Effects of Breathing Maneuver and Sitting
Posture on Muscle Activity in Inspiratory
Accessory Muscles in Patients With Chronic
Obstructive Pulmonary Disease
The Graduate School
Yonsei University
Department of Physical Therapy
Kisong Kim
Effects of Breathing Maneuver and Sitting
Posture on Muscle Activity in Inspiratory
Accessory Muscles in Patients With Chronic
Obstructive Pulmonary Disease
The Graduate School
Yonsei University
Department of Physical Therapy
Kisong Kim
Effects of Breathing Maneuver and Sitting
Posture on Muscle Activity in Inspiratory
Accessory Muscles in Patients With Chronic
Obstructive Pulmonary Disease
Kisong Kim
A Dissertation
Submitted to the Department of Physical Therapy
and the Graduate School of Yonsei University
in partial fulfillment of the
requirements for the degree of
This certifies that the doctoral dissertation of
Kisong Kim is approved.
Thesis Supervisor: Chunghwi Yi
Sanghyun Cho: Thesis Committee Member #1
Ohyun Kwon: Thesis Committee Member #2
Heonseock Cynn: Thesis Committee Member #3
Hyeseon Jeon: Thesis Committee Member #4
The Graduate School
Acknowledgements
First of all, I would like to express my gratitude to God. He always loves and leads me to the right way, and I am very glad for his guidance and support that has enabled me to finish this dissertation. I want to share this pleasure with my lovely father and mother, father in law and mother in law, son and daughter, and other family members. They strongly supported and believed in me when I was frustrated and fatigued. I can never thank them enough for their endless support.
I sincerely thank Professor Chunghwi Yi for his guidance and support. He has been an excellent supervisor of my research who always showed me the highest scholarship, and has nourished my professional knowledge in physical therapy. I also deeply thank Professor Ohyun Kwon for sincere advice that improved the quality of this dissertation. He has demonstrated the deepest insight for developing research ideas and has facilitated my passion for learning physical therapy. Professor Heonseock Cynn provided warm guidance and valuable experience for the dissertation. He enriched my academic and clinical knowledge in physical therapy. I would also like to deeply thank Professor Sanghyun Cho, Professor Hyeseon Jeon, and Professor Sunghyun You for providing encouragement and helping to expand my professional knowledge in subjects with scientific essay, English presentation, motor control and problem solving with evidence based.
I also express my sincerest thanks to my wife, who encouraged me from the depth of her heart and supported me throughout the study period of my dissertation. Many friends made my life at graduate school very happy. I also thank all the physical therapists, Manager Jaeyong Ryu, Chief Hyunmo Goo, Chief Kyuwan Lee, and another all members of the Department of Physical Therapy and Professor Seongwoong Gang, Professor Yoonghil Park, Junghyun Park, and all staffs of Yonsei University, College of Medicine, Gangnam Severance Hospital, for their intellectual support and guidance. I pray to God for their happiness and health.
Table of Contents
List of Figures ··· iii
List of Tables ··· iv Abstract ··· v Introduction ··· 1 Method ··· 3 1. Subjects ··· 3 2. Instruments ··· 5 3. Measurement ··· 6
3.1 Tidal Volume and Respiratory Rate ··· 6
3.2 Muscle Activity ··· 6
4. Procedure··· 7
4.1 Breathing Training ··· 7
4.2 Neutral Position ··· 7
4.3 With Arm Support in a Forward–Leaning Position ··· 7
4.4 With Arm and Head Support in a forward–Leaning Position ··· 8
5. Statistical Analysis ··· 9
Results ··· 10
1. Tidal Volume and Respiratory Rate ··· 10
Discussion ··· 15
Conclusion ··· 21
References ··· 22
List of Figures
Figure 1. Embla N7000 ··· 5 Figure 2. Sitting postures of NP, WAS, and WAHS ··· 8 Figure 3. Comparisons of %RVC among sitting postures ··· 14
List of Tables
Table 1. Subject demographic characteristics and pulmonary functions ··· 4 Table 2. Tidal volume, respiratory rate and muscle activity for each respiratory
ABSTRACT
Effects of Breathing Maneuver and Sitting Posture on
Muscle Activity in Inspiratory Accessory Muscles in
Patients With Chronic Obstructive Pulmonary Disease
Kisong Kim
Dept. of Physical Therapy The Graduate School Yonsei University
The present study was performed to determine the influence of breathing maneuver and sitting posture on tidal volume (TV), respiratory rate (RR), and muscle activity of the inspiratory accessory muscles in patients with chronic obstructive pulmonary disease (COPD).
Twelve men diagnosed with COPD participated in this study. Inductive respiratory plethysmography and surface EMG were used to simultaneously measure TV, RR, and muscle activity of inspiratory accessory muscles, i.e., the scalenus (SM), sternocleidomastoid (SCM), and pectoralis major (PM) muscles, during quiet natural breathing (QB) and pursed-lips breathing (PLB) in three sitting postures: neutral position (NP), with arm support (WAS) in a forward–leaning position, and with arm and head support (WAHS) in a forward–leaning position.
