, donor safety is the prime concern. Because of limited donor pool, inevitable small-for-size graft has not been uncommon. Not all small-for-size grafts pro- voke small-for-size graft syndrome, which is manifested by per- sistent hyperbilirubinemia due to persistent cholestasis, ascites and coagulopathy from delayed synthetic function, resulting in reduced graft survival.(1) There are many factor modifying small-for-size effects to the recipient such as recipient factors (age, original disease, presence of ascites and collateral circu- lation), and donor factors (age, steatosis and warm/cold ische- mia, etc.)(1) The direct mechanism leading to poor outcome in patients receiving small-for-size graft is still unclear. The hep- atic parenchymal cell mass shortage to the metabolic demand is a possible underlying phenomenon. Damage from the relative large portal flow volume and elevated pressure to the small-for- size graft has been partly proven in some studies.(2-5) Among those, portal inflow diversion is one of the promising surgical measures preventing from small-for-size graft syndrome. None- theless, in the late period of recovery after living-donor liver transplantation, portal diversion is no longer needed, and portal flow steal could cause hazardous effects to the graft. Taniguchi et al. reported innovative surgical procedure using endoloop which does not require reoperation to close portacaval shunt in small-for-size graft living-donor liver transplantation.(6) And also the endoloop (OpenLoop
Ⓡ) is manufacture as free one arm, therefore it is easy to encircle the vessel after the anastomosis.
In our case, an endoloop was used for bedside ligation of the
portacaval shunt. In contrast to Taniguchi et al. who occluded
the shunt on 2nd week after surgery, we did it 24 hours after
transplantation. There were two reasons to decide early ligation
of portacaval shunt. Our belief is that small-for-size graft injury
commences from the initial moment of reperfusion and it trig-
gers a cascade of deleterious events several minutes after. Hemo- dynamic instability after reperfusion usually lasts only several minutes and various cytokines and toxic agents produced by the graft enter into the circulation. This process is overcome in just 10 minutes after reperfusion; therefore, the most important mo- ment to avoid hyperperfusion to the graft is the initial several minutes after reperfusion. Nevertheless, this hypothesis has to be further studied. The other reason is the potential risk of in- jury by the knot pusher of the endoloop. As it remains in the abdominal cavity, violent movements of the patient could cause catastrophic consequences. Since the recipient is usually kept in ventilator 24 hours after transplantation, it is advisable to re- move the knot pusher just before the endotracheal extubation.
During the transplantation surgery, portacaval shunt reduced the initial portal pressure from 45 to 25 cm H
20 and active vari- ceal bleeding was reduced, but not completely controlled. The correlation of portal pressure and the severity of the graft dam- age are things to be determined. But the personal cut-off value of the portal-systemic pressure gradient that seems to be con- trolled in the liver transplantation procedure is 20 cm H
20 in our series, which should be determined objectively in the future.
After the liver graft implantation, concomitant splenectomy was performed and adult finger-tip sized engorged gastric fundal variceal collaterals were meticulously ligated and gastric bleed- ing was finally controlled. Especially in left side portal hyper- tension, splenectomy has been the surgical treatment of choice;
however, it is well known that portal thrombosis is one of the lethal complications after splenectomy in a liver transplant pa- tient
3. For this reason, splenectomy is not recommended as a routine procedure to lower portal venous pressure during liver transplantation. However we did not do any prophylactic treat- ment to prevent from portal vein thrombosis except routine transplantation protocols. The recipient stayed in intensive care unit for 5 days after transplantation, had an uneventful post-
operative course, and was discharged with normal graft function 26 days after transplantation.
In conclusion, living-donor liver transplantation with transient portacaval shunt and splenectomy could be an acceptable surgi- cal treatment strategy for patient with end-stage liver disease with small-for-size graft and bleeding gastric fundal varices.
REFERENCES
1) Kiuchi T, Tanaka K, Ito T, Oike F, Ogura Y, Fujimoto Y, et al. Small-for-size graft in living donor liver transplantation:
how far should we go? Liver Transpl 2003;9:29-35.
2) Farantos C, Arkadopoulos N, Theodoraki K, Kostopanagiotou G, Katis K, Tzavara K, et al. Effect of portacaval shunt on reperfusion injury after 65% hepatectomy in pigs. Euro Surg Res 2008;40:347-53.
3) Yamada T, Tanaka K, Uryuhara K, Ito K, Takada Y, Uemoto S. Selective hemi-portocaval shunt based on portal vein pressure for small-for-size graft in adult living donor liver transplantation. Am J Transpl 2008;8:847-53.
4) Troisi R, Ricciardi S, Smeets P, Petrovic M, Van Maele G, Colle I, et al. Effects of hemi-portocaval shunts for inflow modulation on the outcome of small-for-size grafts in living donor liver transplantation. Am J Transpl 2005;5:1397-404.
5) Boilot O, Delafosse B, Mechet I, Boucaud C, Pouyet M.
Small-for-size partial liver graft in an adult recipient; a new transplant technique. Lancet 2002;359:406-7.
6) Taniguchi M, Shimamura T, Suzuki T, Yamashita K, Oura T, Watanabe M, et al. Transient portacaval shunt for a small-for-size graft in living donor liver transplantation. Liver Transpl 2007;13:932-4.
7) Gruttadauria S, Mandala' L, Miraglia R, Caruso S, Minervini MI, Biondo D, et al. Successful treatment of small-for-size syndrome in adult-to-adult living-related liver transplantation:
single center series. Clin Transplant 2007;21:761-6.
Excessive portal venous inflow has been known as a determining factor for hepatic injury in small-for-size graft in living-donor liver transplantation. Partial diversion of portal inflow to the systemic circulation by portacaval shunt has been reported as a promising treatment modality to prevent patient from small-for-size graft syndrome. In addition, splenectomy itself is not only a method to decrease portal flow, but also a treatment for the gastric fundal variceal bleeding. We performed living-donor liver transplantation with transient portacaval shunt and splenectomy due to small-for-size graft in a 50 year-old male suffering from hepatitis B virus related liver cirrhosis with bleeding gastric fundal varices, not amenable to control endoscopically. The donor was patient’s wife and a graft to recipient body weight ratio (GRWR) was 0.64. During surgery, left portal vein was used for temporary portacaval shunt and the right portal vein was anatomosed to the graft portal vein. After all vascular anastomoses completed, an endoloop (OpenLoopⓇ, SJM, Paju, Korea) was placed around portacaval shunt without tightening, and the knot pusher was brought out through abdominal wall introduced in a silastic drain tube. Concomitant splenectomy was performed. Twenty-four hours after transplantation, the loop placed around portacaval shunt was tightened as a bedside procedure. The recipient had an uneventful postoperative course and was discharged with normal graft function 26 days after transplantation. Living-donor liver transplantation with transient portacaval shunt and splenectomy could be an acceptable surgical treatment strategy for patients with end-stage liver disease with small-for-size graft and bleeding gastric fundal varices. (J Korean Soc Transplant 2008;22:262-266)
Key Words: Living-donor liver transplantation, Transient portacaval shunt, Small-for size graft, Splenectomy