저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다.
Relationship Between Intravascular Ultrasound Parameters
and Fractional Flow Reserve in Intermediate Coronary
Artery Stenosis of Left Anterior Descending Artery
– Intravascular Ultrasound volumetric analysis –
by
Hyoung-Mo Yang
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
Relationship Between Intravascular Ultrasound Parameters
and Fractional Flow Reserve in Intermediate Coronary
Artery Stenosis of Left Anterior Descending Artery
– Intravascular Ultrasound volumetric analysis –
by
Hyoung-Mo Yang
A Dissertation Submitted to The Graduate School of
Ajou University in Partial Fulfillment of the Requirements
for the Degree of
Ph.D. in Medicine
Supervised by
Seung-JeaTahk, M.D., Ph.D.
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
This certifies that the dissertation
ofHyoung-Mo Yang is approved.
SUPERVISORY COMMITTEE
Seung-JeaTahk
Joon-Han Shin
Ki-Dong Yoo
Myeong-Ho Yoon
So-Yeon Choi
The Graduate School, Ajou University
June, 18th, 2013
-
ABSTRACT
-Relationship Between Intravascular Ultrasound Parameters and
Fractional Flow Reserve in Intermediate Coronary Artery Stenosis
of Left Anterior Descending Artery
Abstract
Background/Objectives: The objective of this study was to assess the relationship between intravascular ultrasound (IVUS) parameters, including volumetric analysis, and fractional flow reserve (FFR). Methods: Both IVUS and FFR were performed in 206 cases of
intermediate stenosis of the left anterior descending artery (LAD). Myocardial ischemia was assessed by FFR and maximal hyperemia was induced by continuous intracoronary
adenosine infusion. FFR < 0.80 was considered as significant inducible myocardial ischemia. We performed standard IVUS parameter measurements and volumetric analyses. IVUS parameter comparison was performed in the presence (n=90) or absence (n=116) of significant myocardial ischemia. Results: Lesions with minimal lumen area (MLA)
≥4.0mm2 had FFR ≥0.80 in 91.4% of cases, while 50.9% of lesions with MLA <4.0mm2 had
FFR <0.80. The multiple logistic regression analysis demonstrated that IVUS lesion length (odds ratio [OR]: 1.1, 95% confidence interval [CI] =1.1–1.2, p<0.001) and MLA
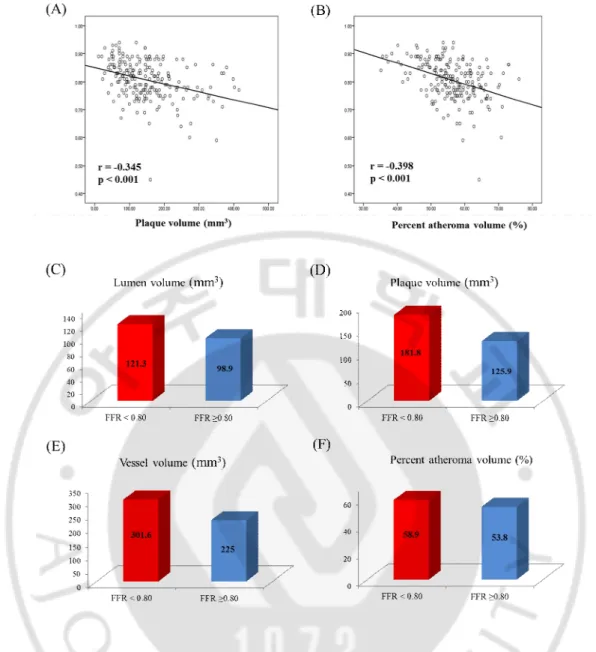
significance according to lesion location (OR: 8.8, 95% CI = 4.4-17.8, p< 0.001) were independent predictors of functionally significant myocardial ischemia (FFR < 0.80). FFR correlated with plaque volume (r= -0.345, p<0.001) and percent atheroma volume (PAV)
(r=-0.398, p<0.001). Lesions with significant ischemia (FFR <0.80) as compared to those with FFR >0.80 were associated with larger plaque volume (181.8±82.3 vs. 125.9±77.9 mm3,
p<0.001) and PAV (58.9±5.6 vs. 53.8± 7.9 %, p<0.001).
Conclusions: IVUS parameters representing severity and extent of atheromatous plaque correlated with functional significance in LAD lesions with intermediate stenosis.
Keywords
: Intravascular ultrasound, Fractional flow reserve, Plaque volumeTABLE OF CONTENTS
ABSTRACT ··· ⅰ TABLE OF CONTENTS ··· ⅱi
LIST OF FIGURES ··· iv
LIST OF TABLES ··· v
I. INTRODUCTION ··· 1
II. MATERIALS AND METHODS ··· 3
A. Study population ··· 3
B. Quantitative coronary angiography ··· 3
C. Intravascular ultrasound analyses ··· 4
D. Measurement of fractional flow reserve ··· 5
E. Statistical analysis ··· 5
III. RESULTS A. Baseline clinical and angiographic characteristics ··· 7
B. Relationship between FFR and IVUS parameters ··· 10
C. IVUS parameters for functionally significant myocardial ischemia ··· 14
D. IVUS volumetric analysis and FFR ··· 17
IV. DISUCUSSION ··· 20
V. CONCLUSION ··· 24
REFERENCES ··· 25
LIST OF FIGURES
Fig. 1. Comparison of minimal lumen area and FFR ··· 11
Fig. 2. Relationship between FFR and IVUS parameters ··· 12
Fig. 3. Best cut off values of IVUS parameters ··· 13
Fig. 4. Effect of MLA and lesion length on FFR ··· 16
Fig. 5. Relationship between IVUS volumetric parameters and FFR ··· 18
LIST OF TABLES
Table 1. Baseline clinical and angiographic characteristics ··· 8
Table 2. Baseline QCA and IVUS results ··· 9
Table 3. Comparison of IVUS parameters according to the presence of
I. Introduction
Intravascular ultrasound (IVUS) and fractional flow reserve (FFR) have been used to overcome the limitations of quantitative coronary angiography in evaluation of myocardial ischemia associated with coronary intermediate stenosis (Topol과 Nissen, 1995; Fischer 등, 2001; Tobis 등, 2001). IVUS is a useful imaging modality while FFR is a good tool to evaluate the presence of myocardial ischemia. The greater simplicity of IVUS and the nature of information it provides have favored its broader use over FFR in many catheterization laboratories, and being able to predict myocardial ischemia using IVUS parameters therefore would be clinically relevant.