Two–way repeated-measures analysis of variance was employed. In a comparison of breathing patterns, PLB significantly increased TV and decreased RR compared with QB. Muscle activity in the SM and SCM increased significantly in PLB compared with QB. In a comparison of sitting postures, the muscle activity of the SM, SCM, and PM increased in the forward–leaning position.
The results suggest that in COPD, PLB induced a favorable breathing pattern (increased TV and reduced RR) compared with QB. Additionally, WAS and WAHS positions induced increased muscle activity of the inspiratory accessory muscles during inspiration versus NP. Differential involvement of accessory respiratory muscles can be readily studied in COPD patients, allowing monitoring of respiratory load during pulmonary rehabilitation.
Key Words: Chronic obstructive pulmonary disease, Forward–leaning position, Inspiratory accessory muscles, Pursed–lips breathing, Quiet natural breathing, Sitting postures.
Introduction
Breathing training (Gosselink 2004) and a sitting posture with a forward–leaning trunk (Sharp et al. 1980) have been advocated as therapeutic interventions in patients with chronic obstructive pulmonary disease (COPD) to relieve dyspnea and improve pulmonary function. Previous studies suggested that pursed–lips breathing (PLB) increased tidal volume (TV) (Petty, and Guthrie 1971) and reduced respiratory rate (RR) (Jones et al. 2003) in patients with COPD. Additionally, PLB was shown to lead to increased rib cage movement and accessory muscle recruitment during inspiration and expiration in patients with COPD (Breslin 1992).
Relief from dyspnea is often experienced in patients with COPD by assuming a forward–leaning position (Sharp et al. 1980). Sitting with a forward–leaning trunk and resting the forearms on the thighs is a modified position for relaxation in chest physical therapy (Bhatt et al. 2009; Brannon et al. 1993; Kisner, and Colby 1996; Shaffer et al. 1981; Simpson 1983). A previous study indicated increased end– expiratory level and active expiration in sitting with a forward–leaning trunk compared with sitting leaning back (Willeput, and Sergysels 1991). In addition to the forward–leaning position, placing the head and neck in proper alignment can reduce airway obstruction, helping to increase pulmonary function (Landers 2006).
However, the effects of a forward–leaning position on inspiratory muscle activity remain unclear. A previous study showed decreased activity of the SM and SCM in a
forward–leaning position (Sharp et al. 1980). In contrast, another study indicated that a forward–leaning position WAS support allowed accessory muscles (i.e., the pectoralis minor and major) to contribute significantly to rib cage elevation, and arm and head support contribute to inspiration in the forward–leaning position (Gosselink 2004). Based on these differing results in previous studies, there is no consensus with respect to the muscle activity of the inspiratory accessory muscles in the forward-leaning position.
Thus, this study was performed to compare the TV, RR, and activity of respiratory accessory muscles during quiet natural breathing (QB) and PLB in three different sitting positions: a neutral position (NP), with arm support (WAS) in a forward– leaning position, and with arm and head support (WAHS) in a forward–leaning position in patients with COPD.
Method
1. Subjects
Twelve male subjects (age = 68.2 ± 8.2 years; weight = 60.4 ± 6.9
㎏
; height = 1.7 ± 0.4 m; body mass index = 21.3 ± 2.0㎏/㎡
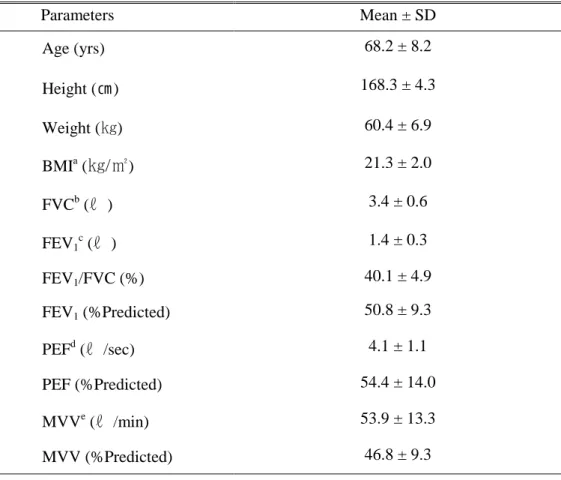
) diagnosed with COPD were recruited from the Division of Pulmonary Medicine, Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Yonsei University Health System, Seoul, Korea. All subjects were classified as stage 2 or 3 COPD (forced expiratory volume in 1 s percent predicted = 50.8 ± 9.3) by the GOLD criteria (Rabe et al. 2007). The demographic characteristics and pulmonary functions of subjects are presented in Table 1. All subjects provided written informed consent. This study was approved by the Yonsei University Wonju Campus Human Studies Committee.Table 1. Subject demographic characteristics and pulmonary functions (N=12) Parameters Mean ± SD Age (yrs) 68.2 ± 8.2 Height (㎝) 168.3 ± 4.3 Weight (㎏) 60.4 ± 6.9 BMIa (
㎏/㎡
) 21.3 ± 2.0 FVCb (ℓ
) 3.4 ± 0.6 FEV1 c (ℓ
) 1.4 ± 0.3 FEV1/FVC (%) 40.1 ± 4.9 FEV1 (%Predicted) 50.8 ± 9.3 PEFd (ℓ
/sec) 4.1 ± 1.1 PEF (%Predicted) 54.4 ± 14.0 MVVe (ℓ
/min) 53.9 ± 13.3 MVV (%Predicted) 46.8 ± 9.3 aBMI: Body mass index.
