The fractures of the proximal humerus are the third most com- mon type of fracture seen in the elderly patient population and account for 10 percent of all fractures in patients over sixty-five years of age1). Undisplaced fractures are the most common and it is generally agreed that they have a good prognosis after con- servative treatment18,19). The management of displaced fractures, however, remains controversial. A variety of operative techniques have been reported, including external fixation, AO buttress plat- ing, blade plate fixation, tension band wiring, Rush rod fixation, flexible Ender nail fixation and percutaneous pinning21,26). Despite the multitude of techniques employed, guideline for the optimal treatment of proximal humeral fractures is not always clear.
One of the major problems in surgical treatment is the high incidence of comminuted fractures in elderly patients with osteo- porotic bone which dose not allow stable internal fixation and early active exercise. Unfavorable results seen after fixation are commonly attributed to the osteopenia of the proximal humerus in the elderly, and to the extensive soft tissue stripping that is
required to adequately visualize the fracture fragments. Because extensive exposure and insertion of large implants increase the risk of avascular necrosis25), the use of a limited exposure and min- imal internal fixation has been recommended12,24).
The purposes of this study were to introduce a surgical tech- nique of retrograde pin fixation with tension band wiring for the proximal humeral fractures and to evaluate the clinical results.
MATERIALS AND METHODS
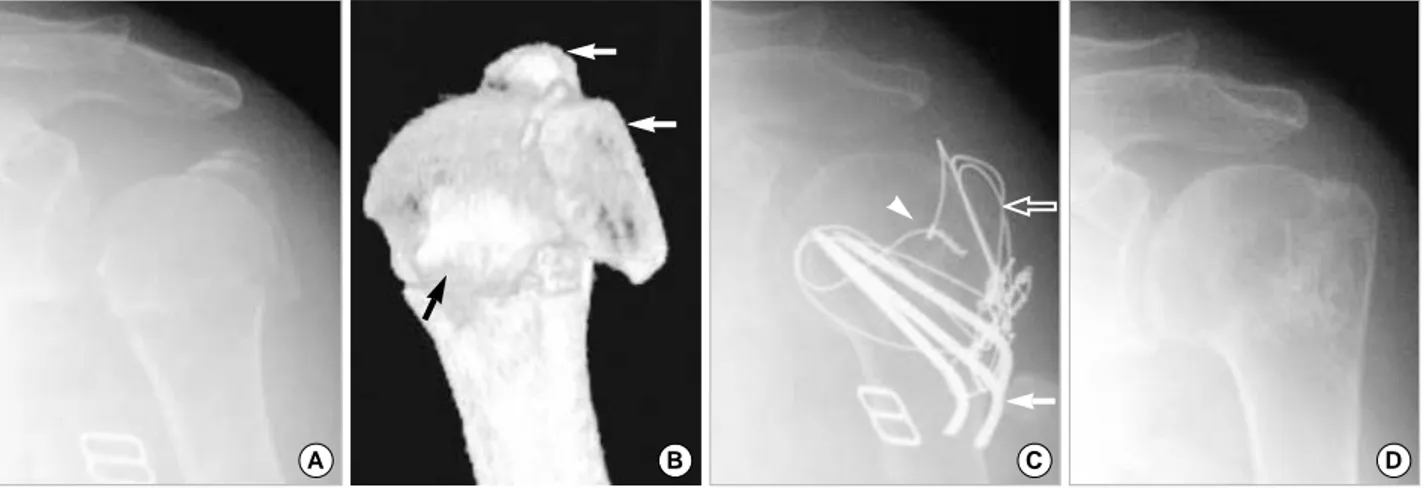
During the five-year period from June 1996 to June 2001, thirty-four patients were treated surgically using retrograde pin fixation with tension band wiring for the proximal humeral frac- tures by a single surgeon (J-M C). Thirty-two patients were avail- able for review. There were seventeen women and fifteen men. The average age was fifty-five years (range, 25-83). The fracture type was classified according to Neer18). Twelve patients had a two-part fracture, and twenty patients had a three-part fracture. Four cases of the three-part fractures were valgus impacted fractures (Fig. 1A, B) and three cases were fractures with varus displacement. There was no history of previous injury or surgery to the shoulder in any patient. All were treated by internal fixation using the retro- grade pin fixation with tension band wiring technique and were examined both clinically and radiologically, with a minimum
498 498 498 498 Address reprint requests to
Jae-Myeung Chun, M.D.