Studies evaluating the relationship between FFR and IVUS parameters mainly focusing on the minimal lumen area (MLA) site and not the whole atherosclerotic lesion have documented a relationship between MLA and FFR, with a low positive predictive value for different MLA cutoff values used, and debate persisting over the best cutoff value (BCV) of MLA to predict functional significance (Takagi 등, 1999; Briguori 등, 2001; Ben-Dor 등, 2011; Kang 등, 2011). Previous studies evaluated all coronary lesions including left anterior descending (LAD), left circumflex (LCX), right coronary artery (RCA) as well as different locations from proximal to distal. Since FFR is influenced by many parameters such as the burden of supplying myocardium and reference vessel size, studies including these heterogenous groups have limitations in assessing the relationship between functional and anatomic parameters due to confounding variables. We have reported on the importance of LAD to predict functional significance using anatomic parameters. If an intermediate lesion was located on the LAD or proximal location, the possibility for it being functionally
significant was higher than that for other locations and the diagnostic accuracy of minimal lumen area was highest in the proximal LAD (Koo 등, 2011).
Although it is well known that coronary atherosclerosis burden measured by IVUS is related with clinical outcomes (Nicholls 등, 2010), its relationship with functional
significance remains unknown. We therefore evaluated potential relationships between FFR and all IVUS parameters including volumetric analyses in LAD.
II. Materials and Methods
A. Study population
From Jan 2009 to Dec 2012, we enrolled 206 patients with intermediate coronary artery stenotic lesions of LAD using both IVUS and FFR guidance. We included patients with silent ischemia, or stable or unstable angina who underwent elective coronary angiography. Angiographic inclusion criteria were 40-70% de novo coronary artery stenosis at the
proximal or mid portion of the LAD and mean reference vessel diameter ≥ 3.0 mm by visual estimation. Exclusion criteria were myocardial infarction, ejection fraction <40%, regional wall motion abnormalities on echocardiography, primary myocardial or valvular heart disease, additional stenosis (>30% by visual estimation) in target vessel, restenosis lesion, left main lesion, presence of collateral vessel and contraindication to adenosine. The study protocol was approved by the institutional review board.
B. Quantitative coronary angiography
Coronary angiography was performed following standard technique after intracoronary administration of 100 to 200μg nitroglycerin (NTG). Intermediate lesion was defined as 40-70% diameter stenosis by visual estimation. Quantitative coronary angiography (QCA) analysis was performed using the Cardiovascular Angiography Analysis System II (CAAS II, Pie Medical, Maastricht, Netherlands). The percent diameter stenosis (DS), minimal luminal diameter (MLD), reference vessel diameter (RVD) and lesion length were measured and calculated. Lesion location was determined according to the American Heart Association classification (Austen 등, 1975). Proximal LAD was defined as the segment between the
branching point of the left main and the first major septal or diagonal branch. Mid LAD spanned up to one-half the distance from the 1st septal/diagonal branch to apex. QCA was
performed by an experienced observer who was blinded to the FFR and IVUS findings.
C. Intravascular ultrasound analyses
IVUS was performed using the Galaxy 2TM IVUS System (Boston Scientific Corporation,
Natick, MA, USA) after intracoronary administration of 100 to 200μg nitroglycerin (NTG), a 40-MHz coronary imaging IVUS catheter (Atlantis SR Pro, Natick, MA, USA) was
advanced as far distal as possible in the target vessel followed by automatic pullback at 0.5mm per sec.
Quantitative IVUS analyses were performed by 2 independent observers blinded to the FFR and QCA information according to the American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of
intravascular ultrasound studies (Mintz 등, 2001). Lumen cross-sectional area (CSA) was quantified by planimetry of the leading edge of the blood-intima acoustic interface, and MLA was measured at the narrowest luminal cross section. The external elastic membrane (EEM) CSA was detected as the interface between media and adventitia. Reference areas were the sites with the largest lumen proximal or distal to a stenosis but within 10 mm with no major intervening branches. Atheroma CSA was calculated as the EEM CSA minus the lumen CSA. Plaque burden at MLA site was calculated as 100 x atheroma CSA/EEM CSA and area stenosis was calculated as 100 x (reference lumen CSA - MLA)/ reference lumen CSA. Remodeling index was calculated as lesion EEM CSA/reference EEM CSA. A lesion represents accumulation of atherosclerotic plaque compared with a predefined reference and
lesion length was measured with automatic pullback. Quantitative analyses included vessel, lumen and total atheroma volumes. To standardize vessel size, we calculated percent atheroma volume (PAV) defined as total atheroma volume divided by vessel volume x 100. All IVUS analyses were performed using computerized planimetry software (EchoPlaque 3.0, Indec Systems, Santa Clara, CA).
D. Measurement of fractional flow reserve
FFR was measured with a 0.014-inch pressure wire (PressureWire, Radi Medical System, Uppsala, Sweden) which was advanced distally to the stenosis after 100 to 200μg
intracoronary administration of NTG. The pressure wire was externally calibrated and then advanced to the distal tip of the guiding catheter. It was verified whether equal pressure was recorded at both the catheter and the pressure wire. The pressure wire was advanced into the coronary artery, and positioned distal to the stenosis. Distal coronary pressure (Pd) and proximal coronary pressure (Pa) were measured simultaneously at baseline and maximal hyperemia. FFR was calculated by dividing mean Pd by mean Pa during maximal hyperemia. Maximal hyperemia was induced with continuous intracoronary adenosine infusion using a microcatheter (>360
µ
g/min)(Yoon 등, 2009). We considered FFR <0.80 as significant inducible myocardial ischemia.E. Statistical analysis
Data are presented as means ± standard deviations for continuous variables and frequency (percentage) for categorical variables. Comparison of continuous variables was performed using the unpaired t-test. Analysis of discrete variables was performed using the chi-square
test or Fisher’s exact test. Multivariate logistic regression analysis was performed to identify independent predictors of significant myocardial ischemia (FFR <0.80). Receiver operating characteristic (ROC) curve analysis was used to determine the best cutoff values (BCV) of IVUS parameters as a predictor of the functional significance of a lesion (FFR <0.80). Using ROC curve analysis, we calculated sensitivity and specificity and BCV were determined by the maximum sum of sensitivity and specificity. MedCalc (MedCalc Software, Belgium) was used for ROC curve analysis, and all other statistical analyses were performed using SPSS 18.0. A p value of <0.05 was considered statistically significant.
