Axillary lymph node status is important for staging, prognosis and determining the optimal treatment for breast cancer. Axillary lymph node metastasis occurs in 30-40% of all patients with breast cancers (1, 2). A physical examination alone is neither a sensitive nor re- liable way to ascertain lymph node status because the
metastatic lymph nodes are often not palpable and reac- tive lymph nodes may be mistaken for metastasis (3, 4).
There are several imaging techniques that have been used to evaluate lymph nodes, including mammogra- phy, computed tomography (CT), MR imaging, lym- phangiography and scintigraphy, and all these methods have unsatisfactory sensitivity and specificity. For ex- ample, the sensitivity of mammography ranges from 18- 41% and the specificity ranges from 80-90% (4-6). The sensitivity of CT is 50% and its specificity is about 75%
(7). Among the imaging modalities, ultrasound has been the most frequently investigated because of its noninva- sive nature and the ease of its use for evaluating the axil-
The Value of Ultrasonographic Detection for Metastatic Axillary Lymph Nodes in Breast Cancer
1Jung Hee Shin, M.D., Asiry Hwang, M.D., Hye-Young Choi, M.D., Seung Yon Baek, M.D.
Purpose: We evaluated the significance and accuracy of sonographic detection of metastatic axillary lymph nodes (LNs) in breast cancer.
Materials and Methods: We retrospectively reviewed the sonographic findings and postoperative results of axillary LNs in 47 patients with breast cancer. The sonograph- ic criteria for metastatic LNs were defined as the loss of the echogenic hilum and any uneven cortical thickness of over 3 mm. We analyzed the correlation between the pre- operative sonographic findings and the postoperative results of the LNs.
Results: Out of 47 patients, 22 patients showed 43 sonographic metastatic LNs.
Among these 22 patients, 18 patients had 183 histopathologically proven metastatic LNs. The pathological examination of the remaining 25 patients revealed metastatic LNs in 6 patients. The overall sensitivity, specificity and accuracy of ultrasonography for detecting metastatic axillary LNs in breast cancer were 75%, 82.6% and 78.7%, re- spectively. As the number of metastatic LNs detected on sonography increased, the number of histologically proven metastatic LNs increased.
Conclusion:Ultrasonographic evaluation of axillary LNs in breast cancer can provide relatively accurate information about the presence or absence of metastasis.
Therefore, it is useful to decide the initial staging and treatment planning of patients with breast cancer.
Index words :Breast neoplasms Ultrasonography Lymph Nodes
1Department of Radiology, College of Medicine, Ewha Womans University
Received March 2, 2004 ; Accepted Decemebr 1, 2004
Address reprint requests to : Hye-Young Choi, M.D., Department of Radiology, Ewha Womans University, Mokdong Hospital, 911-1 Mok- dong, Yangcheon-gu, Seoul 158-710, Korea.
Tel. 82-2-2650-5173 Fax. 82-2-2650-5302 E-mail:choihy@hanmail.net
la. It is used to detect alterations in the size, shape and contours of lymph nodes, as well as detecting changes in the morphology and texture of the nodal cortex: it can thereby identify the presence of the underlying metasta- sis (6).
The purpose of this study was to evaluate the signifi- cance and accuracy for the sonographic detection of metastatic axillary lymph nodes in breast cancer.
Materials and Methods
During a 3-year period, forty-seven patients with breast cancer underwent formal axillary lymph node dissection together with or immediately after lumpecto- my or mastectomy, and all the patients were histologi- cally proved as having an invasive breast cancer. In these 47 patients (46 females and one male), the preop- erative ultrasonographic (US) images and postoperative histologic findings of the axillary lymph nodes were ana- lyzed. We excluded those patients with unavailable pre- operative US findings. The patients’ ages ranged from 25 to 75 years (mean age: 46 years).