b
FVC: Forced vital capacity.
c
FEV1: Forced expiratory volume in 1 second. d
PEF: Peak expiratory flow.
e
2. Instruments
Inductive respiratory plethysmography and surface EMG were performed using an Embla N7000 (Embla Systems, Broomfield, CO) to enable the simultaneous acquisition and recording of respiratory parameters and surface electromyographic measurements (Figure 1). A two–band inductive respiratory plethysmography system consisting of surface electromyographic electrodes were attached to the patient to measure pulmonary function, and muscle activity.
3. Measurement
3.1 Tidal Volume and Respiratory Rate
TV and RR were measured by inductive respiratory plethysmography (Embla N7000; Embla Systems). The system consisted of two bands (Teflon–coated inductance) that measured changes in the cross-sectional area of the rib cage and abdomen, allowing determination of the respiratory phase (inspiration and expiration).
3.2 Muscle activity
For surface EMG, three pairs of Ag/AgCl electrodes and a reference electrode were affixed on the patient’s inspiratory accessory muscles, the scalene muscle (SM), sternocleidomastoid muscle (SCM), and pectoralis major (PM). The EMG unit of the Embla N7000 was used to measure the muscle activity of the inspiratory accessory muscles. Data are expressed as percentages of the reference voluntary contraction (%RVC). Muscle activity was measured during the inspiration phase. The inspiration phase was determined from the nasal pressure curve, measured using a nasal cannula and respiratory analysis software for inductive respiratory plethysmography, and Origin 8, a program that calculates the root mean square (OriginLab, Northampton, MA).
4. Procedure
4.1 Breathing Training
Prior to enrollment in the study, all subjects received a training session for PLB as suggested by Faling (1986). For the QB maneuver, patients were instructed to breath in their normal habitual comfortable breathing style (Bianchi et al. 2007) with no specific training. Breathing maneuvers and sitting postures to be tested were selected by randomized ballots to eliminate any possible test order effect. All subjects felt relaxed and comfortable after a familiarization period of 5 min.
4.2 Neutral Position
The sitting postures were described in Figure 2. NP breathing training was in a vertical sitting position with hands on thighs. The subject assumed a sitting posture maintaining bilateral hip, knee, and ankle joint angles of 90°.
4.3 With Arm Support in a Forward-Leaning Position
The subject assumed a sitting posture maintaining bilateral hip, knee, and ankle joint angles of 90°. Both elbows and forearms rested on the anterior thighs by leaning the trunk forward. An imaginary line connecting the tragus and hip joint should make an angle of 45° relative to the vertical. The head and cervical spine were aligned
comfortably with the trunk. The subject was asked to stabilize the gaze by looking at a predetermined dot 1m in front of the subject.
4.4 With Arm and Head Support in a Forward-Leaning Position
The WAHS position was identical to the WAS position except that the chin was held with both cupped hands. This standardized experimental position was practiced with verbal and tactile cues.
Figure 2. Sitting postures of NP, WAS, and WAHS.
a
NP: Neutral position.
b
WAHS: Breathing training With Arm and Head Support (WAHS).
c
5. Statistical Analysis
The Statistical package for the Social Science for Windows version 18.0 (SPSS, Inc., Chicago, IL, USA) was used for statistical analyses. Two–way (2 × 3) analysis of variance with repeated measures was employed for comparing the two breathing maneuvers (QB, PLB) and three different positions (NP position, WAS position, WAHS position). In the case of significant differences between test positions, Bonferroni’s post hoc test was performed. In all analyses, p-values<0.05 were deemed to indicate statistical significance.
Results
1. Tidal Volume and Respiratory Rate
The mean and standard deviation of TV and RR for each respiratory maneuver and sitting posture are presented in Table 2. For TV, there was no interaction between breathing pattern and position (F=0.13, p=0.88). There was a significant main effect of breathing method (F=90.02, p<0.01), but there was no significant main effect of position (F=0.84, p=0.45). TV in PLB was significantly greater than that in QB. For RR, there was no interaction between breathing pattern and position (F=1.46, p=0.25). There was a significant main effect of breathing method (F=50.70, p<0.01), but there was no significant main effect of position (F=1.39, p=0.27). RR in PLB was significantly lower than that in QB.