III. Results
A. Baseline clinical and angiographic characteristics
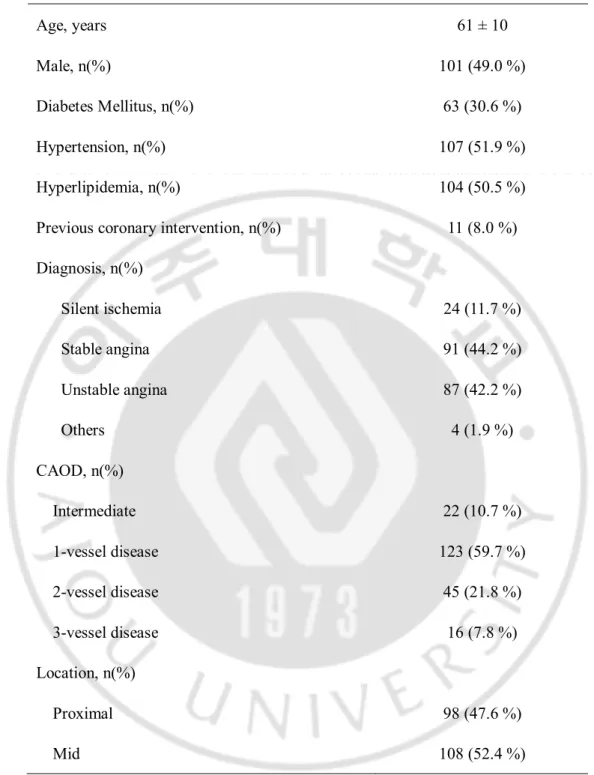
We enrolled 206 patients, 91 (44.2%) patients with stable angina and 87 (42.2%) patients with unstable angina. Mean age was 61±10 years, 63 (30.6%) patients had diabetes, and 61 (29.6%) patients had multivessel disease. Mean reference vessel diameter was 3.3±0.3 mm and mean lesion length on IVUS was 20.0 ± 8.2 mm (Tables 1 and 2). One hundred seventy-one (83.0 %) patients had lesion MLA <4.0 mm2 on IVUS, however, only 87 (50.9%) of
Table 1. Baseline clinical and angiographic characteristics (n=206). Age, years 61 ± 10 Male, n(%) 101 (49.0 %) Diabetes Mellitus, n(%) 63 (30.6 %) Hypertension, n(%) 107 (51.9 %) Hyperlipidemia, n(%) 104 (50.5 %)
Previous coronary intervention, n(%) 11 (8.0 %)
Diagnosis, n(%) Silent ischemia Stable angina 24 (11.7 %) 91 (44.2 %) Unstable angina Others 87 (42.2 %) 4 (1.9 %) CAOD, n(%) Intermediate 22 (10.7 %) 1-vessel disease 123 (59.7 %) 2-vessel disease 45 (21.8 %) 3-vessel disease 16 (7.8 %) Location, n(%) Proximal 98 (47.6 %) Mid 108 (52.4 %)
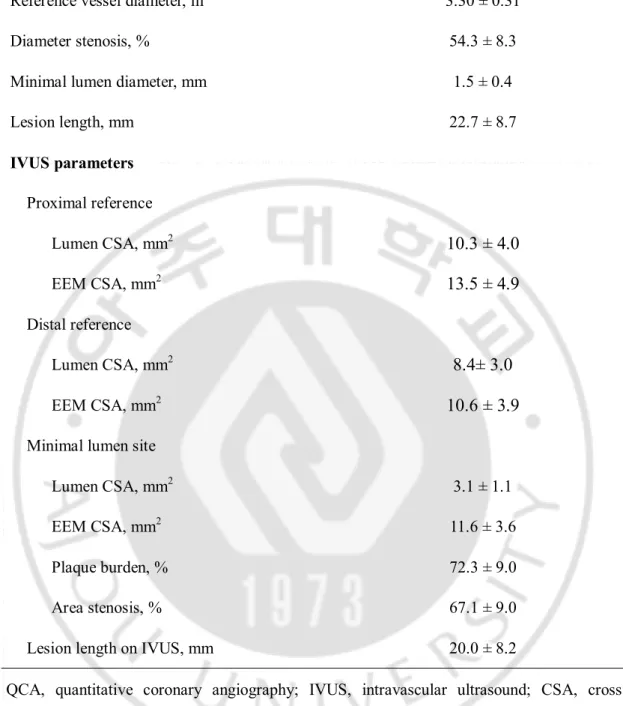
Table 2. Baseline QCA and IVUS results (n=206).
Reference vessel diameter, m 3.30 ± 0.31
Diameter stenosis, % 54.3 ± 8.3
Minimal lumen diameter, mm 1.5 ± 0.4
Lesion length, mm 22.7 ± 8.7 IVUS parameters Proximal reference Lumen CSA, mm2
10.3 ± 4.0
EEM CSA, mm213.5 ± 4.9
Distal reference Lumen CSA, mm28.4± 3.0
EEM CSA, mm210.6 ± 3.9
Minimal lumen site
Lumen CSA, mm2 3.1 ± 1.1
EEM CSA, mm2 11.6 ± 3.6
Plaque burden, % 72.3 ± 9.0
Area stenosis, % 67.1 ± 9.0
Lesion length on IVUS, mm 20.0 ± 8.2
QCA, quantitative coronary angiography; IVUS, intravascular ultrasound; CSA, cross sectional area; EEM, external elastic membrane.