All the scans were performed by an experienced radi- ologist with real-time ultrasound using a 10 MHz linear array probe XP 10 (Acuson, Moutain view, CA), or an HDI 5000 (Advanced Technology Laboratories, Bothell, WA). A careful search for adenopathy was performed along the axilla in the longitudinal and transverse planes using the axillary vessels as landmarks. On preoperative US, we evaluated the size of the breast cancer, the pres- ence of echogenic hilum, the uneven degree of cortical thickness and the number of axillary lymph nodes.
Sono-graphic criteria of metastatic lymph nodes were defined as the loss of the echogenic fatty hilum and any uneven cortical thickness over 3 mm. We then analyzed the correlation between the preoperative US findings that were suggestive of metastatic lymph nodes and the postoperative results. For the control study (48 lymph nodes in 31 negative cases), the ratio of the shortest axis to the longest axis (S/L), the cortical thickness, and the obliteration of the echogenic hilum of the lymph nodes were compared between the metastatic and benign lymph nodes. For statistical analysis, Spearman’s corre- lation coefficients were obtained. Correlation was con- sidered significant at the 0.01 level.
Results
Out of 47 patients, 22 patients showed 43 lymph
nodes that were suggestive of metastasis on US exami- nation. Axillary dissection revealed metastasis in 24 of 47 patients (51.1%). The correlation between the ultra- sonography and histopathology is presented in Table 1.
Among the 22 sonographically positive patients, 18 pa- tients (18/22, 81.8%) had histopathologically proven breast cancers with 183 metastatic lymph nodes (Fig. 1).
The remaining 25 patients revealed no evidence of metastatic lymph nodes on US (Fig. 2), but 6 of these pa- tients (6/25, 24%) were histologically confirmed as hav- ing 11 metastatic lymph nodes. Each of these 6 patients had three or less metastatic lymph nodes on histologic examination. One of four false positive patients was confirmed histologically as having tuberculous lym- phadenitis. Three false positive patients showed reac- tive hyperplasia. The overall sensitivity of ultrasonogra- phy for the detection of metastatic axillary lymph nodes in breast cancer was 75%, the specificity was 82.6%, the accuracy was 78.7%, the positive predictive value was 81.8% and the negative predictive value was 76%. The greater the number of nodes that were suggestive of metastasis on US, the greater was the number of histo-
Table 1. Correlation between Ultrasonography and Histology Histologic Findings
No. of patients Positive Negative Total
US Positive 18 04 22
Negative 06 19 25
Total 24 23 47
No.: Number, US: Ultrasonography
Table 2. Correlation between Metastatic Lymph Nodes on Ultra- sonography and Histologically Positive Lymph Nodes
No. of metastatic No. of patients Mean No. of histologically LNs on US positive LNs
0 25 0.44
1 10 4
2-3 10 5.7
≥4 02 23
No.: Number, LNs: lymph nodes, US: Ultrasonography
Table 3. Correlation between Tumor Size and Number of Metastatic Lymph Nodes
Tumor size (cm) No. /A total of patients Mean No.
with positive LNs (%) of positive LNs
≤1 1 / 5 (20) 0.2
1-2 5 / 14 (35.7) 1.57
2-5 17 / 27 (63) 3.78
>5 1/1 (100) 19
No.: Number, LNs: lymph nodes
logically proven metastatic lymph nodes that were iden- tified (p<0.01)(Table 2). Moreover, there was a statisti- cally significant correlation between the size of the breast mass and the number of histologically proven metastatic lymph nodes (p<0.01) (Table 3). When com- paring the control and metastatic lymph nodes, the ratio of the shortest axis to the longest axis (S/L), and the corti- cal thickness were 0.38 and 1.46 mm, respectively, in the benign nodes and 0.74 and 6.11 mm, respectively, in the metastatic nodes. Twenty-seven (81.8%) of thirty-
three lymph nodes that were suggestive of metastasis on US showed the obliteration of the fatty hilum. All three of the criteria we selected for the presence of metastasis showed statistically significant results (p<0.01).