2. Muscle Activity
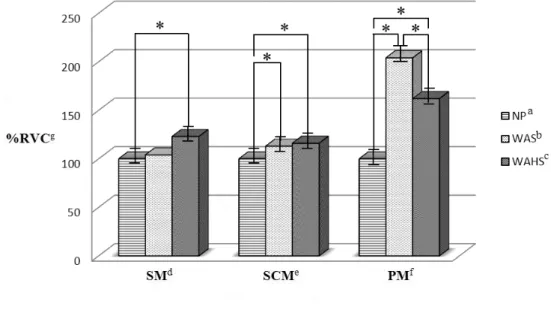
The mean and standard deviation of %RVC for each respiratory maneuver and sitting posture are presented in Table 2. Comparisons of %RVC among sitting postures are presented in Figure 3. For SM activity, there was no interaction between breathing pattern and position (F=0.83, p=0.45). However, there were significant main effects of breathing method (F=19.55, p=0.01) and position (F=7.47, p=0.01). Muscle activity in PLB was significantly greater than that in QB. Bonferroni’s post
hoc test showed that the muscle activity in WAHS was increased significantly
compared with that in NP (p=0.02). Muscle activity was not significantly different between WAHS and WAS (p=0.07) or between WAS and NP (p=0.50). For SCM activity, there was no interaction between breathing pattern and position (F=0.65,
p=0.53), but significant main effects of breathing method (F=5.75, p=0.04) and
position (F=24.12, p<0.01) were observed. Muscle activity in PLB was significantly greater than that in QB. Bonferroni’s post hoc test showed that the muscle activity in WAHS was increased significantly compared with that in NP (p=0.01), and the muscle activity in WAS was increased significantly compared with that in NP (p<0.01). No significant difference in muscle activity between WAHS and WAS (p=0.15) was observed. For PM muscle activity, the results showed no interaction between breathing pattern and position (F=1.14, p=0.36) and no significant main
effect of breathing method (F=3.94, p=0.07), but a significant main effect of position (F=4.66, p=0.04) was observed. Bonferroni’s post hoc test showed significant muscle activity differences among the three sitting positions used in this study. Muscle activity in WAS was increased significantly compared with that in NP (p=0.03) and in WAHS (p=0.03). Muscle activity in WAHS was increased significantly compared with that in NP (p= 0.04).
a NP : N eut ral posi tion . b WAS : B rea thi ng t rai ni ng W ith A rm S uppor t ( WAS ). c WAH S : B rea thi ng t rai ni ng W ith A rm and H ea d S uppor t ( WAH S). d TV : T idal vol um e. e Mean ± SD f RR : R es pi rat or y r at e . g SM : S ca lene m usc le . h % R V C : P er ce nt age of r ef er enc e vol unt ar y cont rac tion . i SC M : S ter nocl ei dom as toi d m usc le . j PM : P ec tor al is m aj or m usc le. PM j ( % R V C ) SC M i ( % R V C ) SM g ( % R V C h ) RR f ( f/ m in) TV d (ℓ) par am et er s Tabl e 2 . Tida l vol um e, r es pi rat or y r at e a nd m usc le a ct ivi ty f or ea ch r es pi rat or y m ane uver and s itt ing post ur e (N =12) 100.0 ± .0 100.0 ± .0 100.0 ± .0 18.1 ± 3.0 0.7 ± 0.2 e NP a Q ui et N at ur al B rea thi ng 204.0 ± 89.0 113.1 ± 12.4 104.4 ± 35.1 16.7 ± 3.4 0.8 ± 0.2 WAS b 161.2 ± 78.1 115.6 ± 13.7 123.4 ± 25.2 16.5 ± 2.1 0.8 ± 0.3 WAH S c 113.6 ± 20.5 115.8 ± 17.0 118.4 ± 17.7 12.0 ± 0.6 1.3 ± 0.1 NP Purs ed -Lips B rea thi ng 271.1 ± 214.6 12 2.9 ± 24.0 134.6 ± 31.2 12.0 ± 1.1 1.3 ± 0.2 WAS 167.0 ± 69.2 131.0 ± 24.0 150.1 ± 45.3 12.0 ± 0.9 1.3 ± 0.2 WAH S
Figure 3. Comparisons of %RVC among sitting postures. (*p<0.05)
a
NP: Neutral position.
b
WAHS: Breathing training With Arm and Head Support (WAHS).
c
WAS: Breathing training With Arm Support (WAS).
d
SM: Scalene muscle.
e
SCM: Sternocleidomastoid muscle.
f
PM: Pectoralis major muscle.
g
Discussion
The findings of this study showed that TV was significantly greater in PLB than in QB and that RR was significantly lower in PLB than in QB, supporting the research hypothesis. These results are consistent with previous studies indicating beneficial effects of PLB compared with QB for increasing TV (Petty, and Guthrie 1971) and decreasing RR (Jones et al. 2003; Breslin 1992).