Relationship between FFR and IVUS parameters
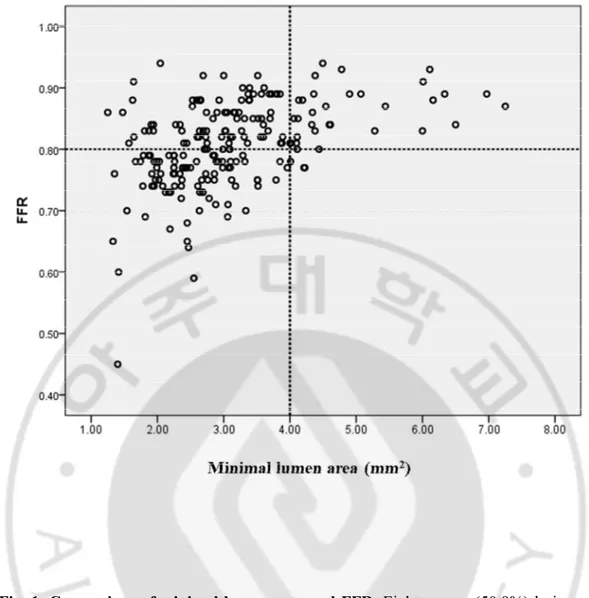
Eighty-seven (50.9%) lesions with IVUS MLA <4.0 mm2 had FFR <0.80, while 3 (8.6%)
lesions with IVUS MLA ≥4.0 mm2 had FFR <0.80 (Fig. 1). Also, 96.7% of lesions with FFR
<0.80 had IVUS MLA <4.0 mm2. FFR correlated with IVUS parameters including MLA
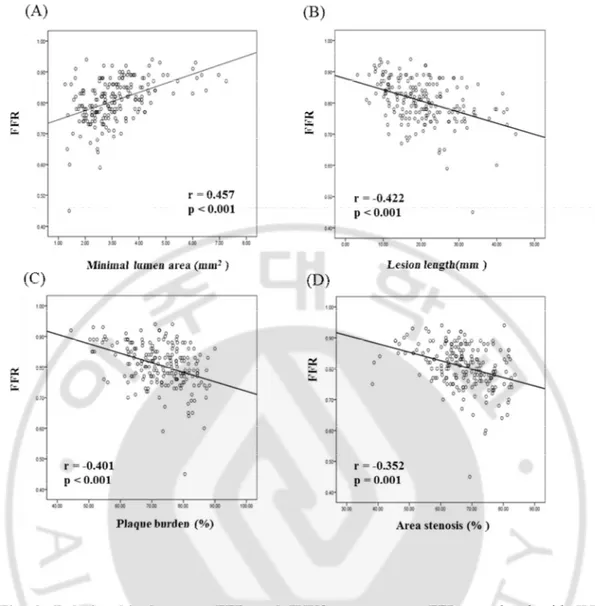
(r=0.457, p<0.001), plaque burden (r= -0.401, p<0.001), lesion length (r= -0.422, p<0.001) and area stenosis (r= -0.352, p=0.001) (Fig. 2).
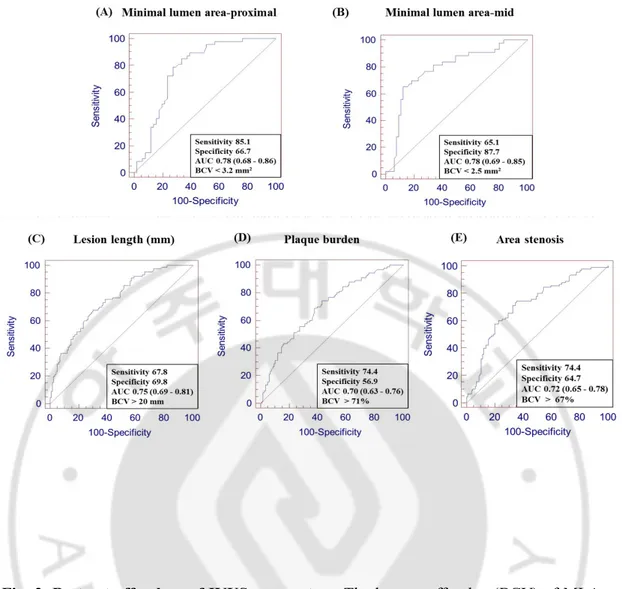
We also obtained the best cutoff value of IVUS parameters to predict functional
significance. The best cutoff value (BCV) of MLA to predict functional significance was 3.2 mm2 (AUC 0.78, 95% CI 0.68 - 0.86) for proximal and 2.5mm2 for mid lesions (AUC 0.78,
95% CI 0.69-0.85), 20 mm for lesion length (AUC 0.75, 95% CI 0.69-0.81) and 71% for plaque burden (AUC 0.70, 95% CI 0.63-0.76), respectively (Fig. 3).
Fig. 1. Comparison of minimal lumen area and FFR. Eighty-seven (50.9%) lesions with IVUS MLA <4.0 mm2 had FFR <0.80, while 3 (8.6%) lesions with IVUS MLA ≥4.0 mm2
had FFR <0.80. FFR, fractional flow reserve; IVUS, intravascular ultrasound; MLA, minimal lumen area.
Fig. 2. Relationship between FFR and IVUS parameters. FFR correlated with IVUS parameters including MLA (A), lesion length (B), plaque burden (C), and area stenosis (D). FFR, fractional flow reserve; IVUS, intravascular ultrasound; MLA, minimal lumen area.
Fig. 3. Best cut off values of IVUS parameters. The best cutoff value (BCV) of MLA to predict functional significance was 3.2 mm2 for proximal (A) and 2.5mm2 for mid lesions
(B), 20 mm for lesion length (C), 71% for plaque burden (D), and 67% for area stenosis (E),respectively. IVUS, intravascular ultrasound; BCV, best cutoff value; MLA, minimal lumen area; AUC, area under the curve; CI, confidence interval)
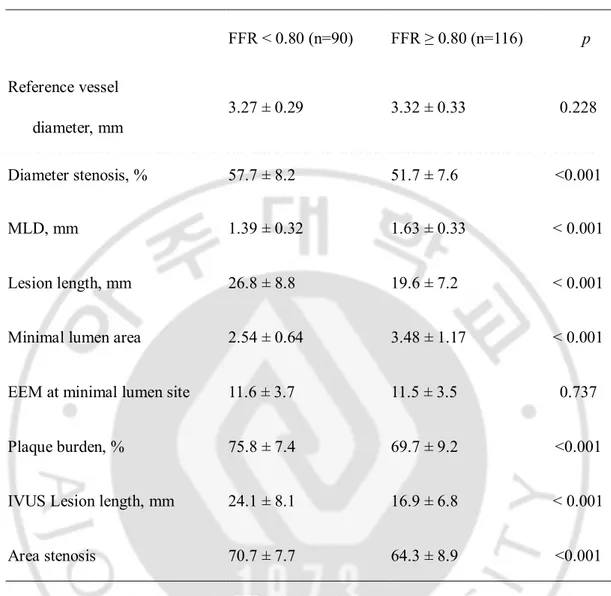
IVUS parameters for functionally significant myocardial ischemia
We compared IVUS parameters between lesions with FFR <0.80 and FFR ≥0.80. Lesions with significant myocardial ischemia (FFR <0.80) had smaller minimal lumen area (2.54 ± 0.64 vs. 3.48 ± 1.17 mm2, p<0.001), longer lesion length (26.8 ± 8.8 vs. 19.6 ± 7.2 mm,
p<0.001), larger plaque burden at MLA site (75.8 ± 7.4 vs. 69.7 ± 9.2 %, p<0.001) and more severe area stenosis (70.7 ± 7.7 vs. 64.3 ± 8.9 %, p<0.001). However, there were no
significant differences in plaque eccentricity and remodeling index between the 2 groups (Table 3).
