저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다.
Doctoral Thesis in Medicine
The effect of comorbidities on the
initiation timing of dialysis
and patient survival
Graduate School of Ajou University
Department of Medicine
The effect of comorbidities on the
initiation timing of dialysis
and patient survival
Gyu-Tae Shin, Advisor
I submit this thesis as the
Doctoral thesis in Medicine.
February 2020
Graduate School of Ajou University
Department of Medicine
i
- ABSTRACT –
The effect of comorbidities on the initiation timing of
dialysis and patient survival
Rationale & Objective: The association of estimated glomerular filtration rate
(eGFR) at dialysis therapy initiation with mortality among dialysis patients has been greatly debated. However, we think it would be a reasonable idea to start dialysis early in high-risk patients with many comorbid conditions. We investigated predialysis comorbidities and adverse outcome preceding initiation of dialysis, and the association of predialysis comorbidities with estimated eGFR at dialysis initiation.
Study Design: Retrospective cohort study.
Setting & Participants: 1,038 incident dialysis patients who started maintenance
dialysis between January 2010 and December 2015. Patients were assessed for comorbidity indicies when eGFR was < 20 ml/min/1.73m2 and followed up until dialysis initiation.
Predictor: Khan, Davies, Charlson comorbidity index.
Outcomes: Predialysis adverse outcomes of cardiovascular event, infection
requiring hospitalization, and cerebrovascular event, death from any cause.
Analytical Approach: Comparisons of the comorbidity indicies and predialysis
adverse outcomes were done by Cox regression model. Post-dialysis mortality was assessed by Cox proportional hazards model.
ii
Results: During predialysis period, patients with higher comorbidities experienced
more cardiovascular adverse outcome such as myocardial infarction or angina, and more infection event requiring hospitalization. Cox regression resulted hazard ratio (HR) of each risk groups to predialysis cardiovascular adverse events as follows: medium risk, 4.36 (95% Confidence Interval (C.I.) 1.71 – 11.14); high risk, 8.84 (95% C.I. 3.06 – 25.55), respectively (p < 0.001). After adjustment of age, sex, eGFR at dialysis initiation, and comorbidity index, HR for death after dialysis initiation in urgent group when compared with the planned dialysis group was 1.45 (95% C.I. 1.04-2.02, p = 0.029).
Limitations: Single-center retrospective observational cohort study; Possible
residual confounding; Insufficient death data.
Conclusions: Patients with larger comorbidities experienced more adverse events
during pre-RRT periods. Dialysis start should be individualized considering the comorbid conditions.
Keywords: Dialysis initiation; estimated glomerular filtration rate (eGFR);
iii
Table of Contents
Abstract ……….. i List of Figures ……… iv List of Tables ……….. iv List of Text I. Introduction ……….… 1 II. Methods ………..… 3 A. Study populations ……….. 3 B. Comorbidity indicies ………. 4C. Definition of planned dialysis and urgent dialysis ………. 5
D. Statistical analysis ………. 6 III. Results ……….. 7 IV. Discussion ……….……… 9 References ………..…………. 13 Figures ………. 15 Tables ………... 18 국문요약 …..……….... 25
iv
List of Figures
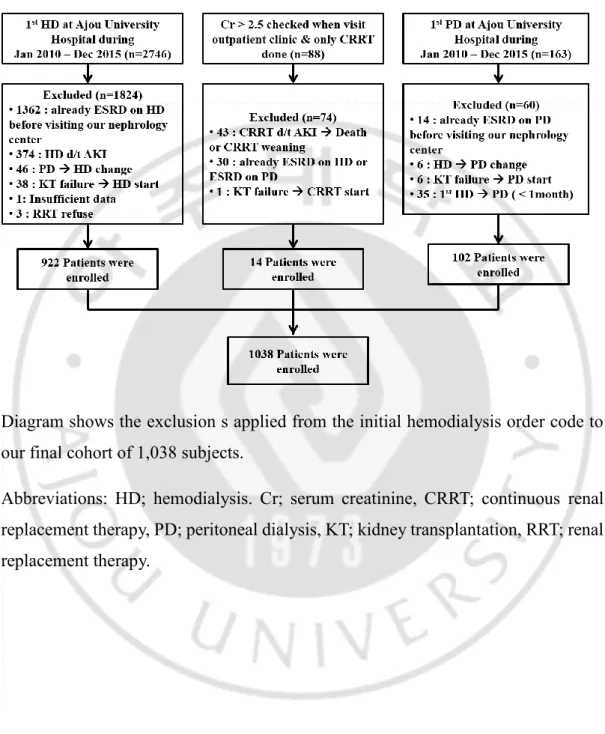
▶ Figure 1. Patients flow diagram
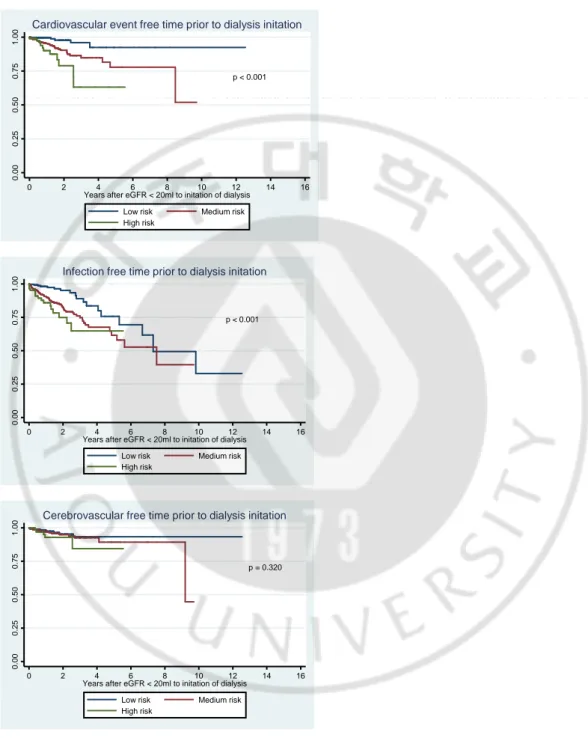
▶ Figure 2. Predialysis adverse outcome according to comorbidity indices
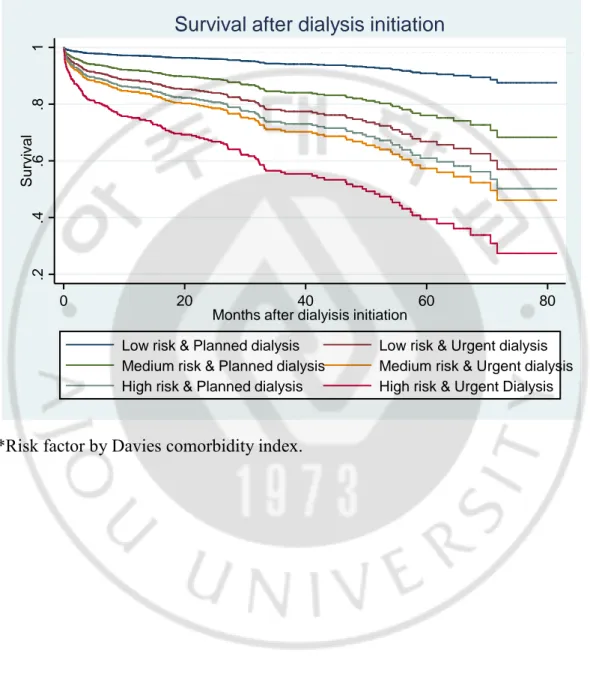
▶ Figure 3. Kaplan-Meier survival curves for comparisons of survival by comorbidity indices and urgency
List of Tables
▶ Table 1. Baseline characteristics of patients.