Department of Orthopaedic Surgery, Asan Medical Center University of Ulsan College of Medicine, 388-1 Pungnap-2dong, Songpa-gu, Seoul 138-736, Korea Tel: +82.2-3010-3530, Fax: +82.2-448-7877
E-mail: jmchun@www.amc.seoul.kr
Purpose:To introduce a surgical technique of retrograde pin fixation with tension band wiring for the proximal humeral fractures and to evaluate the clinical results.
Materials and Methods:The clinical results of thirty-two patients who underwent surgical treatment for the proximal humeral fractures, during the period from June 1996 to June 2001, using a retrograde pin fixation with tension band wiring were reviewed. The mean follow up was 2.5 years (1-5 years) Twelve patients had a two-part fracture, and twenty patients had a three-part fracture with Neer’s classifica- tion. We analyzed the clinical results using Neer score and radiological state using Zyto’s three-point graded scale.
Results:By clinical evaluation, eighteen cases (56%) were excellent, twelve cases (38%) were satisfactory, one case (3%) was unsatis- factory and one case (3%) was failure. By radiological evaluation, twenty-one cases (66%) were good, nine cases (28%) were accept- able and two cases (6%) were poor. Three unsatisfactory cases were a case with pin migration, loss of reduction or avascular necrosis.
There was not a case of delayed union, nonunion or infection.
Conclusion:Retrograde pin fixation with tension band wiring for the proximal humeral fractures was considered to be a useful method, which is easy and induces limited soft tissue injury, and provides enough stability for postoperative rehabilitation in majority cases such as surgical neck or three-part fractures.
Key Words:Shoulder, Proximal humeral fractures, Retrograde pin fixation with tension band wiring
Retrograde Pin Fixation with Tension Band Wiring for the Proximal Humeral Fractures
Jae-Myeung Chun, M.D., Soung-Yon Kim, M.D.*, Sang Won Lee, M.D., Kyoung Hwan Kim, M.D.*, Jong Ha Lee, M.D.*
Department of Orthopaedic Surgery, Asan Medical Center, Gangneung Asan Hospital*, University of Ulsan College of Medicine, Seoul, Korea
follow-up of one year (average: two years six months, range: 1-5 years).
1. Surgical techniques
Under general anesthesia, the patient was secured in the modi- fied beach chair position (about 30 degree upright position) with a rolled towel under the medial border of the scapula. An image intensifier was positioned before surgery parallel to the edge of the table so that we could visualize the proximal humerus and glenoid in both anteroposterior and axillary planes. A standard anterior incision measuring ten to fifteen centimeters in length was made, running lateral to the coracoid process down to the proximal portion to the deltoid tuberosity. Deltopectoral inter- val was identified and cephalic vein retracted laterally. Deltoid origin was left intact. A retractor was placed deep to the deltoid, along the lateral margin of the humeral head and superficial to the rotator cuff, and the arm was abducted. The long head of the biceps tendon was identified as a landmark between the lesser and greater tuberosities. For ease of mobilization to correct the varus or valgus tilting of the humeral head or reduction of the tuberosity fragment, several stay sutures were routinely placed at the lesser and greater tuberosity cuff junction in all type of fracture. This provided good control of the tuberosity fragments and reduction of the head to the shaft. Traction on the sutures enabled the fragments to be manipulated into its anatomical location. Reduction was also possible by manipulating the posi- tion of the arm and by elevation of the humeral head using Cobb’s
elevator or a Steinmann pin inserted into the humeral head (Joy stick method) in the cases of impacted fracture. If the reduction was adequate under fluoroscopy, retrograde insertion of # 2 Stein- mann pin was performed from the shaft 2-3 cm below the frac- ture site to the humeral head in all cases. Possible pin placement options were retrograde anterior, anterolateral and lateral. After retrograde insertion of two or three Steinmann pins, twenty gauge wire was passed through the rotator cuff just proximal to the greater tuberosity and the distal end of the wire was passed around previously inserted Steinmann pins in a figure of eight fashion with tension band mode. By the same manner, tension band wiring was also applied between the subscapularis tendon at the lesser tuberosity and Steinmann pins. The wires were snugly tightened under tension and distal ends of the Steinmann pins were cut and bent to form loops with an AO wire bender. In markedly displaced three-part fractures, an additional tension band wire was applied in a figure of eight fashion between the posterior and anterior cuffs (Fig. 1C). Pendulum exercise was begun at three weeks after surgery and progressive forward ele- vation was added. When union was ensured, passive external rotation was recommended in cases with limitation of external rotation. Strengthening exercises were instituted in 14 patients who had good passive range of motion but showed limitation of the active range of motion after bony union. The patients were advised to avoid heavy manual work was avoided until solid bony union was confirmed. The implants were removed at about six months after surgery.