Discussion
The axillary lymph node status is, in the absence of distant metastasis, the single most important factor for predicting breast cancer patient survival. Axillary
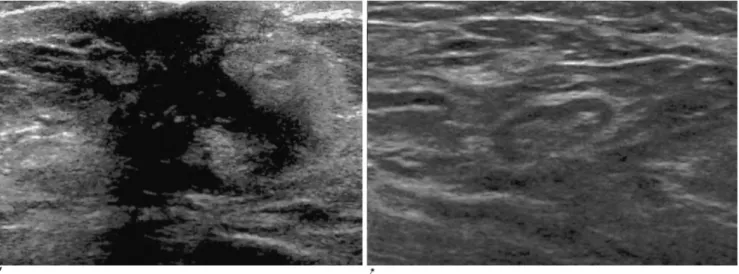
A B
Fig. 2. A 43-year-old woman with breast cancer.
A. An indistinct hypoechoic lesion is noted in the right subareolar area that measured about 2.2 cm in width.
B. An axillary lymph node shows the even cortical thickness and the visualization of the echogenic hilum, representing no evi- dence of metastasis on US, but this node revealed the presence of metastasis on pathology.
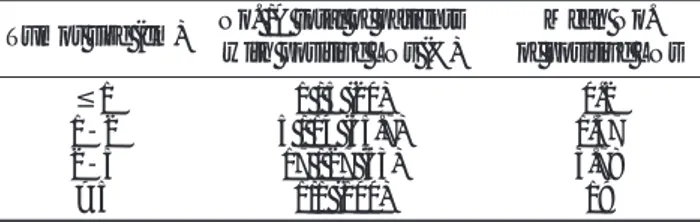
A
B
Fig. 1. A 56-year-old woman with breast cancer.
A. An inhomogeneous hypoechoic mass is noted in the upper outer portion of the right breast. This mass measured about 4.3×4.1 cm in size.
B. An ipsilateral axillary lymph node of the same patient shows uneven cortical thickness of more than 3 mm (arrow) with preservation of echogenic hilum, which was compatible with the malignant criteria used in our study. This node had proven pathologically metastasis of the infiltrating ductal carcinoma.
lymph node dissection is routinely performed as a part of the surgical treatment for breast cancer, and it is mainly done for staging and planning the adjuvant ther- apy according to the number of metastatic lymph nodes that are found (1, 2). However, in most patients, axillary dissection has proved to have been unnecessary after the histological node examination. Moreover, axillary node dissection has significant complications, such as lymphedema, pain in the arm, nerve injury and a pro- longed hospital stay. The newer surgical approaches, such as sentinel node dissection or selective node dissec- tion, have been proposed to reduce the number of un- necessary axillary dissections and these techniques are currently under investigation. An accurate noninvasive preoperative diagnostic method to assess the axillary lymph node status would help reduce the need for axil- lary operations.
US has been proved to have a higher sensitivity (45- 84%) and specificity (72-97%) for the detection of metastatic axillary lymph nodes in breast cancer than a clinical examination or the other imaging techniques (3-6, 8). Similar to the results of earlier studies, the sen- sitivity, specificity and accuracy of ultrasonography were 75%, 82.6% and 78.7%, respectively, in our cur- rent study. According to previous studies, false negative cases had three or less microscopically invaded lymph nodes on histologic examination (9, 10). In our study, the six false negative patients had less than three metastatic lymph nodes. It appears that the common factors associated with the discrepancy between the US findings and the pathological results are the failure to vi- sualize lymph nodes during US examination of the axil- la, the small number of metastatic lymph nodes and the presence of micrometastasis. Ultrasonography alone cannot always differentiate reactive or inflammatory conditions from the malignant causes due to the overlap of their sonographic features. The four false positive cas- es in our study were considered to be benign reactive hyperplasia, and one of these cases was confirmed by histology as tuberculous lymphadenitis. As for the caus- es of the other false positive nodes, pathological sinusoid hyperplasia and irregular, thickened capsules represent- ed the uneven sonographic cortical thickening. Also, the rich vascular structures within the lymph node can cause the compression or absence of hilum. US-guided fine-needle aspiration (FNA) may increase the specifici- ty or reliability in such cases. In a study by Kirshna- murthy et al, the overall sensitivity, specificity, diagnos- tic accuracy, positive predictive value and negative pre-
dictive value of US-guided FNA were 86.4%, 100%, 79%, 100% and 67%, respectively (10).