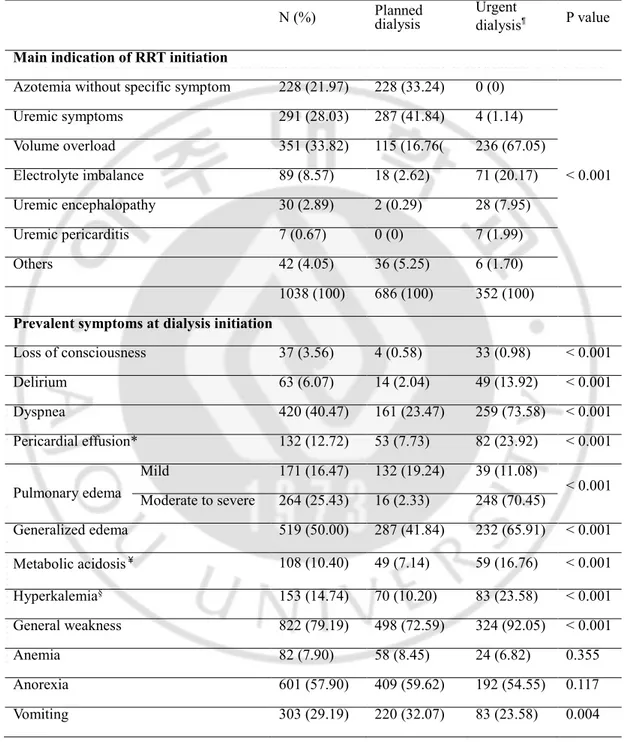
▶ Table 2. Main indication and prevalent symptoms at RRT initiation.
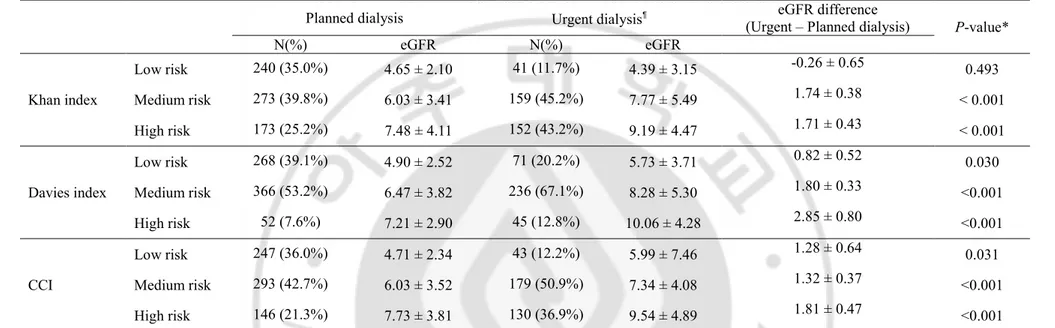
▶ Table 3. Estimaed GFR at RRT intiation according to comorbidity index.
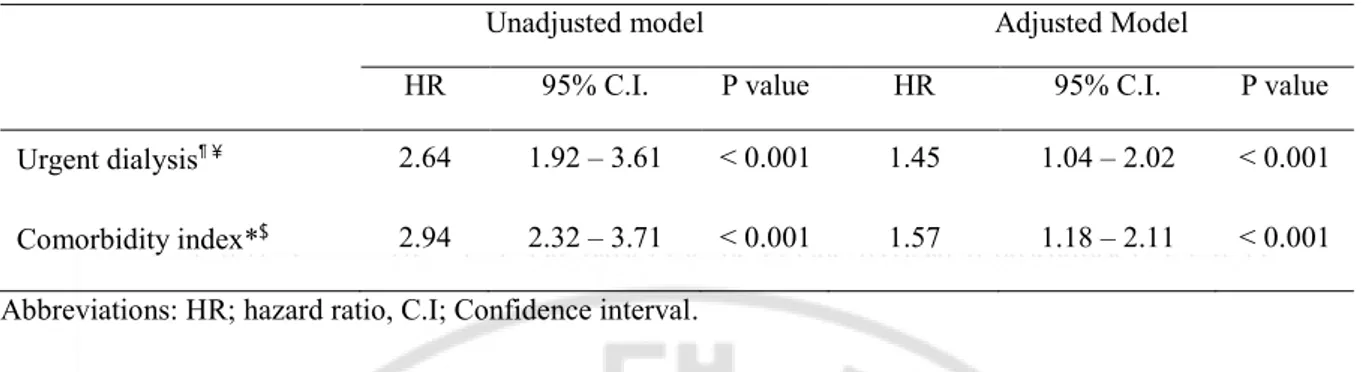
▶ Table 4. Assessment of mortality after dialysis initiation by using Cox regression proportional analysis.
