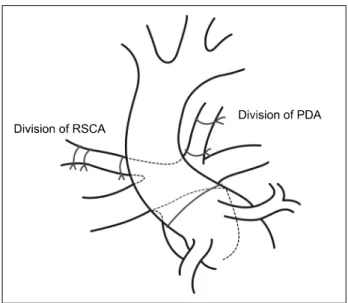
Anomalous Origin of the Right Subclavian Artery in a Patient with D-transposition of the Great Arteries
전체 글
수치
관련 문서
Kuwait will celebrate on Sunday the fourth anniversary of the UN honoring and proclamation of His Highness the Amir, Sheikh Sabah Al-Ahmad Al-Jaber Al-Sabah as
• 이명의 치료에 대한 매커니즘과 디지털 음향 기술에 대한 상업적으로의 급속한 발전으로 인해 치료 옵션은 증가했 지만, 선택 가이드 라인은 거의 없음.. •
If the total charge is zero, the dipole moment is independent of the choice of origin. Let’s displace the origin by
A source of light waves moving to the right with velocity 0.7c. The frequency is higher on the right, and lower
One might try to solve the problem by copying the first d elements of x to a temporary array, moving the remaining n − d elements left d places, and then copying the first d
The proposal of the cell theory as the birth of contemporary cell biology Microscopic studies of plant tissues by Schleiden and of animal tissues by Microscopic studies of
Since every classical or virtual knot is equivalent to the unknot via a sequence of the extended Reidmeister moves together with the forbidden moves, illustrated in Section 2,
웹 표준을 지원하는 플랫폼에서 큰 수정없이 실행 가능함 패키징을 통해 다양한 기기를 위한 앱을 작성할 수 있음 네이티브 앱과