Fig. 1. (A) Initial anteroposterior view of a case of three-part fracture of the proximal humerus by Neer’s classification, with valgus impacted fracture pattern. There was valgus displacement of the humeral head at the surgical neck and displaced fracture of the greater tuberosity.
(B) Three-dimensional CT image. The lesser tuberosity remained with humeral head (black arrow). There was displaced fracture of the greater tuberosity which was fractured into two fragments (white arrows). (C) Anteroposterior view after retrograde tension band fixation. After reduc- tion, surgical neck was stabilized by three Steinmann pins (white arrow). The greater tuberosity was fixed by a tension band wire which was inserted through the rotator cuff and around the Steinmann pins (empty arrow). Additional tension band wire between the posterior cuff and anterior cuff was applied (arrowhead). (D) Anteroposterior view after implants removal. Solid bony union was accomplished in well reduced position.
A B C D
2. Assessment of results
The clinical function of the shoulder was assessed by the Neer scoring system18). The Neer score assigns the points for pain (35 points), range of motion (ROM) (30 points), activities of daily living (ADL) function (25 points) and, fracture position (10 points). The result is designated as excellent when the score is 90 or higher points, satisfactory when it is 80-89 points, unsat- isfactory when 70-79 points, and failure when below 70 points.
All patients were examined radiographycally. Radiographs were taken in the anteroposterior (AP) and axillary lateral views. Occur- rence of necrosis of the humeral head was checked (yes or no), and the quality of fracture reduction was evaluated by Zyto’s three- point graded scale (good, acceptable, poor)28).
RESULTS
Ninety percent (30 cases) achieved to excellent or satisfactory results. Overall, the mean score was 88.9 (66-100). The results were excellent in eighteen cases (56%), satisfactory in twelve cases (38%), unsatisfactory in one case (3%) and failure in one case (3%) with clinical evaluation. By radiological evaluation, there were twenty-one cases were good (66%) (Fig. 1C, D), nine cases (28%) were acceptable and two cases (6%) were poor. Unsatisfactory results (3 cases) were seen in the cases with pin migration, loss of reduction and avascular necrosis, respectively. All cases were united within three months. The three cases with unsatisfactory results also showed solid bony union even with the complications.
In the case with pin migration, the pins were removed at four months after surgery. At the last follow-up, the patient showed good functional recovery with solid bony union. A case of loss of reduction with unsatisfactory clinical result showed varus angu- lation with mild pain and some limitation of ADL. The patient did not want further procedure. A case with avascular necrosis showed mild pain and moderate limitation of shoulder motion.
Fortunately, this condition did not deteriorate over time. This patient also did not want further surgery. There was not a case of delayed union, nonunion or infection. Some tendency to under- correction was observed in the fracture with severe varus displace- ment (3 cases). However, there was hard to find any difference between the age, sex, dominancy of the hand and type of the frac- ture after retrograde pin fixation with tension band wiring.
DISCUSSION
There is no consensus concerning treatment in comminuted displaced fractures of the proximal humerus. Non-operative treat- ment7,27,28), osteosynthesis4,5,8,13,15-17,19,23), and primary implanta- tion of a prosthesis19)have been advocated. Neer19) recommend-
ed prosthetic replacement in displaced four part fractures and open reduction and internal fixation in three part fractures. In 1991, Jakob et al.9)described a group of four-part fractures with a good prognosis that showed the head fragment in a valgus impact- ed position and have recommended open reduction, minimal internal fixation and early exercise. As demonstrated by Lee and Hansen14), revascularization of the humeral head after total inter- ruption of the vascular supply occurs through the mechanism of creeping substitution. There has been a trend toward trial of open reduction and internal fixation3-6,12,14,16,23,25)in the treatment of three- or four-part fractures, especially in young patients.