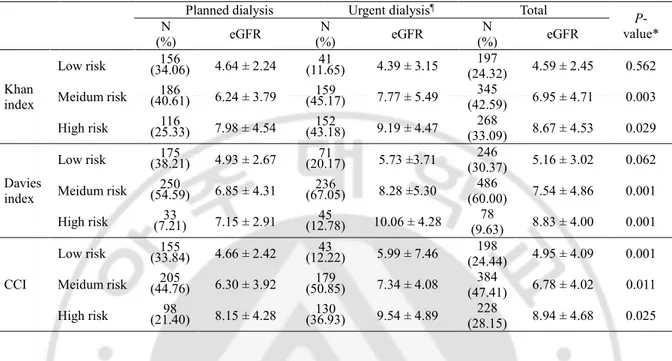
▶ Table S1. Estimaed GFR at dialysis initiation according to comorbidity index in symptomatic patient at dialysis initiation (N=810)
1
I. INTRODUCTION
The number of end-stage renal disease (ESRD) patients requiring dialysis treatment has been continuously and rapidly increasing over the past few decades1-4. Nevertheless, optimal level of estimated glomerular filtration rate (eGFR) to start renal replacement therapy (RRT) is still controversial. In the 1990s, nephrologists believed that early initiation of dialysis could improve patient survival. Several observational cohort and case-control studies have suggested that starting dialysis early may improve patients' survival, quality of life, and capacity for employment and decrease complications5, 6. Recently, several observational studies have shown that initiation of RRT at high eGFR was associated with poorer post-RRT patient survival7-12. And the Initiating Dialysis Early and Late (IDEAL) study, the only randomized trial in Australia and New Zealand to have tested the impact of dialysis initiation at two different levels of kidney function on outcomes, showed planned early initiation of dialysis in patient with stage V chronic kidney disease was not associated with an improvement in survival or clinical outcomes13. ‘Early’ at these studies, it is based on only the eGFR. The decision to start dialysis is generally guided by the measures of renal function, most often eGFR from serum creatinine, but clinical data such as uremic symptoms, signs of protein–energy wasting or fluid overload are also considered. In real clinical practice, timing of RRT initiation are thought be individualized considering the burden of comorbid conditions. European Best Practice Guidelines (EBPG) do not advocate using a certain threshold of eGFR, but rather encourage the use of clinical parameters (nutrition, electrolytes and volume status)14.
Few studies of predialysis morbidity have so far done among the previous studies about the timing of dialysis initiation. We hypothesis that dialysis should be initiated
2
at the higher eGFR if the patents with many comorbid conditions. Therefore, we retrospectively investigated predialysis comorbidities and adverse outcomes preceding initiation of dialysis as clinical outcomes and the association of comorbidities with eGFR at dialysis initiation.
3
II. METHODS
We performed a retrospective cohort study at Ajou University Medical Center (AUMC). We enrolled patients 18 years of age or older at the dialysis initiation with progressive chronic kidney disease. The study was approved by the ethics committee of the Ajou University School of Medicine (AJIRB-MED-MDB-15-514).
Study populations
We received the list of patients receiving the first order of hemodialysis in AUMC from electronic medical chart and reviewed all of them. A total of 2,746 patients received conventional hemodialysis for the first time at AUMC between January 2010 and December 2015. Of these, 1,362 patients were excluded because they had started hemodialysis previously in other centers. Other excluded patients were 347 who received hemodialysis for management of acute kidney injury, 46 who switched to hemodialysis from peritoneal dialysis, 38 who returned to hemodialysis following renal allograft failure, 1 who had insufficient data on electrical medical record (EMR), and 3 who refused RRT (only prescription and not hemodialysis performed). Therefore, of the 2,746 patients, 922 patients had started maintenance hemodialysis for management of ESRD between January 2010 and December 2015. Out of these 922 patients, 26 patients were preemptive cases with brief hemodialysis immediately before kidney transplantation. We enrolled 14 patients who had been followed up at the outpatient clinic due to chronic kidney disease and started RRT using continuous renal replacement therapy (CRRT) but died before switching conventional hemodialysis. These patients included only those with ESRD who were considering dialysis initiation during outpatient follow-up, and acute kidney injury on chronic
4
kidney disease patients were excluded. During six years, 102 patients had started peritoneal dialysis for management of ESRD. Finally, including hemodialysis, CRRT and peritoneal dialysis, medical records of 1,038 incident dialysis patients who started maintenance dialysis between January 2010 and December 2015 were reviewed. This process for constructing the retrospective cohort is summarized in Fig.1.
Demographic, laboratory and clinical information was collected. The presence of comorbid illness was assessed at the enrolled time by complete review of the patients’ inpatient and outpatient record (containing information about medical and surgical consultations and previous hospital admission). The eGFR was calculated using the Modification of Diet in Renal Disease study equation15. The enrolled time was defined as the first time of estimated glomerular filtration below 20ml/min/1.73m2. From the enrolled time to dialysis initiation, we reviewed predialysis adverse outcome, such as cardiovascular events (nonfatal myocardial infarction, new onset angina requiring percutaneous intervention), nonfatal stroke, transient ischemic attack, infection requiring hospitalization. Early referral and late referral were defined according whether the patient’s first encounter with a nephrologist was more than or less than 3 months prior to the RRT initiation. Body mass index (BMI) was categorized according to World Health Organization classification for Asian population16. Mortality data was obtained from the time of dialysis initiation until December 2017.
Comorbidity indicies
5
ischemic heart disease (stable angina, unstable angina and myocardial infarction), peripheral vascular disease, cerebrovascular disease, liver cirrhosis (compensated, decompensated), chronic obstructive pulmonary disease, malignancy, AIDS, neuromuscular disease and collagen disorder. The Khan17, Davies18, and Charlson comorbidity indices (CCI)19 were calculated for each patient based on the comorbidities at the enrolled time. The Khan index is a combination of age and comorbidities, used to assign patients to one of three risk groups; low, medium, and high risk17. The Davies score is based on the presence or absence of seven comorbid conditions, also producing three risk groups18. Age is not included in this index. Patients without comorbid conditions are classified as low risk. Patients with one or two comorbid diseases are regarded as medium-risk patients. Patients with three or more comorbid conditions are classified as high-risk patients. The Charlson index is based on weights for each comorbidity and age class19. To be able to compare Charlson index with the Khan and Davies indicies, patients were categorized as low-risk (Charlson score ≤ 3), medium low-risk (Charlson score 4-5) and high low-risk (Charlson score ≥ 6) groups, based on tertile limits20.
Definition of planned dialysis and urgent dialysis
Patients were classified as planned dialysis group vs. urgent dialysis group. Urgent dialysis group was defined as the patients who started maintenance dialysis from urgent indication such as uremic encephalopathy, uremic pericarditis, pulmonary edema, or serum potassium more than 7.0 mEq/L. Patients who showed pulmonary edema on chest X-ray with their clinical course that were consistent with pulmonary edema were included urgent dialysis group. Planned dialysis group was defined as the remaining cases where there were no urgent RRT due to the safe initiation of
6
dialysis.
Statistical analysis
Summaries of continuous variables are presented as means (± SD) for normally distributed data categorical variables are presented as frequencies (percentages). Continuous variables were compared with the use of Student’s t-test, the Mann-Whitney test or one way ANOVA (for non-normally distributed data), and categorical data with the use of chi-square tests.