The increased TV during PLB was probably due largely to the increased pressure in extra–thoracic airways and thus to a reduced cost of breathing due to decreased intrinsic positive end–expiratory pressure (PEEP). Many patients with COPD use PLB in an attempt to produce extrinsic PEEP to reduce lung hyperinflation and dyspnea (Martin, and Davenport 2011). The increased TV observed in our study may be explained by a recent study that described that deflation of the abdomen and inflation of the rib cage contributed to increased TV of the chest wall during PLB (Bianchi et al. 2007). However, dyspnea scores in relation to postural changes and breathing maneuver were not measured in this study. A recent report showed that PLB slowed RR and increased TV both at rest and during exercise in COPD subjects; no subject complained of dyspnea at rest or during controlled exercise at 60% of maximum exercise workload. However, dyspnea scores were increased with PLB in four of the eight COPD patients. (Spahija et al. 2005). PLB had no effect on minute ventilation, increased muscle activity of the abdominal muscles, and had a variable
effect on dyspnea during volitional exercise in that study. Some studies have indicated that expiratory muscle recruitment has been associated with a worsening of dyspnea (O‘Donnell et al. 1988; Petrof et al. 1990). In the present study, no subject had received treatment with PLB or had used PLB voluntarily prior to entry into this study. No patient complained of any increasing sense of dyspnea in each experimental trial because all subjects had a familiarization period with PLB and posture assumption before enrollment.
The diaphragm contains three types of muscular fibers (types I, IIA, and IIB/X), and
the types of fibers vary in function with aging, type of exercise, and chronic respiratory load in patients with COPD (Papavramidis et al. 2011). A shift in diaphragmatic muscle fiber type toward slow–twitch, oxidative type I fibers, which are more fatigue–resistant, increases endurance, whereas protein degradation and a significant reduction in myosin content decreases muscular force–generating capacity (Klimathianaki et al. 2011). Pulmonary hyperinflation shortens and flattens the diaphragm, altering the length of the diaphragm muscle fibers as well as their strength (Serres et al. 1998). Concomitantly, the capacity of the diaphragmatic muscle to generate optimal pressure is decreased due to the mechanical disadvantage in the length–tension relationship caused by hyperinflation (Klimathianaki et al. 2011).
Although there was no complaint of dyspnea during quiet breathing in this study, the effect of PLB for relief of dyspnea could not be explained because we collected
in TV and RR during PLB could not be shown to explain the positive effect in relief of dyspnea because of the limited data in our study, PLB is likely to reduce diaphragm activity and consequently may help to protect from fatigue of the diaphragmatic muscles during increased ventilatory conditions in patients with COPD (Breslin 1992; Puhan 2007; Miravittles 2006).
In contrast to PLB, TV and RR did not differ significantly with sitting position. Thus, the research hypothesis regarding breathing position was not supported by the results of this study. These findings are consistent with a recent study by Bhatt et al. (2009), who found no significant differences in FEV1, the ratio of forced expiratory
volume to forced vital capacity (FEV1/FVC), maximum inspiratory pressure (MIP),
maximal expiratory pressure (MEP), diaphragmatic movements during tidal breathing, or forced breathing in the sitting, supine, or sitting leaning forward with the hands supported on the knees (tripod position) in patients with COPD. Kera and Maruyama (2005) reported that TV did not change significantly according to sitting positions in 15 young adult men.
Posture can influence the degree of limitation on expiratory tidal flow according to changes in functional residual capacity (FRC) (Agostoni, and Hyatt 1986). Recent studies described that slumped sitting decreases TV, FVC, FEV1, and peak expiratory
flow compared with upright postures (Landers et al. 2003; Lin et al. 2006). Another recent study reported that the effect of postural changes on respiratory movements of the chest wall had not been specifically addressed, and reported that single plane changes in sitting posture altered three–dimensional ribcage configuration and chest
wall kinematics in seven healthy subjects during breathing while maintaining constant respiratory function (Lee et al. 2010).
Patients with severe COPD frequently lean forward, bracing their arms. A position bracing the elbows on a table increased ventilatory capacity significantly in four healthy men, and this effect could be helpful information for COPD patients, whose diaphragms are flattened and ineffective, as such patients depend more on the inspiratory muscles of the rib cage (Banzett 1988). In contrast, bracing the arms impaired the function of the inspiratory muscles and reduced ribcage stability in six normal subjects, and these negative effects could not explain the improved capacity to sustain hyperpnea when the arms are braced (Prandi et al. 1999).