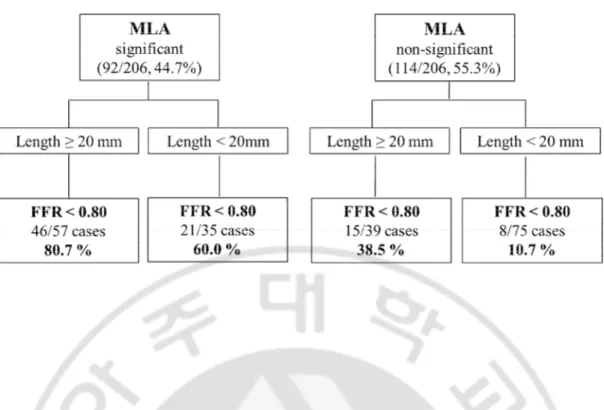
Multivariate logistic regression analysis was performed to identify independent predictors for significant ischemia (FFR <0.80). Independent variables included reference vessel diameter, diameter stenosis, MLA significance according to lesion location, IVUS lesion length, plaque burden, area stenosis, PAV and lumen volume/length. The multiple logistic regression analysis demonstrated that IVUS lesion length (odds ratio [OR]: 1.1, 95% confidence interval [CI] =1.1–1.2, p<0.001) and MLA significance according to lesion location (OR: 8.8, 95% CI = 4.4-17.8, p< 0.001) were independent predictors of functionally significant myocardial ischemia (FFR < 0.80).
In lesions with MLA significance less than cutoff value according to lesion location and lesion length ≥20 mm, 80.7% of lesions had FFR < 0.80. In contrast, both MLA according to lesion location and lesion length were non-significant, only 10.7 % of lesions were FFR < 0.80 (Fig. 4).
Table 3. Comparison of IVUS parameters according to the presence of significant myocardial ischemia (FFR < 0.80). FFR < 0.80 (n=90) FFR ≥ 0.80 (n=116) p Reference vessel diameter, mm 3.27 ± 0.29 3.32 ± 0.33 0.228 Diameter stenosis, % 57.7 ± 8.2 51.7 ± 7.6 <0.001 MLD, mm 1.39 ± 0.32 1.63 ± 0.33 < 0.001 Lesion length, mm 26.8 ± 8.8 19.6 ± 7.2 < 0.001
Minimal lumen area 2.54 ± 0.64 3.48 ± 1.17 < 0.001
EEM at minimal lumen site 11.6 ± 3.7 11.5 ± 3.5 0.737
Plaque burden, % 75.8 ± 7.4 69.7 ± 9.2 <0.001
IVUS Lesion length, mm 24.1 ± 8.1 16.9 ± 6.8 < 0.001
Area stenosis 70.7 ± 7.7 64.3 ± 8.9 <0.001
IVUS, intravascular ultrasound; FFR, fractional flow reserve; MLD, minimal luminal diameter; EEM, external elastic membrane.
Fig. 4. Effect of MLA and lesion length on FFR. In lesions with MLA significance according to lesion location and lesion length ≥20 mm, 80.7% of lesions had FFR < 0.80. In contrast, when both MLA and lesion length were non-significant, only 10.7 % of lesions had FFR < 0.80. MLA, minimal lumen area; FFR, fractional flow reserve.
IVUS volumetric analysis and FFR
FFR correlated with total atheroma volume (r= -0.345, p<0.001) and PAV (r= -0.398, p<0.001) at target lesion. Volumetric IVUS analyses showed that the lesions with significant myocardial ischemia (FFR <0.80) had larger lumen volume (121.3±50.1 vs. 98.9±42.3 mm3,
p=0.001), vessel volume (301.6±125.6 vs. 225.0±113.5 mm3, p<0.001), total atheroma
volume (181.8±82.3 vs. 125.9±77.9 mm3, p<0.001) and PAV of target lesion (58.9±5.6 vs.
53.8± 7.9 %, p<0.001) (Fig. 5).
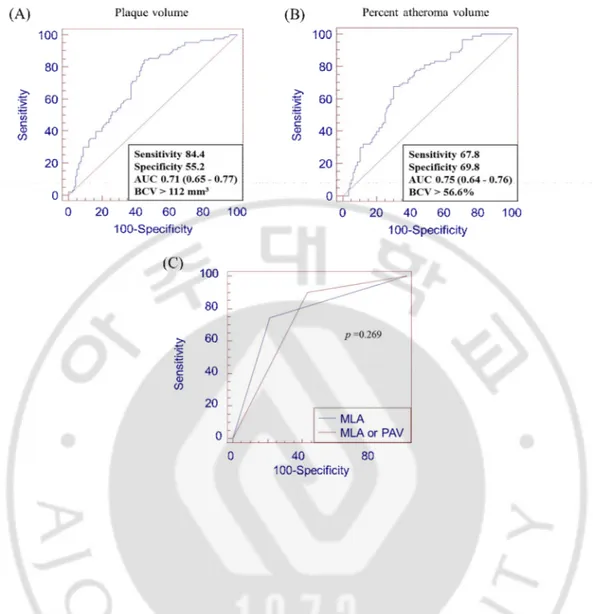
ROC cure analysis showed the BCV of plaque volume at target lesion to predict FFR < 0.80 was 112.0 mm3 (AUC 0.71, 95% CI 0.65 - 0.77) and 56.6% for PAV at target lesion
(AUC 0.75, 95% CI 0.64-0.76). However, in ROC comparison analysis between MLA and volumetric parameters at target lesion, there were no significant additional benefits in diagnostic accuracy (Fig. 6).
Fig. 5. Relationship between IVUS volumetric parameters and FFR. FFR correlated with plaque volume (r= -0.345, p<0.001)(A), PAV (r= -0.398, p<0.001)(B) at target lesion. The lesions with significant myocardial ischemia (FFR <0.80) had larger lumen volume (C), plaque volume (D), vessel volume (E), and PAV of target lesion (F). IVUS, intravascular ultrasound; FFR, fractional flow reserve; PAV, percent atheroma volume.