Multivariable logistic regression was used to assess risk factors associated with urgent dialysis initiation. Comparisons of the comorbidity indicies and predialysis morbidities between the planned dialysis group and the urgent dialysis group were done. We used a time-to-event analysis to compare the proportions of patients with clinical outcomes in the two groups. Kaplan-Meier (KM) plots were used to visualize the association of comorbidities with predialysis complications, such as cardiovascular event, infection event, and cerebrovascular event. Significance was calculated by log-rank test. We used the Cox proportional hazards model to assess the factor that is associated with the end point of death from any cause.
All reported P values are two-tailed, with a P value of 0.05 indicating statistical significance. Analyses were performed with the use of Stata software, version 15.0 (Stata Corporation, College Station, TX, USA).
7
III. RESULTS
Between Jan 2010 and Dec 2015, a total 1,038 patients were enrolled for final analysis, and Figure 1 shows the details of the patients. Table 1 shows the baseline characteristics of patients. Among total 1,038 patients, female was 461 (44.4%). Mean age at dilaysis initiation was 58.6 ± 14.8 years old. BMI was 23.1 ± 3.6 kg/m2. Mean eGFR at the enrolled time was 14.07 ± 5.93 ml/min/1.73m2 and mean eGFR at dialysis initiation was 6.62 ± 4.15 ml/min/1.73m2. Proportion of early referral was 84.2%. Common comorbidities at the enrolled time includes diabetes (53.7 %), hypertension (87.7 %), previous myocardial infarction (5.5 %), previous angina s/p (status post) stent insertion (7.7 %), heart failure (8.9 %), and previous cerebrovascular disease (12.4 %). In the urgent group, cardiovascular disease, such as MI and angina, heart failure, and peripheral arterial obstructive disease were more prevalent. The past history of chronic obstructive pulmonary disease, malignancy, neuromuscular disease and collagen disease did not differ between the two groups. Urgent dialysis group was 352 out of 1038, or 34 % and older than planned dialysis group (p < 0.001). Mean eGFR at dialysis initiation in the urgent dialysis group was higher than those of the planned dialysis group (7.99 ± 5.05 ml/min/1.73m2 vs. 5.91 ± 3.40 ml/min/1.73m2, p < 0.001). Table 2 shows in detail the main indications of dialysis and what prevalent symptoms were at the start of dialysis. In the table S1, the changes of eGFR at start of dialysis according to the comorbidity index were shown, except for the asymptomatic patients who started dialysis with progressive azotemia without specific symptoms. Logistic regression analysis showed that age at enrolled time (OR 1.034, 95% C.I. [1.023-1.045]), DM (OR 1.942, 95% C.I [1.442-2.614]), HF (OR 2.812, C.I. [1.701–4.624]), and PAOD (OR 2.216, 95% C.I. [1.124-4.366]) were independent risk factors in urgent dialysis group.
8
Urgent dialysis group had higher comorbidity indicies than safe dialysis group. And, the higher comorbidity indices, the higher eGFR at the initiation of dialysis (Table 3,
p < 0.001). In addition, eGFR at dialysis initiation was higher in urgent dialysis group
than in planned dialysis group at all comorbidity indicies. The difference in eGFR at the start of dialysis increased as the comorbid condition becomes higher risk. When the predialysis period from enroll time to dialysis initiation was reviewed, patients with higher comorbidities experienced more cardiovascular adverse outcomes such as myocardial infarction or angina, and more infection events requiring hospitalization (Figure 2). Cox regression resulted hazard ratio of each risk groups to predialysis cardiovascular adverse events as follows: medium risk, 4.36 (95% Confidence Interval (C.I.) 1.71 – 11.14); high risk, 8.84 (95% C.I. 3.06 – 25.55), respectively (log rank test: p < 0.001). The hazard ratio of each risk groups to predialysis infection events were as follows: medium risk, 2.57 (95% C.I. 1.51 – 4.37); high risk, 3.85 (95% C.I. 1.94 – 7.68), respectively (log rank test: p < 0.001). The hazard ratio of each risk groups to predialysis cerebrovascular events were as follows: medium risk, 0.85 (95% C.I. 0.36 – 1.99); high risk, 1.04 (95% C.I. 0.36 – 1.99), respectively (log rank test: p = 0.320).
Figure 3 shows the results of survival after dialysis initiation by comorbidity indicies and urgency.
After adjustment for age, sex, eGFR at dialysis initiation, and comorbidity indicies, hazard ration (HR) for death after dialysis initiation in the urgent dialysis group when compared with the planned dialysis group was 1.45 (95% C.I. 1.04-2.02, p < 0.001) (Table 4). After adjustment for age, sex, eGFR at dialysis initiation, and urgent dialysis initiation, there was significant increase the risk of death as the higher comorbidity index increased (HR 1.57, 95% C.I. 1.18-2.11, p < 0.001) (Table 4).
9
IV. DISCUSSION
In present study, we found that patients with higher comorbidities experienced more cardiovascular adverse outcome such as myocardial infarction or angina, and more infection event requiring hospitalization during predialysis period. And we could confirm that the urgent RRT itself increases the mortality after dialysis even if such comorbidities are statistically corrected.
Early dialysis initiation (at an eGFR > 10 mL/min/1.73 m2) has not been associated with a morbidity and mortality benefit, as shown in the IDEAL study13. This observational study influenced the development of the most recent European guidelines on the timing of dialysis initiation21, which place greater emphasis on the assessment of patients’ symptoms and signs rather than eGFR. It is suggested that in asymptomatic patients with stage V chronic kidney disease, dialysis may be safely delayed until the eGFR is at least as low as 5–7 mL/min/1.73 m2 if there is careful clinical follow-up and adequate patient education. In our study, mean eGFR at RRT initiation of 1,038 patients was 6.62 ± 4.15 ml/min/1.73m2. This results support that with careful clinical management of chronic kidney disease, dialysis can be delayed for some patients until the GFR drops below 7.0 ml/ min/1.73m2. The eGFR at dialysis initiation in our study was very low value when compared with 12.0 ml/min/1.73m2 in the early start group and 9.8 ml/min/1.73m2 in the late start group as shown in the IDEAL study.