Because the muscular force–generating capacity of the diaphragm is decreased in COPD and the effects of elbow bracing differed between the past studies, in the present study, we focused on changes in inspiratory accessory muscle activity related to changes in posture with or without elbow bracing to identify postural effects.
Although both the WAS and WAHS postures, characterized by the trunk leaning forward, might increase intra–abdominal pressure and decrease diaphragmatic excursion toward the abdominal cavity during inspiration, many patients with COPD adopt on a sitting posture with the trunk forward leaning during conditions of an increasing sense of dyspnea (Bhatt et al. 2009; Neumann 2009), and athletic runners stand with the trunk forward, leaning, with hands on knees after finishing races to lessen ventilatory demand. Many researchers would like to identify sitting postures
TV and RR did not differ significantly in relation to sitting position in this study. We had no data on inspiratory duty cycle or FRC according to different sitting posture; thus, our results do not provide complete information about postural changes in lung volumes.
The muscle activities of the SM and SCM in PLB were significantly greater than those in QB in this study. Given that the SM and SCM attach between the cervical spine and the upper two ribs, increased muscle activity in these muscles during inspiration in patients with COPD can be interpreted as an attempt to increase intrathoracic volume by elevating the upper ribs and sternum (Neumann 2009). Increased SCM activity in PLB compared with QB is consistent with the results of a previous study indicating increased inspiratory rib cage expansion and recruitment of respiratory accessory muscles and reduced diaphragm recruitment during inspiration of PLB compared with tidal breathing (Breslin 1992).
In this study, muscle activities of the SM and SCM in a forward–leaning position, both WAHS and WAS, were greater than those in NP, even though the increased muscle activity of the SM in WAS relative to NP failed to reach statistical significance. Several mechanisms may explain these results. First, it is possible that increased activity of the SM and SCM overcame restricted downward movement of the diaphragm. The forward–leaning position results in increased intra–abdominal pressure by approximating the ribs to the pelvis, making it difficult for the diaphragm to descend caudally during inspiration (Landers et al. 2003; Crosbie, and Myles 1985). A second possibility is the reversal of muscle action by the stabilizing force of
the hand on the face in WAHS and of the forearm on the thigh in WAS. As the hands or forearms are stabilized, the sternum, clavicle, and rib cage can be pulled upward by the SM and SCM.
In this study, the PM showed the greatest muscle activity in WAS, followed by WAHS, and the lowest PM activity was observed in NP. These results may be explained by reversal of muscle contraction. When the distal limb segment is stabilized, the proximal limb segment can be mobilized. Decreased activity of the PM in WAHS, compared with that in WAS, may be attributable to increased SM and SCM activity in WAHS. However, muscle activities of the major muscles of respiration, including the diaphragm and intercostal muscles, were not measured, so the effects of changes in the activity of accessory muscles during different breathing maneuvers and of various positions on major muscle activity could not be determined in this study. Additionally, the effects of breathing maneuvers and sitting postures on pulmonary function in patients with COPD remain unclear because of limitations in the measurement of lung volume and dyspnea according to breathing maneuver and sitting posture. Further studies are required to measure the major muscles of respiration, including examination of various activities and conditions of ventilatory insufficiency, using various pulmonary parameters and dyspnea scales.
Conclusion
These results suggest that in COPD patients, PLB induced a favorable breathing pattern (as assessed by TV and RR) in comparison with QB. Additionally, WAS and WAHS induced increased activity of inspiratory accessory muscles during inspiration compared with NP in COPD. Differential involvement of the accessory respiratory muscles can be readily studied in COPD patients, allowing monitoring of respiratory load during pulmonary rehabilitation. Finally, PLB combined with WAS or WAHS can be recommended for reduced diaphragmatic respiratory work in COPD patients.
References
Agostoni E, and Hyatt, RE. Static behavior of the respiratory system, Handbook of physiology. Section 3. The respiratory system, Vol III, in: A Fishman, P Macklem, J Mead, S Geiger, editors. Bethesda, Maryland: American Physiological Society, 1986.
Banzett RB, Topulos GP, Leith DE, and Nations CS. Bracing arms increases the capacity for sustained hyperpnea. Am Rev Respir Dis. 1988;138(1):106-109.
Bhatt SP GR, Luqman–Arafath TK, Gupta AK, Mohan A, Nanda S, and Stoltzfus JC. Effect of tripod position on objective parameters of respiratory function in stable chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci. 2009;51(2):83-85.
Bianchi R GF, Romagnoli I, Lanini B, Castellani C, Grazzini M, and Scano G. Patterns of chest wall kinematics during volitional pursed-lip breathing in COPD at rest. Respir Med. 2007;101(7):1412-1418.