Fig. 6. ROC curve analysis of volumetric parameters. The BCV of plaque volume at target lesion was 112.0 mm3 (A) and 56.6% for PAV (B) at target lesion to predict FFR <
0.80. ROC comparison analysis between MLA and PAV at target lesion(C). ROC curve, receiver operating characteristic curve; BCV, best cut-off value; FFR, fractional flow reserve; PAV, percent atheroma volume; MLA, minimal lumen area
IV. Discussion
The main findings of this study are that IVUS lesion length, MLA according to lesion location and plaque volume, i.e., variables that represent severity and extent of atheromatous plaques, were related with functional significance in intermediate coronary artery stenosis of the LAD.
FFR is an invasive method to evaluate myocardial ischemia defined as the ratio of pressure measured distal to the stenosis to aorta during hyperemia. Theoretically, pressure drop across the stenosis is related with viscous friction, flow separation and turbulence. The loss of flow separation pressure is affected by the geometry of the stenosis and rheological properties of blood, while viscous friction loss is determined by stenosis length and MLA, and these parameters can be measured by IVUS (Gould 등, 1978; Kolozsvári 등, 2011; Seiler 등, 1992; Spaan 등, 2006). In this study, the independent IVUS predictors of myocardial ischemia (FFR < 0.80) were MLA significance according to lesion location and IVUS measured lesion length.
The notion that a lesion with IVUS MLA ≥ 4.0 mm2 has a low clinical event rate in the
case of IVUS-guided deferralhas led many operators to perform PCI when IVUS MLA < 4.0 mm2 (Abizaid 등, 1998; Abizaid 등, 1999). In this study only 3 cases had functionally
significant lesions when MLA was ≥ 4.0 mm2. If an intermediate lesion shows IVUS MLA
≥4.0 mm2, the lesion could be safely deferred in almost all cases, however, if the lesion has
MLA <4.0 mm2 , one should consider many contributing factors which influence FFR such
as clinical presentation, lesion location, the amount of supplying myocardium, reference vessel size, plaque vulnerability and lesion length. Several studies have evaluated the
relationship between IVUS parameters and FFR and they have documented the relationship between FFR and MLA (Takagi 등, 1999; Briguori 등, 2001; Ben-Dor 등, 2011; Kang 등, 2011; Koo 등, 2011). We already reported that the MLA cutoff value to predict myocardial ischemia is influenced by lesion location, the diagnostic accuracy being higher in proximal lesions with less anatomic variations (Koo 등, 2011) and this study showed similar results. The BCV of MLA was 3.2 mm2 in proximal LAD lesions and 2.5 mm2 in mid LAD lesions.
Also, our study included only proximal or mid LAD lesions and reference vessel diameter ≥ 3.0 mm by visual estimation, allowing more accurate evaluation of the relationship between IVUS parameters and FFR by minimizing the effect of vessel size and anatomic variation. Since the BCV of MLA to predict functional significance is also influenced by reference vessel size, there was a limitation to determine the BCV of MLA in small reference vessels. IVUS catheter can cause spasm or stretch the vessel and ring down artifact especially in small coronary arteries. Moreover, several studies have failed to demonstrate the relationship between IVUS and FFR in small vessels (Costa 등, 2007; Koo 등, 2011).
Although in the analysis of the relationship between IVUS parameters and FFR, many previous studies mainly focused on MLA, lesion length is another important IVUS parameter. Lesion length in a previous study was very short (9 mm) (Briguori 등, 2001) and another study only evaluated length when IVUS MLA was < 3-4 mm2 (Kang 등, 2011), which is not
a practical method. In this study, about 50% of lesions had IVUS lesion length ≥ 20 mm and the BCV of lesion length for FFR < 0.80 was 20 mm. Our data showed that correlation coefficient between FFR and lesion length and AUC value of lesion length on ROC curve analysis were as good as MLA among IVUS parameters (Figs. 2, 3). Also, when both MLA according to lesion location and lesion length were considered as significant, 80.7% of
lesions had FFR < 0.80. In contrast, about 40 % of lesions were functionally significant in longer lesions despite MLA being non-significant according to location (Fig 4). Moreover, when both MLA and IVUS lesion length were non-significant, only 10% of cases had FFR < 0.80. We therefore should consider not only MLA but also lesion length and when evaluating intermediate lesions by IVUS.
In this study, plaque volume and PAV also had a negative correlation with FFR, and larger plaque volume and PAV were noted in lesions with FFR < 0.80. Some investigators have evaluated the relationship between plaque volume and FFR using different methods. Kolozsvári R et al have reported that plaque volume measured by three dimensional (3D) reconstruction of coronary angiography is an important parameter of functional significance (Kolozsvári 등, 2011) and Kristensen TS documented a significant correlation between FFR and plaque volume using coronary multi-detector computed tomography (MDCT)
(Kristensen 등, 2010); however, the plaque volume measured by 3D-QCA or MDCT is different from that directly measured by IVUS. Although the Phantom trial analyzed the relationship between FFR and plaque volume and found no correlation between the two parameters (Costa 등, 2007), it included only small vessels and relatively short lesions. To our knowledge, this is the first study to evaluate plaque volume and FFR in a major
epicardial coronary artery. Our study showed that amount and severity of atheromatous plaque measured by IVUS were correlated with FFR, and functionally significant lesions had larger plaque volume and PAV. A previous IVUS study showed that in patients who
experienced myocardial infarction, major adverse clinical outcomes were related to larger plaque volume and PAV (Nicholls 등, 2010). Also, it is well known that the presence of myocardial ischemia is related with clinical outcomes in patients with coronary artery
disease. Our study revealed that absolute amount of plaque volume and PAV at target lesion were related with myocardial ischemia. Although larger plaque volume and PAV were related with FFR, our study did not demonstrate that the combined criteria of MLA and PAV at target lesion increased the diagnostic accuracy on ROC curve analysis. Since FFR was influenced by atheromatous plaques throughout the entire coronary artery as well as at the target lesion itself, further analysis would be needed including residual plaque volume.
Limitations
This study had several limitations. First, this study enrolled patients who had a
proximal or mid-LAD lesion and reference vessel diameter > 3.0 mm by visual
estimation, and therefore further evaluation will be needed in the RCA and LCX.