There was a positive correlation between the number of nodes that were suggestive of metastasis on US and the number of histologically proven metastatic lymph nodes that were identified (p<0.01).
According to Lam and associates and also Yang and colleagues, a normal axillary lymph node was defined as having an ovoid hypoechoic C-shaped rim of lymphoid tissue (usually 1 to 2 mm thick) around a central echogenic fatty hilum, and lymph nodes that were sug- gestive of metastasis were rounded and hypoechoic with or without the associated eccentric cortical hyper- trophy and obliteration of the fatty hilum (5, 6). Size was not considered an important factor. In an in vitro US study for axillary node analysis by Feu et al., absence of the hilum was found to be the most specific sonographic feature for the diagnosis of metastasis (12). The in- creased long-to-short axis ratio was the finding that caused the most false-negative interpretations, indicat- ing that lymph nodes appearing elongated or ovoid can be metastatic. Yet in other study by Tateishi et al, a cir- cular shape (i.e., a ratio between 0.5 and 1.0 for the shortest axis to the longest axis) was the best single fea- ture for distinguishing metastatic from nonmetastatic lymph nodes (13). In our study, we defined metastatic lymph nodes as those nodes having obliteration of the fatty hilum and if they had over 3mm of uneven cortical thickness.
The prevalence of axillary nodal involvement in breast cancer is 40-70%, and the prevalence of axillary nodal involvement has been shown to be related to tu- mor size. The risk for having a positive node is known to be 30% if the primary tumor is larger than 1 cm, and it’s 15% if the primary tumor is less than 1 cm. In patients with T3 cancer, up to 60% will have axillary nodal metastasis at presentation (14). In a current study, there was a statistically significant correlation between the size of the breast mass and the number of proven metastatic lymph nodes (p<0.01).
The accuracy of ultrasonographic axillary lymph node detection will probably improve with the support of more advanced sonographic scanners and better-de- fined nodal differential criteria. Additional studies will be necessary to determine the value of ultrasonographic evaluation for the detection of metastatic axillary lymph nodes due to the limited number of cases in this study.
In conclusion, if the axillary lymph nodes in patients with breast cancer show an increased ratio of the short-
est axis to the longest axis, the obliteration of fatty hilum and over 3 mm of uneven cortical thickness on US, then they should be considered as having metastasis. As the number of metastatic LNs detected on US was higher or the size of breast mass was larger, the number of histo- logically proven metastatic nodes increased. The rela- tively high accuracy and the positive and negative pre- dictive values of US for detecting metastatic axillary lymph nodes indicate that it is a useful modality for the initial staging of breast cancer, and this US modality can be immensely valuable for planning the appropriate management of breast cancer patients.
References
1. Fisher B, Bauer M, Wickerham L, Redmond C, Fisher E. Relation of number of positive axillary nodes to the prognosis of patients with primary breast cancer. Cancer 1983;52:1551-1557
2. Ruffin WK, Stacey-Clear A, Younger J, Hoover HC Jr. Rationale for routine axillary dissection in carcinoma of the breast. J Am Coll Surg 1995;180:245-251
3. DeFreitas R Jr, Costa MV, Schneider SV, Nicolau MA, Marussi E.
Accuracy of ultrasound and clinical examination in the diagnosis of axillary lymph node metastasis in breast cancer. Eur J Surg Oncol 1991;17:240-244
4. Pamilo M, Soiva M, Lavast EM. Real time ultrasound, axillary mammography and clinical examination in the detection of axil- lary lymph node metastases in breast cancer patients. J Ultrasound Med 1989;8:115-120