However, advanced chronic kidney disease patients with a higher comorbidity burden may require early dialysis. In our study, the eGFR at dialysis initiation in the urgent dialysis group was 7.99 ± 5.05 ml/min/1.73m2, and the eGFR at dialysis initiation in the safe dialysis group was 5.91 ± 3.40 ml/min/1.73m2 (p < 0.001). So, if we know what comorbidities make start dialysis with high eGFR, the dialysis can
10
be prepared in advance for patient with this comorbidities. As shown previously, cardiovascular disease, such as MI and angina, heart failure, and PAOD were more prevalent in the urgent group. In our study, urgent dialysis were associated with a significantly increased risk of death after adjustment for comorbidities. In other words, planned dialysis itself has a protective effect on survival. So, patients with these comorbidities need to be prepared in advance to be able to initiate dialysis at higher eGFR to perform early planned dialysis initiation. As Table 3 shown, the higher comorbidity indicies, the greater the difference in eGFR at dialysis initiation between planned dialysis group and urgent dialysis group. Therefore, patients with many comorbidities, the nephrologist should be alert early. In addition, as shown in Table 2 and Table S1, symptoms related to volume overload occurred frequently in urgent patients. Therefore, it is important to emphasize the importance of low salt diet education and proper use of diuretics for volume control, especially in high risk patients.
Cardiovascular disease is common in advanced chronic kidney disease and ESRD. Actually, cardiovascular disease accounts for approximately 50% of deaths among dialysis patients22. Clinical data are limited and do not clearly clarify the association between predialysis nephrology care and cardiovascular outcomes in patients with ESRD. A recently published study suggested that early nephrology referral did not improve cardiovascular outcomes in dialysis patients23. Yet another studies revealed that frequent predialysis nephrology visits are associated with fewer composite major adverse cardiac events (MACEs)24, 25. Management of diverse potential interventions by nephrologists, including improved management of blood pressure, volume overload, hyperkalemia, anemia, acid-base disturbances, and nutritional deficiencies, may be expected to improve cardiovascular outcomes26.
11
Infection may be another important complication of chronic kidney disease. In our study, more infection events requiring hospitalization occurred in the patients with higher comorbidity scores during predialysis period. About fifty years ago, it was assumed that general debility from chronic uremia increased the risk of infection. And, it was postulated that reversal of the uremic state would reduce the risk of infection27. Unfortunately, RRT has not reduced the problem of infection28. ESRD may be considered a state of acquired immunodeficiency29. Increased risk for hospitalization with infection has also been observed among individuals with less severely decreased kidney function that does not require dialysis30-32. Some investigators have indicated that there may be a link between infectious events, which increase inflammatory mediators, and subsequent cardiovascular events, including myocardial infarction and congestive heart failure33.
Our study has several limitations. First, this study was a retrospective, single center study of tertiary university hospital and the results cannot be generalized. And, the classification of comorbidities for each patient was determined by clinical impression (based on documentation in electronic records). This introduces the possibility for misclassification bias. Second, as in previous studies7-10, our study have been based on registry data by patients who survived to initiate dialysis therapy. RRT prevalence is used as surrogate estimate for ESRD prevalence, although this approach ignores patients receiving conservative care. Therefore, the patients with ESRD who might have experienced premature death from in adequate RRT accessibility were not analyzed in our study. Third, there was a lot of missing data of death event after dialysis initiation and long-term follow-up data. Since our hospital is a tertiary university hospital, many patients have moved to outside dialysis clinic after dialysis initiation. In our study, urgent dialysis initiation, high comorbidity score were significantly associated with an increased risk of death in a Cox model
12
after adjustment. However, this death result has a limitation due to insufficient data. Fourth, in Figures 2 and 3, there was a significant overlap between the planned dialysis group at high risk and the urgent dialysis group at medium risk, indicating that comorbidity modeling is not sophisticated. Fifth, alertly early dialysis initiation with many comorbidities could reduce predialysis adverse outcomes, but it is unknown whether patients survival after dialysis initiation will improve. However, planned early dialysis is expected to reduce the events during the transition period immediately before and after dialysis.
In spite of these limitations, our study has provided several clinically relevant points. Because of the precise chart review, not the registry data, our data is reliable and valuable. We investigated predialysis morbidities and adverse clinical outcomes preceding initiation of dialysis. Also, we investigated the association of comorbidities with eGFR at dialysis initiation. There was no previous study of predialysis adverse events of advanced chronic kidney disease patients.
Our study provides important information for decision making in advanced chronic kidney disease patients starting dialysis. Patients with larger comorbidities experienced more adverse events during predialysis periods. Especially, in high risk patients with a history of HF, MI, and PAOD, early planned dialysis should be considered.
Supplementary Material
Table S1: Estimaed GFR at dialysis intiation according to comorbidity index in symptomatic patient at dialysis initiation (N=810)
13
References
1. Liyanage T, Ninomiya T, Jha V, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385(9981): 1975-1982.
2. McCullough KP, Morgenstern H, Saran R, Herman WH, Robinson BM. Projecting ESRD Incidence and Prevalence in the United States through 2030. J Am Soc Nephrol. 2019;30(1): 127-135.
3. Jin DC, Yun SR, Lee SW, et al. Lessons from 30 years' data of Korean end-stage renal disease registry, 1985-2015. Kidney Res Clin Pract. 2015;34(3): 132-139.
4. Jin DC, Yun SR, Lee SW, et al. Current characteristics of dialysis therapy in Korea: 2016 registry data focusing on diabetic patients. Kidney Res Clin Pract. 2018;37(1): 20-29. 5. Tattersall J, Greenwood R, Farrington K. Urea kinetics and when to commence dialysis. Am
J Nephrol. 1995;15(4): 283-289.
6. Termorshuizen F, Dekker FW, van Manen JG, et al. Relative contribution of residual renal function and different measures of adequacy to survival in hemodialysis patients: an analysis of the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD)-2. J Am Soc Nephrol. 2004;15(4): 1061-1070.
7. Stel VS, Dekker FW, Ansell D, et al. Residual renal function at the start of dialysis and clinical outcomes. Nephrol Dial Transplant. 2009;24(10): 3175-3182.
8. Lassalle M, Labeeuw M, Frimat L, et al. Age and comorbidity may explain the paradoxical association of an early dialysis start with poor survival. Kidney Int. 2010;77(8): 700-707. 9. Kazmi WH, Gilbertson DT, Obrador GT, et al. Effect of comorbidity on the increased
mortality associated with early initiation of dialysis. Am J Kidney Dis. 2005;46(5): 887-896. 10. Evans M, Tettamanti G, Nyren O, Bellocco R, Fored CM, Elinder CG. No survival benefit from early-start dialysis in a population-based, inception cohort study of Swedish patients with chronic kidney disease. J Intern Med. 2011;269(3): 289-298.