However, the fact that assessment was performed in a homogenous group helped
minimize the effects of other confounding factors. Second, this study evaluated only
the relationship between two methods and not with clinical outcomes. Although
IVUS provides a vast amount of information during PCI and showed significant
relationship with FFR, further study will be needed to evaluate clinical outcomes
according to the practical use of FFR or IVUS parameters in clinical setting. Third,
we did not evaluate vulnerable plaque such as plaque rupture or large lipid core on
IVUS which were related acute coronary syndrome events. Finally, since FFR was
influenced by atheromatous plaques throughout the entire coronary artery as well as
at the target lesion itself, further analysis would be needed including residual plaque
volume.
V. Conclusion
IVUS parameters which represent severity and extent of atheromatous plaques correlated with functional significance in intermediate coronary artery stenosis of LAD.
References
1. Abizaid AS, Mintz GS, Mehran R, Abizaid A, Lansky AJ, Pichard AD, Satler LF, Wu H, Pappas C, Kent KM, Leon MB: Long-term follow-up after percutaneous
transluminal coronary angioplasty was not performed based on intravascular ultrasound findings: importance of lumen dimensions. Circulation 100:256-261, 1999
2. Abizaid A, Mintz GS, Pichard AD, Kent KM, Satler LF, Walsh CL, Popma JJ, Leon MB: Clinical, intravascular ultrasound, and quantitative angiographic determinants of the coronary flow reserve: before and after percutaneous transluminal coronary angioplasty. Am J Cardiol 82:423–428, 1998
3. Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB: A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 51:5–540, 1975
4. Ben-Dor I, Torguson R, Gaglia MA Jr, Gonzalez MA, Maluenda G, Bui AB, Xue Z, Satler LF, Suddath WO, Lindsay J, Pichard AD, Waksman R: Correlation between fractional flow reserve and intravascular ultrasound lumen area in intermediate coronary artery stenosis. EuroIntervention 7:225-233, 2011
5. Briguori C, Anzuini A, Airoldi F, Gimelli G, Nishida T, Adamian M, Corvaja N, Di Mario C, Colombo A : Intravascular ultrasound criteria for the assessment of the functional significance of intermediate coronary artery stenoses and comparison with fractional flow reserve. Am J Cardiol 87:136–141, 2001
6. Costa MA, Sabate M, Staico R, Alfonso F, Seixas AC, Albertal M, Crossman A, Angiolillo DJ, Zenni M, Sousa JE, Macaya C, Bass TA: Anatomical and physiologic assessments in patients with small coronary artery disease: final results of the
Physiologic and Anatomical Evaluation Prior to and After Stent Implantation in Small Coronary Vessels (PHANTOM) trial. Am Heart J 153:296.e1-7, 2007
7. Fischer JJ, Samady H, McPherson JA, Sarembock IJ, Powers ER, Gimple LW, Ragosta M: Comparison between visual assessment and quantitative angiography versus
fractional flow reserve for native coronary narrowings of moderate severity. Am J
Cardiol 90:210-215, 2001
8. Gould K: Pressure–flow characteristics of coronary stenoses in unsedated dogs at rest and during coronary vasodilation. Circ Res 43:242–253, 1978
9. Kang SJ, Lee JY, Ahn JM, Mintz GS, Kim WJ, Park DW, Yun SC, Lee SW, Kim YH, Lee CW, Park SW, Park SJ: Validation of intravascular ultrasound-derived parameters with fractional flow reserve for assessment of coronary stenosis severity. Circ
10. Kolozsvári R, Tar B, Lugosi P, Sánta J, Béres Z, Ungvári T, Polgár P, Kőszegi Z: Plaque volume derived from three-dimensional reconstruction of coronary angiography predicts the fractional flow reserve. Int J Cardiol 160:140-144, 2012
11. Koo BK, Yang HM, Doh JH, Choe H, Lee SY, Yoon CH, Cho YK, Nam CW, Hur SH, Lim HS, Yoon MH, Park KW, Na SH, Youn TJ, Chung WY, Ma S, Park SK, Kim HS, Tahk SJ:Optimal intravascular ultrasound criteria and their accuracy for defining the functional significance of intermediate coronary stenoses of different locations. JACC
Cardiovasc Interv 4:803-811, 2011
12. Kristensen TS, Engstrøm T, Kelbæk H, von der Recke P, Nielsen MB, Kofoed KF: Correlation between coronary computed tomographic angiography and fractional flow reserve. Int J Cardiol 144:200–205, 2010
13. Lee CH, Tai BC, Soon CY, Low AF, Poh KK, Yeo TC, Lim GH, Yip J, Omar AR, Teo SG, Tan HC: New set of intravascular ultrasound-derived anatomic criteria for defining functionally significant stenoses in small coronary arteries (results from Intravascular Ultrasound Diagnostic Evaluation of Atherosclerosis in Singapore [IDEAS] study). Am
J Cardiol 105:1378-1384, 2010
14. Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, Pinto FJ, Rosenfield K,Siegel RJ, Tuzcu EM, Yock PG: American College of Cardiology
Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll
Cardiol 37:1478-1492, 2001
15. Nicholls SJ, Hsu A, Wolski K, Hu B, Bayturan O, Lavoie A, Uno K, Tuzcu EM, Nissen SE: Intravascular ultrasound-derived measures of coronary atherosclerotic plaque burden and clinical outcome. J Am Coll Cardiol 55:2399-2407, 2010
16. Seiler C, Kirkeeide RL, Gould KL: Basic structure–function relations of the epicardial coronary vascular tree. Basis of quantitative coronary arteriography for diffuse coronary artery disease. Circulation 85:1987–2003, 1992
17. Spaan J, Piek J, Hoffman J, Siebes M: Physiological basis of clinically used coronary hemodynamic indices. Circulation 113:446–455, 2006
18. Takagi A, Tsurumi Y, Ishii Y, Suzuki K, Kawana M, Kasanuki H: Clinical potential of intravascular ultrasound for physiological assessment of coronary stenosis: relationship between quantitative ultrasound tomography and pressure-derived fractional flow reserve. Circulation 100:250–255, 1999
19. Tobis J, Azarbal B, Slavin L: Assessment of intermediate severity coronary lesions in the catheterization laboratory. J Am Coll Cardiol 49:839-848, 2007