Numerus fixation devices have been used, and the results of the different techniques have been reported in the literature2): Percutaneous pinning20), Rush nails16), wireloops15,19), T-plates8,13), semitubular blade plates17,23), modified cloverleaf plate4). Various fixation techniques described for proximal humeral fractures demonstrate that the optimal surgical procedure has not yet been developed. The goal of surgical therapy is to obtain acceptable reduction of fragments and stable fixation, to enable immediate rehabilitation. And surgical treatment should not lead to further devascularization of fracture fragments and an increased risk of avascular necrosis.
While plating has substantially improved the assurance of union and functional recovery, there is sometime interference with phys- iologic blood supply to the regions of the fracture and consequent- ly, to the biological elements of healing. Plates are usually quite bulky and may interfere with the delicate soft tissue coverage, as well as with function. And for correct placement, considerable exposure of bone is required22). The complications of the fixation with plate includ avascular necrosis secondary to extensive soft tissue dissection, impingement by a superiorly placed plate, loss of fixation with screw loosening, malunion, infection. Because many elderly people have osteopenia, plates and screws provide poor fixation for fractures of the upper humerus. Low incidence of avascular necrosis and nonunion has been reported after plate fixation with indirect reduction8). Hawkins et al.6)recommend operative treatment using tension band wiring for the healthy, active individual who has a three part fracture of the proximal part of the humerus. Tension band wiring intentionally incorpo- rates the healthy tissue of the rotator cuff as additional fixation.
In addition, the amount of soft tissue dissection required for ten- sion band wiring is usually less than that required with buttress plate, and this reduces the potential for avascular necrosis. Ten- sion band wiring is not technically overly demanding. Darder3) recommended antegrade intramedullary Kirschner wire and ten- sion band fixation in four part displaced fractures. Ruedi22)rec-
ommended an alternative method of treatment of proximal hu- meral fractures using screw and wiring systems. We thought that simple tension band wiring has disadvantage because of weakness in rotational stability. Antegrade insertion of the pin has disad- vantage of subacromial impingement by proximally protruded tip of the pin.
Majority of the proximal humeral fracture develop around the surgical neck of the proximal humerus. The rotator cuff muscles are the only muscles attached to the proximal fragment above the surgical neck. At the distal fragment below the surgical neck, extrinsic muscles including deltoid, latissimus dorsi and pectoralis major muscles are inserted. For stable fixation of the surgical neck, the forces of both groups muscles should be neutralized and trans- ferred to the opposite fragments. Furthermore, soft tissue should not be widely dissected to protect vascularity of the humeral head and to preserve osteogenetic potential at the fracture site. And there should be no protruded hard material in the subacromial space to avoid mechanical impingement. Low profile implant would be better for motion between deltoid muscle and subdel- toid structure. We thought that retrograde pin fixation with tension band wiring method would be one of good choice full- filling these criteria. In retrograde pin fixation and tension band wiring, two or three Steinmann pins are used to act as an inter- nal splint neutralizing rotational and angular displacement forces without oecupation of the subacromial space with implant. Addi- tional tension band wiring between the rotator cuff and the Stein- mann pins converts distractive and shearing forces into compres- sive forces across the fracture site11). The compressive forces pro- mote early fracture healing and the stable fixation also allows early mobilization and rehabilitation. In high surgical neck fracture, a technique of internal fixation with plate and screw is very dif- ficult to get stable fixation due to the small proximal fragment.