11. Winnicki E, Johansen KL, Cabana MD, et al. Higher eGFR at Dialysis Initiation Is Not Associated with a Survival Benefit in Children. J Am Soc Nephrol. 2019;30(8): 1505-1513. 12. Susantitaphong P, Altamimi S, Ashkar M, et al. GFR at initiation of dialysis and mortality in
CKD: a meta-analysis. Am J Kidney Dis. 2012;59(6): 829-840.
13. Cooper BA, Branley P, Bulfone L, et al. A randomized, controlled trial of early versus late initiation of dialysis. N Engl J Med. 2010;363(7): 609-619.
14. European Best Practice Guidelines Expert Group on Hemodialysis ERA. Section I. Measurement of renal function, when to refer and when to start dialysis. Nephrol Dial Transplant. 2002;17 Suppl 7: 7-15.
15. Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145(4): 247-254.
16. Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403): 157-163. 17. Khan IH, Catto GR, Edward N, Fleming LW, Henderson IS, MacLeod AM. Influence of
coexisting disease on survival on renal-replacement therapy. Lancet. 1993;341(8842): 415-418.
14
patients and its relationship to other predictors of survival. Nephrol Dial Transplant. 2002;17(6): 1085-1092.
19. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5): 373-383.
20. Van Manen JG, Korevaar JC, Dekker FW, et al. Adjustment for comorbidity in studies on health status in ESRD patients: which comorbidity index to use? J Am Soc Nephrol. 2003;14(2): 478-485.
21. Tattersall J, Dekker F, Heimburger O, et al. When to start dialysis: updated guidance following publication of the Initiating Dialysis Early and Late (IDEAL) study. Nephrol Dial Transplant. 2011;26(7): 2082-2086.
22. Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2017 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis. 2018;71(3S1): A7. 23. Hayashi T, Kimura T, Yasuda K, et al. Early Nephrology Referral 6 Months Before Dialysis Initiation Can Reduce Early Death But Does Not Improve Long-Term Cardiovascular Outcome on Dialysis. Circ J. 2016;80(4): 1008-1016.
24. Huang CY, Hsu CW, Chuang CR, Lee CC. Pre-Dialysis Visits to a Nephrology Department and Major Cardiovascular Events in Patients Undergoing Dialysis. PLoS One. 2016;11(2): e0147508.
25. Yang JY, Huang JW, Chen L, et al. Frequency of Early Predialysis Nephrology Care and Postdialysis Cardiovascular Events. Am J Kidney Dis. 2017;70(2): 164-172.
26. Hundemer GL, Sood MM. Predialysis Care and Cardiovascular Outcomes: Why the Lead Up to Dialysis Matters. Kidney Int Rep. 2019;4(5): 635-637.
27. Montgomerie JZ, Kalmanson GM, Guze LB. Renal failure and infection. Medicine (Baltimore). 1968;47(1): 1-32.
28. Sarnak MJ, Jaber BL. Mortality caused by sepsis in patients with end-stage renal disease compared with the general population. Kidney Int. 2000;58(4): 1758-1764.
29. Vanholder R, Ringoir S. Infectious morbidity and defects of phagocytic function in end-stage renal disease: a review. J Am Soc Nephrol. 1993;3(9): 1541-1554.
30. Dalrymple LS, Katz R, Kestenbaum B, et al. The risk of infection-related hospitalization with decreased kidney function. Am J Kidney Dis. 2012;59(3): 356-363.
31. James MT, Quan H, Tonelli M, et al. CKD and risk of hospitalization and death with pneumonia. Am J Kidney Dis. 2009;54(1): 24-32.
32. Ishigami J, Grams ME, Chang AR, Carrero JJ, Coresh J, Matsushita K. CKD and Risk for Hospitalization With Infection: The Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis. 2017;69(6): 752-761.
33. Cheikh Hassan HI, Tang M, Djurdjev O, Langsford D, Sood MM, Levin A. Infection in advanced chronic kidney disease leads to increased risk of cardiovascular events, end-stage kidney disease and mortality. Kidney Int. 2016;90(4): 897-904.
15
Figure 1. Patients flow diagram.
Diagram shows the exclusion s applied from the initial hemodialysis order code to our final cohort of 1,038 subjects.
Abbreviations: HD; hemodialysis. Cr; serum creatinine, CRRT; continuous renal replacement therapy, PD; peritoneal dialysis, KT; kidney transplantation, RRT; renal replacement therapy.
16
Figure 2. Predialysis adverse outcome according to comorbidity indices*.
*Risk factor by Davies comorbidity index.
p < 0.001 0 .0 0 0 .2 5 0 .5 0 0 .7 5 1 .0 0 0 2 4 6 8 10 12 14 16
Years after eGFR < 20ml to initation of dialysis
Low risk Medium risk
High risk
Cardiovascular event free time prior to dialysis initation
p < 0.001 0 .0 0 0 .2 5 0 .5 0 0 .7 5 1 .0 0 0 2 4 6 8 10 12 14 16
Years after eGFR < 20ml to initation of dialysis
Low risk Medium risk
High risk
Infection free time prior to dialysis initation
p = 0.320 0 .0 0 0 .2 5 0 .5 0 0 .7 5 1 .0 0 0 2 4 6 8 10 12 14 16
Years after eGFR < 20ml to initation of dialysis Low risk Medium risk High risk
17
Figure 3. Kaplan-Meier survival curves for comparisons of survival by comorbidity indices* and urgency.
*Risk factor by Davies comorbidity index.
.2 .4 .6 .8 1 S u rv iv a l 0 20 40 60 80
Months after dialyisis initiation
Low risk & Planned dialysis Low risk & Urgent dialysis Medium risk & Planned dialysis Medium risk & Urgent dialysis High risk & Planned dialysis High risk & Urgent Dialysis
18
Table 1. Baseline characteristics of patients.