Brannon FJ, Foley MW, Starr JA, and Saul LM. Cardiopulmonary Rehabilitation:
Breslin EH. The pattern of respiratory muscle recruitment during pursed–lip breathing. Chest. 1992;101(1):75-78.
Crosbie WJ, and Myles S. An investigation into the effect of postural modification on some aspects of normal pulmonary function. Physiotherapy. 1985;71(7):311-314.
Faling LJ. Pulmonary rehabilitation–physical modalities. Clinics in chest medicine 1986;7(4):599-618.
Gosselink R. Breathing techniques in patients with chronic obstructive pulmonary disease (COPD). Chron Respir Dis. 2004;1(3):163-172.
Jones AYM, Dean E, and Chow C. Comparison of the oxygen cost of breathing exercises and spontaneous breathing in patients with stable chronic obstructive pulmonary disease. Phys Ther. 2003;83(5):424-431.
Kera T, and Maruyama H. The effect of posture on respiratory activity of the abdominal muscles. J Physiol Anthropol Appl Human Sci. 2005;24(4):259-265.
Kisner C, and Colby LA. Therapeutic exercise: foundations and techniques. 3rd ed. Philadelphia: FA Davis, 1996.
Klimathianaki M, Vaporidi K, and Georgopoulos D. Respiratory muscle dysfunction in COPD: from muscles to cell. Curr Drug Targets. 2011;12(4):478-488.
Landers MR, Barker G, Wallentine S, McWhorter JW, and Peel C. A comparison of tidal volume, breathing frequency, and minute ventilation between two sitting postures in healthy adults. Physiother Theory Pract. 2003;19:109–119.
Landers MR, McWhorter JW, Filibeck D, and Robinson C. Does sitting posture in chronic obstructive pulmonary disease really matter? An analysis of 2 sitting postures and their effect [corrected] on pulmonary function. J Cardiopulm Rehabil. 2006;26(6):405-409.
Lee LJ, Chang AT, Coppieters MW, and Hodges PW. Changes in sitting posture induce multiplanar changes in chest wall shape and motion with breathing. Respir
Physiol Neurobiol. 2010;170(3):236-245.
Lin F, Parthasarathy S, Taylor SJ, Pucci D, Hendrix RW, and Makhsous M. Effect of different sitting postures on lung capacity, expiratory flow, and lumbar lordosis.
Martin AD, and Davenport PW. Extrinsic threshold PEEP reduces post–exercise dyspnea in COPD patients: A placebo–controlled, double-blind cross–over study.
Cardiopulm Phys Ther J. 2011;22(3):5-10.
Miravittles M. Management of COPD exacerbations. Multidiscip Resp Med. 2006;1(4):82-85.
Neumann DA. Kinesiology of the musculoskeletal system: foundation for physical
rehabilitation. 2nd ed. Philadelphia: Mosby, 2009.
O‘Donnell DE, Sanii R, and Younes M. Improvement in exercise endurance in patients with chronic airflow limitation using continuous positive airway pressure.
Am Rev Respir Dis. 1988;138(6):1510-1514.
Papavramidis TS, Kotidis E, Ioannidis K, Cheva A, Lazou T, Koliakos G, Karkavelas G, and Papavramidis ST. Diaphragmatic adaptation following intra-abdominal weight charging. Obes Surg. 2011;21(10):1612-1616.
Petrof BJ, Calderini E, and Gottfried SB. Effect of CPAP on respiratory effort and dyspnea during exercise in severe COPD. J Appl Physiol. 1990;69(1):179–188.
Petty TL, and Guthrie A. The effects of augmented breathing maneuvers on ventilation in severe chronic airway obstruction. Respir Care. 1971;16:104-111.
Prandi E, Couture J, and Bellemare F. In normal subjects bracing impairs the function of the inspiratory muscles. Eur Respir J. 1999;13(5):1078-1085.
Puhan MA, and Steurer–Stey C. Physical exercise for COPD: initiation and long-term maintenance. Multidiscip Resp Med. 2007;2(2):63-68.
Rabe KF HS, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, and Zielinski J. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532-555.
Serres I, Hayot M, Préfaut C, and Mercier J. Skeletal muscle abnormalities in patients with COPD: contribution to exercise intolerance. Med Sci Sports Exerc. 1998;30(7):1019-1027.
Shaffer TH, Wolfson MR, and Bhutani VK. Respiratory muscle function, assessment, and training. Phys Ther. 1981;61(12):1711-1723.
Sharp JT, Drutz WS, Moisan T, Foster J, and Machnach W. Postural relief of dyspnea in severe chronic obstructive pulmonary disease. Am Rev Respir Dis. 1980;122(2):201-211.
Simpson LS. Effect of increased abdominal muscle strength on forced vital capacity and forced expiratory volume. Phys Ther. 1983;63(3):334-337.
Spahija J, de Marchie M, and Grassino A. Effects of imposed pursed–lips breathing on respiratory mechanics and dyspnea at rest and during exercise in COPD. Chest. 2005;128(2):640-650.