In high surgical neck fracture, the retrograde pin fixation with tension band wiring is more convenient and easier than any other procedure. Also it has advantages of minimizing soft tissue injury through blunt dissection of the deltopectoral interval, limited periosteal injury, indirect reduction and neutralization of the rota- tor cuff and major muscle forces. With modified tension band wiring and multiple pin fixation, there is less tissue dissection and consequently, less interference with the physiologic fracture healing process. By retrograde insertion of the Steinmann pins, it is possible to prevent the risk of subacromial impingement and it facilitate the rehabilitation. However, Steinmann pins may become loose and migrate. In that respect, screw fixation might be better than Steinmann pin to prevent pin migration. However, it is not always easy to insert screws in oblique direction. Stein-
mann pin can be inserted also in cases with relatively low surgical neck fracture. However, in very low surgical neck fracture, it may be difficult to insert pins obliquely with acute angle. In such cases, plate and screw would be a better choice because it would be easy to insert enough number of screws into the proximal fragment due to its large size. Fracture with severe varus displacement has a risk of collapse at the fracture site and occurrence of varus defor- mity. In fracture with severe varus displacement, it may be dif- ficult to maintain reduction with tension band wiring because the rigidity of fixation may not be enough to prevent loss of reduc- tion. For these cases, it would be better to control the proximal fragment directly, instead of indirect control through the rotator cuff. For these special cases, special implants should be developed in the future. Even with these limitations for special cases, the retrograde pin fixation with tension band wiring method could be applied for the majority cases in author’s hands, and the tech- nique showed a good functional recovery and clinical outcome in the majority of the cases of the proximal humeral fractures.
CONCLUSION
Retrograde pin fixation with tension band wiring for the prox- imal humeral fractures was considered to be a useful method, which is easy and induces limited soft tissue injury, and provides enough stability for postoperative rehabilitation in majority of cases such as surgical neck or three-part fractures.
REFERENCES
1. Baron JA, Karagas M, Barrett J, Kniffin W, Malenka D and Keller RG:Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology, 7: 612-618, 1996.
2. Chun JM, Groh GI and Rockwood CA Jr: Two part fractures of the proximal humerus. J Shoulder Elbow Surg, 3: 273-287, 1994.
3. Darder A, Darder A Jr, Sanchis V, Gastaldi E and Gomar F: Four part displaced proximal humeral fractures. Operative treatment using Kir- schner wires and a tension band. J Orthop Trauma 7: 497-505, 1993.
4. Esser RD: Open reduction and internal fixation of three and four part fractures of the proximal humerus. Clin Orthop Rel Res, 299: 244-251, 1994.
5. Gerber C, Hersche O and Berberat C: The clinical relevance of posttrau- matic avascular necrosis of the humeral head. J Shoulder Elbow Surg, 7: 586- 590, 1998.
6. Hawkins RJ, Bell RH and Gurr K: The three part fracture of the prox- imal part of the humerus. J Bone Joint Surg, 68-A: 1410-1414, 1986.
7. Hechmann T, Ochsner PE, Wingstrand H and Jonsson K: Non oper- ative treatment versus tension band osteosynthesis in three and four part proximal humeral farctures. International Orthop, 22: 316-320: 1998.
8. Hessmann M, Baumgaertel F, gehling H, Klingelhoeffer I and
Gotzen L:Plate fixation of proximal humeral fractures with indirect reduc- tion. Surgical technique and results utilizing three shoulder scores. Injury, 30: 453-462, 1999.
9. Jacob RP, Miniaci A, Anson PS, Jaberg H, Oslerwalder A and Ganz R:Four part valgus impacted fractures of the proximal humerus. J Bone Joint Surg, 73-B: 295-298, 1991.
10. Kim YK, Jang YH and Kim KB: Operative treatment of unstable frac- ture of the proximal humerus. J. of Korean Shoulder Elbow Society, 1: 198- 204, 1998.
11. Klinik H, Us AK and Mergen E: Self locking tension band technique.
Arch Orthop Trauma Surg, 119: 432-434, 1999.
12. Ko JY and Yamamoto R: Surgical treatment of complex fracture of the proximal humerus. Clin Orthop Rel Research, 327: 225-237, 1996.
13. Kristiansen B and Christensen SW: Plate fixation of proximal humer- al fractures. Acta Orthop Scand 57: 320, 1986.
14. Lee CK, Hansen HR and Weiss AB: Surgical treatment of the difficult humeral neck fracture acromial shortening anterloateral approach. J Trauma, 20: 67, 1980.
15. Lee CK and Hansen HR: Post traumatic avascular necrosis of the humer- al head in displaced proximal humeral farctures. J Trauma, 21: 788, 1981.