Total Planned dialysis Urgent dialysis¶ P value
Number (%) 1038 (100) 686 (66) 352 (34) Male, n(%) 577 (55.6) 383(55.7) 195 (55.4) 0.930 Age (years) 58.6 ± 14.8 56.1 ± 14.6 63.8 ± 13.8 <0.001 BMI (kg/m2) 23.1 ± 3.6 23.0 ± 3.5 23.3 ± 4.0 0.316 Follow Up Days* 434.1 ± 557.2 462.7 ± 581.9 378.4 ± 501.8 0.021 DM, n(%) 557 (53.7) 325 (47.2) 235 (66.2) <0.001 DM duration (years) 8.82 ± 10.5 7.33 ± 9.81 11.7 ± 11.06 <0.001 Use of Insulin, n(%) 251 (24.2) 143 (20.8) 108 (30.7) 0.006 HTN, n(%) 910 (87.7) 600 (87.5) 310 (88.1) 0.779 HTN Duration (years) 8.97 ± 9.73 8.11 ± 7.59 10.61 ± 8.46 <0.001 Modality (HD : PD) 936: 102 590 : 96 346 : 6 <0.001 Temporary catheter insertion 769 (74.1) 448 (65.3) 321 (91.2) <0.001 eGFR(ml/min/1.73m2) at enrolled time 14.07 ± 5.93 13.92 ± 5.97 14.36 ± 5.84 0.257 eGFR(ml/min/1.73m2) at dialysis initiation 6.62 ± 4.15 5.91 ± 3.40 7.99 ± 5.05 <0.001 Comorbidities at enrolled time
Cancer 93 (8.96) 58 (8.45) 35 (9.95) 0.474
19
Note: Values for categorical variables are given as number (percentage); values for continuous variables, as mean ± standard deviation.
Abbreviations: BMI; body mass index, DM; diabetes mellitus, HTN; hypertension, HD; hemodialysis, PD; peritoneal dialysis, eGFR; estimated glomerular filtration rate.
¶Urgent dialysis: Urgent dialysis group was defined as the patients who started maintenance dialysis
from urgent indication such as uremic encephalopathy, uremic pericarditis, pulmonary edema, or serum potassium more than 7.0 mEq/L.
*Follow Up Days: from the enrolled time to dialysis initiation
CVA 129 (12.43) 78 (11.37) 51 (14.49) 0.182 COPD 11 (1.06) 5 (0.73) 6 (1.69) 0.146 MI 57 (5.49) 29 (4.23) 28 (7.95) 0.013 Angina 80 (7.71) 41 (5.98) 39 (11.10) 0.011 HF 92 (8.86) 35 (5.10) 57 (16.19) 0.000 PAOD 41 (3.95) 16 (2.33) 25 (7.10) 0.001 NMD 1 (0.10) 1 (0.15) 0 (0.00) 0.474 Collagen disease 22 (2.12) 16 (2.33) 6 (1.70) 0.506
20
Table 2. Main indication and prevalent symptoms at RRT initiation.
N (%) Planned dialysis Urgent dialysis¶ P value
Main indication of RRT initiation
Azotemia without specific symptom 228 (21.97) 228 (33.24) 0 (0)
< 0.001 Uremic symptoms 291 (28.03) 287 (41.84) 4 (1.14) Volume overload 351 (33.82) 115 (16.76( 236 (67.05) Electrolyte imbalance 89 (8.57) 18 (2.62) 71 (20.17) Uremic encephalopathy 30 (2.89) 2 (0.29) 28 (7.95) Uremic pericarditis 7 (0.67) 0 (0) 7 (1.99) Others 42 (4.05) 36 (5.25) 6 (1.70) 1038 (100) 686 (100) 352 (100) Prevalent symptoms at dialysis initiation
Loss of consciousness 37 (3.56) 4 (0.58) 33 (0.98) < 0.001 Delirium 63 (6.07) 14 (2.04) 49 (13.92) < 0.001 Dyspnea 420 (40.47) 161 (23.47) 259 (73.58) < 0.001 Pericardial effusion* 132 (12.72) 53 (7.73) 82 (23.92) < 0.001 Pulmonary edema Mild 171 (16.47) 132 (19.24) 39 (11.08) < 0.001 Moderate to severe 264 (25.43) 16 (2.33) 248 (70.45) Generalized edema 519 (50.00) 287 (41.84) 232 (65.91) < 0.001 Metabolic acidosis¥ 108 (10.40) 49 (7.14) 59 (16.76) < 0.001 Hyperkalemia§ 153 (14.74) 70 (10.20) 83 (23.58) < 0.001 General weakness 822 (79.19) 498 (72.59) 324 (92.05) < 0.001 Anemia 82 (7.90) 58 (8.45) 24 (6.82) 0.355 Anorexia 601 (57.90) 409 (59.62) 192 (54.55) 0.117 Vomiting 303 (29.19) 220 (32.07) 83 (23.58) 0.004
21
¶Urgent dialysis: Urgent dialysis group was defined as the patients who started maintenance dialysis
from urgent indication such as uremic encephalopathy, uremic pericarditis, pulmonary edema, or serum potassium more than 7.0 mEq/L.
*Pericardial effusion is confirmed by echocardiogram and/or computed tomography.
¥Metabolic acidosis was defined as serum bicarbonate below 10mEq/L.
§Hyperkalemia was defined as when serum potassium was greater than 6mEq/L.
General ache 37 (3.56) 23 (3.35) 14 (3.98) 0.607 Pruritus 49 (4.72) 35 (5.10) 14 (3.98) 0.419 Insomonia 47 (4.53) 33 (4.81) 14 (3.98) 0.541 Neuropathy 89 (8.57) 64 (9.33) 25 (7.10) 0.225 No symptoms 69 (6.65) 68 (9.91) 1 (0.28) < 0.001 Systemic infection 40 (3.85) 15 (2.19) 25 (7.10) < 0.001
22
Table 3. Estimaed GFR at RRT intiation according to comorbidity index.
Planned dialysis Urgent dialysis¶ eGFR difference
(Urgent – Planned dialysis) P-value*
N(%) eGFR N(%) eGFR Khan index Low risk 240 (35.0%) 4.65 ± 2.10 41 (11.7%) 4.39 ± 3.15 -0.26 ± 0.65 0.493 Medium risk 273 (39.8%) 6.03 ± 3.41 159 (45.2%) 7.77 ± 5.49 1.74 ± 0.38 < 0.001 High risk 173 (25.2%) 7.48 ± 4.11 152 (43.2%) 9.19 ± 4.47 1.71 ± 0.43 < 0.001 Davies index Low risk 268 (39.1%) 4.90 ± 2.52 71 (20.2%) 5.73 ± 3.71 0.82 ± 0.52 0.030 Medium risk 366 (53.2%) 6.47 ± 3.82 236 (67.1%) 8.28 ± 5.30 1.80 ± 0.33 <0.001 High risk 52 (7.6%) 7.21 ± 2.90 45 (12.8%) 10.06 ± 4.28 2.85 ± 0.80 <0.001 CCI Low risk 247 (36.0%) 4.71 ± 2.34 43 (12.2%) 5.99 ± 7.46 1.28 ± 0.64 0.031 Medium risk 293 (42.7%) 6.03 ± 3.52 179 (50.9%) 7.34 ± 4.08 1.32 ± 0.37 <0.001 High risk 146 (21.3%) 7.73 ± 3.81 130 (36.9%) 9.54 ± 4.89 1.81 ± 0.47 <0.001
Note: Values for categorical variables are given as number (percentage); values for continuous variables, as mean ± standard deviation. Values for differences, as contrast ± standard error.