Willeput R, and Sergysels R. Respiratory patterns induced by bent posture in COPD patients. Rev Mal Respir. 1991;8(6):577.
국문 요약
호흡방법과 앉은 자세 형태가 만성폐쇄성폐질환
환자의 흡기 보조근 근활성도에 미치는 영향
연세대학교 대학원
물리치료학 전공
김 기 송
본 연구의 목적은 호흡운동 방법과 앉아있기 자세가 만성폐쇄성폐질환 환자들의 1회 호흡량, 호흡빈도, 그리고 흡기 보조근의 근활성도에 어떻게 영향을 미치는 지를 알아보는 것이었다. 12명의 만성폐쇄성폐질환 환자가 본 연구에 참여하였다. 본 연구의 데이터를 수집하기 위하여 유도성 호흡계 체적변동기록장치와 표면 근 전도기기를 사용하여 두 가지 호흡방법(평상 시 호흡방법과 오므린 입술 호흡방법)으로 호흡을 할 때와 세 가지 형태의 앉은 자세 형태(고관절과 체간이 90도로 굴곡되어 유지되는 중립위치의 앉은 자세 형태, 팔꿈치와 앞 팔을 무릎에 기대고체간을 전방으로 굴곡시켜 앉은 자세 형태 그리고 팔꿈치를 무릎에 기댄 채 양 손으로 머리를 받쳐 고정하고 체간을 전방으로 굴곡시켜 앉은 자세 형태)를 조합하여 적용하였을 때 각각의 조합들에서 환자들의 1회 호흡량, 호흡빈도, 그리고 흡기 보조근의 근활성도를 호흡주기 중 흡기주기 동안에 맞춰 데이터를 동시에 측정하였다. 2요인 3수준 군간 반복 측정된 데이터를 분석하기 위해 반복 측정된 이원분산분석 방법을 이용하여 통계학적 유의성을 검증하였으며, 앉아있기 자세에 따라 통계학적으로 유의한 차이가 있을 경우 본페로니 사후 검정을 통하여 호흡방법에 따른 대응 별 비교에서 유의성의 차이를 확인하였다. 본 연구의 호흡방법에 따른 결과에서, 오므린 입술 호흡방법을 하였을 때가 평상 시 호흡방법을 하였을 때 보다 1회 호흡량은 유의하게 증가되었고, 호흡 빈도는 유의하게 감소되었다. 목갈비근과 흉쇄유돌근의 근활성도는 오므린 입술 호흡방법을 하였을 때 평상 시 호흡방법을 하였을 때 보다 유의하게 증가하였다. 본 연구의 앉은 자세 형태에 따른 결과에서 1회 호흡량과 호흡 빈도는 자세 형태에 따라 유의한 차이가 없었다. 그러나 목갈비근, 흉쇄유돌근 그리고 대흉근의 근활성도는 팔꿈치와 앞 팔을 무릎에 기대고 체간을 전방으로 굴곡시켜 앉은 자세와 팔꿈치를 무릎에 기댄 채 양 손으로
머리를 받쳐 고정하고 체간을 전방으로 굴곡시켜 앉은 자세 형태를 유지하고 있을 때가 고관절과 체간이 90도로 굴곡되어 유지되는 중립위치의 앉은 자세 형태를 유지하고 있을 때와 비교하여 유의하게 증가되었다. 결과를 종합하여 볼 때, 오므린 입술 호흡 방법은 만성폐쇄성폐질환 환자의 호흡을 치료하고자 하는 방향인 1회 호흡량은 증가시키고 호흡빈도는 감소시켰으며, 팔꿈치와 앞 팔을 무릎에 기대고 체간을 전방으로 굴곡시켜 앉은 자세와 팔꿈치를 무릎에 기댄 채 양 손으로 머리를 받쳐 고정하고 체간을 전방으로 굴곡시켜 앉은 자세 형태를 취하게 하였을 땐, 흡기보조근의 근활성도를 증가시켰다. 결론적으로 이 연구의 결과들은 향후 다른 호흡보조근을 포함한 연구와 호흡계 재활을 위한 치료 시 환자들이 느끼는 호흡 부담을 평가하는 데 도움이 될 수 있을 것이라 판단된다. 아울러 오므린 입술 호흡과 이 연구에서 사용된 체간을 전방으로 굴곡시킨 두 가지 다른 형태의 앉은 자세들의 조합은 만성폐쇄성폐질환 환자가 환기요구가 증가된 상황에서 횡격막의 호흡 일을 줄일 수 있게 할 수 있는 방법으로 추천될 수 있을 것이다.
핵심 되는 말: 만성페쇄성폐질환, 앉아있기 자세, 오므린 입술 호흡법, 전방굴곡 자세, 평상 시 호흡, 흡기보조근