16. Lentz W and Meuser P: The treatment of fractures of the proximal hu- merus. Arch Orthop Trauma Surg, 96: 283, 1980.
17. Moda SK, Chadha NS, Sangwan SS, Khurana DK, Dahiya AS and Siwach RC:Open reduction and fixation of proximal humeral fractures and fracture dislocations. J Bone Joint Surg, 72-B: 1050-1052, 1990.
18. Neer C: Displaced proximal humerus fractures. J Bone Joint Surg, 52-A:
1077-1089, 1970.
19. Neer C: Displaced proximal humerus fractures. Part II. Treatment of three part and four part displacement. J Bone Joint Surg, 52-A: 1090-1103, 1970.
20. Park JY, Rho HJ and Kim MH: Percutaneous pinning in unstable two part fracture of surgical neck in humerus. J. of Korean Shoulder Elbow Society, 3: 26-32, 2000.
21. Rees J, Hicks J and Ribbans W: Assessment and management of three and four part proximal humearl fractures. Clin Orthop Rel Research, 353:
18-29, 1998.
22. Ruedi T: The treatment of displaced metaphyseal fractures with screws and wiring systems. Orthop 12: 55-59, 1989.
23. Sehr JR and Szabo RM: Semitubular blade plate for fixation of the prox- imal humerus. J Orthop Trauma, 2: 327, 1989.
24. Sturzenegger M, Fornaro E and Jakob RP: Results of surgical treat- ment of multifragmented fractures of the humeral head. Arch Orthop Trau- ma Surg, 100: 249-259, 1982.
25. Szyszkowitz R, Seggl W, Schleifer P and Cundy PJ: Proximal humer- al fractures. Management techniques and expected results. Clin Orthop, 292: 13-25, 1993.
26. Williams G Jr and Wong KL: Two part and three part fractures. Open reduction and internal fixation versus closed reduction and percutaneous pinning. Orthop Clin North Am, 31: 1-21, 2000.
27. Zyto K, Ahrengart L, Sperber A and Tornkvist H: Treatment of dis- placed proximal humeral farctures in elderly patients. J Bone Joint Surg, 79-B: 412-317, 1997.
28. Zyto K, Kronberg M and Brostrom LA: Shoulder function after dis- placed fractures of the proximal humerus. J Shoulder Elbow Surg, 4: 331- 336, 1995.
목 적 : 상완골 근위부 골절에 대해 역행적 강선 장력 대 고정의 수술적 치료를 시행한 후 결과를 알아보고, 그 수기를 소개하고자 하였다.
대상 및 방법 : 1996년 6월부터 2001년 6월까지 역행적 강선 장력 대 고정을 이용하여 상완골 근위부 골절을 수술한 후, 1년 이상 추시 관찰(평균 2.5 년: 1-5년)이 가능했던 32예를 대상으로 하였다. Neer의 분류상 2분 골절이 12예, 3분 골절이 20예이었으며, 수술 후의 평가는 Neer의 임상 평가법 및 Zyto의 방사선학적 평가법을 이용하여 분석하였다.
결 과 : 임상 평가 결과는 우수가 18예(56%), 만족이 12예(38%), 불만족이 1예(3%), 실패가 1예(3%)이었으며, 방사선 평가는 양호가 21예(66%), 보 통이 9예 (28%), 불량이 2예(6%)이었다. 불만족한 결과를 보인 예는 강선의 이동, 정복 유지의 실패, 상완골 두 괴사가 발생한 경우에 해당하였으며 지 연 유합이나 불유합, 감염 등의 합병증은 없었다.
결 론 : 역행적 강선 장력 대 고정을 이용한 상완골 근위부 골절의 수술은 연부 조직의 손상을 최소화하면서 비교적 견고한 고정을 얻을 수 있어 조기 에 견관절 운동이 가능하여 상완골의 외과적 경부 골절 및 3분 골절에 유용한 수술 방법 중의 하나라고 생각하였다.
색인 단어 : 견관절, 상완골 근위부 골절, 역행적 강선 장력 대 고정
상완골 근위부 골절의 역행적 강선 장력 대 고정
전재명ㆍ김성연*ㆍ이상원ㆍ김경환*ㆍ이종하*
울산대학교 의과대학 서울ㆍ강릉아산병원* 정형외과학교실