Abbreviations: CCI; Charlson comorbidity index, eGFR; estimated glomerular filtration rate.
¶Urgent dialysis: Urgent dialysis group was defined as the patients who started maintenance dialysis from urgent indication such as uremic encephalopathy, uremic
pericarditis, pulmonary edema, or serum potassium more than 7.0 mEq/L
23
Table 4. Assessment of mortality after dialysis initiation by using Cox regression proportional analysis.
Unadjusted model Adjusted Model
HR 95% C.I. P value HR 95% C.I. P value
Urgent dialysis¶¥ 2.64 1.92 – 3.61 < 0.001 1.45 1.04 – 2.02 < 0.001
Comorbidity index*$ 2.94 2.32 – 3.71 < 0.001 1.57 1.18 – 2.11 < 0.001
Abbreviations: HR; hazard ratio, C.I; Confidence interval.
¶Urgent dialysis: Urgent dialysis group was defined as the patients who started maintenance dialysis from urgent
indication such as uremic encephalopathy, uremic pericarditis, pulmonary edema, or serum potassium more than 7.0 mEq/L.
*Comorbidity index is used for CCI and is divided into low, medium and high risk.
¥Adjustment for sex, age at dialysis initiation, charlson comorbidity scores, and eGFR at dialysis initiation.
24
Supplementary Material
Table S1. Estimaed GFR at dialysis initiation according to comorbidity index in symptomatic patient at dialysis initiation (N=810).
Planned dialysis Urgent dialysis¶ Total
P-value* N
(%) eGFR (%) N eGFR (%) N eGFR Khan index Low risk (34.06) 156 4.64 ± 2.24 (11.65) 41 4.39 ± 3.15 (24.32) 197 4.59 ± 2.45 0.562 Meidum risk (40.61) 186 6.24 ± 3.79 (45.17) 159 7.77 ± 5.49 (42.59) 345 6.95 ± 4.71 0.003 High risk (25.33) 116 7.98 ± 4.54 (43.18) 152 9.19 ± 4.47 (33.09) 268 8.67 ± 4.53 0.029 Davies index Low risk (38.21) 175 4.93 ± 2.67 (20.17) 71 5.73 ±3.71 (30.37) 246 5.16 ± 3.02 0.062 Meidum risk (54.59) 250 6.85 ± 4.31 (67.05) 236 8.28 ±5.30 (60.00) 486 7.54 ± 4.86 0.001 High risk (7.21) 33 7.15 ± 2.91 (12.78) 45 10.06 ± 4.28 (9.63) 78 8.83 ± 4.00 0.001 CCI Low risk (33.84) 155 4.66 ± 2.42 (12.22) 43 5.99 ± 7.46 (24.44) 198 4.95 ± 4.09 0.001 Meidum risk (44.76) 205 6.30 ± 3.92 (50.85) 179 7.34 ± 4.08 (47.41) 384 6.78 ± 4.02 0.011 High risk (21.40) 98 8.15 ± 4.28 (36.93) 130 9.54 ± 4.89 (28.15) 228 8.94 ± 4.68 0.025
¶Urgent dialysis: Urgent dialysis group was defined as the patients who started maintenance dialysis from urgent
indication such as uremic encephalopathy, uremic pericarditis, pulmonary edema, or serum potassium more than 7.0 mEq/L.
25 - 국문요약 – 만성콩팥병 환자에서 투석치료 시작시점과 환자 생존율에 미치는 동반질환의 영향 아주대학교 대학원 의학과 이 민 정 (지도교수 : 신 규 태) 투석 개시 시점에서의 사구체여과율과 투석 환자 사망률의 연관성에 대해서는 여 전히 논의의 여지가 있다. 그러나 저자들은 많은 동반 질환이 있는 고위험 만성 콩팥병 환자에게서는 조기에 투석을 시작하는 것이 합리적이라고 생각한다. 따라 서 만성콩팥병 추적 당시의 동반 질환과 추적기간동안 투석 전 발생하는 여러가 지 합병증, 그리고 투석 시작 시점에서의 사구체여과율과의 연관성에 대하여 분 석하였다. 본 연구는 후향적 코호트 분석 연구로, 2010년 1월부터 2015년 12월 사이에 유 지투석을 시작한 1,038명의 투석환자를 대상으로 하며, 만성콩팥병 환자의 추적 기간 중, 계산된 사구체여과율 20ml/min/1.73m2 미만시부터 동반 질환을 평가 하고, 투석 개시까지 추적관찰 하였다. 응급으로 투석을 시작하게 되는 환자들의 경우 투석 개시 시점의 사구체여과율은 계획된 투석 환자들보다 높았다(7.99 ± 5.05 ml/min/1.73m2 vs. 5.91 ± 3.40 ml/ min/1.73m2, p <0.001). 투석 전 추적기간동안, 동반 질환이 높은 환자는 심근
26 경색 또는 협심증과 같은 심혈관계 부작용이 더 많이 발생하였으며, 입원이 필요 한 감염 사례가 더 많았다. 특히, 과거 병력상 심부전, 금성심근경색의 병력 및 말초동맥폐색질환의 병력이 있는 고위험 만성콩팥병 환자의 경우, 투석 개시 시 점까지의 추적기간도중 심혈관계 부작용이 많이 발생하였다. 또한, 이러한 동반 질환들을 통계적으로 보정하더라도, 응급으로 투석을 시작하게 되는 경우에는 투 석 후 사망률을 증가시킨다는 것을 확인할 수 있었다 (Hazard ratio 1.45, 95% 신뢰구간 1.04-2.02, p < 0.001). 즉, 계획된 투석 그 자체가 투석 후 사망률을 감소시키는 효과가 있음을 알 수 있었다. 본 연구는 투석을 시작하는 진행된 만 성콩팥병 환자에 있어, 심부전, 급성심근경색 및 말초동맥폐색질환의 병력이 있는 고위험 환자군의 경우, 투석 전 기간동안 더 면밀한 관찰이 필요하며, 조기 투석 을 고려해야한다는 정보를 제공한다. 본 연구가 투석을 시작하는 진행된 만성신 부전 환자의 투석 개시 시점에 중요한 정보가 되길 기대한다.