5. Lam WW, Yang WT, Chan YL, Stewart IE, Metrewelic, King W.
Detection of axillary lymph node metastases in breast carcinoma by technetium-99m sestamibi breast scintigraphy, ultrasound and conventional mammography. Eur J Nucl Med 1996;23:498-503 6. Yang WT, Ahuja A, Tang A, Suen M, King W, Metrewelic. High
resolution sonographic detection of axillary lymph node metas- tases in breast cancer. J Ultrasound Med 1996;15:241-246
7. March DE, Wechsler RJ, Kurtz AB, Rosenberg AL, Needleman L.
CT pathologic correlation of axillary lymph nodes in breast carci- noma. J Comput Assist Tomogr 1991;15:440-444
8. Bruneton JN, Caramella E, Hery M, Aubanel D, Manzino JJ, Picard JL. Axillary lymph node metastasis in breast cancer : preop- erative detection with US. Radiology 1986;158:325-326
9. Verbanck J, Vandewiele I, De Winter H, Tytgat J, Van Aelst F, Tanghe W. Value of axillary ultrasonography and sonographically guided puncture of axillary nodes: a prospective study in 144 con- secutive patients. J Clin Ultrasound 1997;25:53-56
10. Krishnamurthy S, Sneige N, Bedi DG, Edieken BS, Fornage BD, Kuerer HH, et al. Role of ultrasound-guided fine-needle aspiration of indeterminate and suspicious axillary lymph nodes in the initial staging of breast carcinoma. Cancer 2002;95:982-988
11. Yang WT, Ahuja A, Tang A, Suen M, King W, Metreweli C.
Ultrasonographic demonstration of normal axillary lymph nodes - a learning curve. J Ultrasound Med 1995;14:823-827
12. Feu J, Tresserra F, Fabregas R, Navarro B, Grases PJ, Suris JC, et al. Metastatic breast carcinoma in axillary lymph nodes: in vitro US detection. Radiology 1997;205: 831-835
13. Tateishi T, Machi J, Feleppa EJ, Oishi R, Furumoto N, McCarthy LJ, et al. In vitro B-mode ultrasonographic criteria for diagnosing axillary lymph node metastasis of breast cancer. J Ultrasound Med 1999;18:349-356
14. Carter CL, Allen C, Henson DE. Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer 1989;63:181-187
대한영상의학회지 2005;52:45-49
유방암의 액와 림프절 전이에 대한 초음파 검사의 가치1
1이화여자대학교 의과대학 이대목동병원 방사선과 신정희・황아실이・최혜영・백승연
목적:유방암 환자에서 액와 림프절의 전이 유무를 알아보기 위한 초음파 검사의 진단적 정확성과 가치를 알아 보고자 하였다.
대상과 방법:수술 전 초음파 검사에서 액와 림프절 전이 유무와 수술 후 전이 여부를 알고 있는 47명의 유방암 환자를
대상으로 하였다. 전이된 림프절의 초음파적 진단 기준은 에코성의 문의 소실과 3 mm 이상의 비균일한 피질 두께를 가 질 경우로 정의하였다. 수술 전 림프절의 초음파 소견과 수술 후 결과 사이의 관계를 분석했다.
결과:47명 중 22명의 환자에서 초음파 검사로 43개 림프절의 전이가 진단되었다. 22명의 환자 중 18명에서 병리조직 학적으로 183개의 액와 림프절 전이가 확진되었다. 초음파 검사에서 나머지 25명은 전이된 림프절이 발견되지 않았으 나 이 중 6명은 병리조직학적으로 7개의 림프절 전이가 확진되었다. 유방암에서 전이된 액와 림프절의 발견에 대한 초 음파의 진단적 예민도, 특이도, 그리고 정확도는 각각 75%, 82.6%, 78.7% 였다. 초음파 검사에서 전이된 림프절의 수 가 많이 보일수록, 병리적으로도 전이된 림프절의 수가 증가하였다.
결론:유방암에서 액와 림프절의 초음파 검사는 전이의 유무에 대한 비교적 정확한 정보를 제공한다. 그러므로 유방암 환자의 액와 림프절 검사는 초기 병기와 치료 계획을 결정하는 데 도움을 주는 필요한 검사라고 생각된다.