20. Topol EJ and Nissen SE: Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease.
Circulation 92:2333-2342, 1995
21. Yoon MH, Tahk SJ, Yang HM, Park JS, Zheng M, Lim HS, Choi BJ, Choi SY, Choi UJ, Hwang JW, Kang SJ, Hwang GS, Shin JH: Comparison of the intracoronary
continuous infusion method using a microcatheter and the intravenous continuous adenosine infusion method for inducing maximal hyperemia for fractional flow reserve measurement. Am Heart J 157:1050-1056, 2009
- 국문요약 -
중등도
관상동맥 협착 질환에서 혈관내초음파로 측정된 변수와
심근
분획 혈류 예비력과의 상관 관계
혈관내 초음파는 관상동맥 죽상 경화반 (atheromatous plaque)의 형상 평가, 혈관 내경 및 병변 길이등 형태학적 특성을 평가할 수 있는 좋은 검사법으로 관상동맥 중재 시술 시 많은 도움을 주고 있으나, 심근 허혈을 직접적으로 평가할 수는 없는 검사이다. 심근분획 혈류 예비력 (fractional flow reserve, FFR)은 심근 허혈을 평가하는 침습적 검사법으로, 이를 기준으로 시술 여부를 결정하여 시술한 경우 장기 예후 개선에 도움이 되는 것이 잘 알려져 있다. 본 연구에서는 혈관내 초음파로 얻어진 최소 내경 면적, 병변 길이 등의 값 및 이를 이용하여 계산된 정량적 변수들과, 심근 허혈을 평가하는 심근분획 혈류 예비력과의 상관 관계 및 심근 허혈을 예측하는 혈관 내 초음파의 예측 인자들을 알아보고자 하였다. 환자는 206 명을 대상으로 하였으며, 심근 허혈군 90 명, 심근 허혈이 없는 환자 116 명을 대상으로 하였으며, 의미있는 심근 허혈은 심근분획 혈류 예비력 수치가 0.80 미만인 환자로 정의하였다. 혈관내 초음파로 측정된 최소 내경 면적이 4 mm2이상인 경우 91.4 %에서 심근 허혈은 관찰되지 않았으며, 4 mm2미만인 경우에는 50.9 %에서 심근 허혈이 관찰 되었다. 심근 허혈을 예측하는 혈관 내 초음파 변수로는, 혈관 내 초음파로 측정 된 병변의 길이 (위험도 1.1, p <0.001) 및 혈관 내 최소 내경 면적의 값이 병변의 위치에 따른 기준 값 미만 여부(위험도 7.01, p =0.001)이었다. 또한, 심근분획 혈류 예비력 수치는 혈관 내 초음파로 측정하여 계산된 목표 병변 전체의 죽상 경 화반의 양을 측정한 plaque volume (r= -0.345, p <0.001) 및 전체 혈관에서 죽상 경 화반 양의 비율을 측정한 percent atheroma volume (r= -0.398, p <0.001)과 좋은 음의 상관 관계를 보여 주었다. 또한, 의미있는 심근 허혈을 보인 병변은 (FFR < 0.80), 전체 죽상 경화반의 양 (181.8±82.3 vs. 125.9±77.9 mm3, p<0.001) 및 percent atheroma volume (58.9±5.6 vs. 53.8± 7.9 %, p <0.001) 모두 그 값이 더 많음을 알 수 있었다. 결론적으로, 중등도 협착을 가지는 관상동맥 협착질환에서, 심근 허혈을 평가하 는 검사법인 혈류 분획 예비력 수치는, 혈관내 초음파로 평가한 죽상동맥 경화반 의 양 및 병변의 중증도 (severity)와 관계가 있음을 알 수 있었다. 핵심어 : 혈관내 초음파, 심근분획 혈류 예비력, 죽상 경화반
References
1. Topol EJ and Nissen SE: Our preoccupation with coronary luminology. The dissociation
between clinical and angiographic findings in ischemic heart disease. Circulation 92:2333-2342, 1995
2. Fischer JJ, Samady H, McPherson JA, Sarembock IJ, Powers ER, Gimple LW, Ragosta M: Comparison between visual assessment and quantitative angiography versus fractional flow reserve for native coronary narrowings of moderate severity.Am J Cardiol 90:210-215, 2001 3. Tobis J, Azarbal B, Slavin L: Assessment of intermediate severity coronary lesions in the
catheterization laboratory. J Am CollCardiol 49:839-848, 2007
4. Takagi A, Tsurumi Y, Ishii Y, Suzuki K, Kawana M, Kasanuki H: Clinical potential of
intravascular ultrasound for physiological assessment of coronary stenosis: relationship between quantitative ultrasound tomography and pressure-derived fractional flow reserve.
Circulation100:250–255, 1999
5. Briguori C, Anzuini A, Airoldi F, Gimelli G, Nishida T, Adamian M, Corvaja N, Di Mario C, Colombo A : Intravascular ultrasound criteria for the assessment of the functional significance of intermediate coronary artery stenoses and comparison with fractional flow reserve. Am J Cardiol 87:136–141, 2001
6. Ben-Dor I, Torguson R, Gaglia MA Jr, Gonzalez MA, Maluenda G, Bui AB, Xue Z, Satler LF, Suddath WO, Lindsay J, Pichard AD, Waksman R:Correlation between fractional flow reserve and intravascular ultrasound lumen area in intermediate coronary artery
stenosis.EuroIntervention 7:225-233, 2011
7. Kang SJ, Lee JY, Ahn JM, Mintz GS, Kim WJ, Park DW, Yun SC, Lee SW, Kim YH, Lee CW, Park SW, Park SJ:Validation of intravascular ultrasound-derived parameters with fractional flow reserve for assessment of coronary stenosis severity.Circ Cardiovasc Interv 4:65-71, 2011
8. Koo BK, Yang HM, Doh JH, Choe H, Lee SY, Yoon CH, Cho YK, Nam CW, Hur SH, Lim HS, Yoon MH, Park KW, Na SH, Youn TJ, Chung WY, Ma S, Park SK, Kim HS, Tahk SJ:
Optimal intravascular ultrasound criteria and their accuracy for defining the functional significance of intermediate coronary stenoses of different locations.JACC CardiovascInterv 4:803-811, 2011
9. Nicholls SJ, Hsu A, Wolski K, Hu B, Bayturan O, Lavoie A, Uno K, Tuzcu EM, Nissen SE:Intravascular ultrasound-derived measures of coronary atherosclerotic plaque burden and clinical outcome. J Am Coll Cardiol 55:2399-2407, 2010
10. Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB: A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association.Circulation 51:5–540, 1975
11. Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, Pinto FJ,
RosenfieldK,Siegel RJ, Tuzcu EM, Yock PG:American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents.J Am Coll Cardiol 37:1478-1492, 2001
12. Yoon MH, Tahk SJ, Yang HM, Park JS, Zheng M, Lim HS, Choi BJ, Choi SY, Choi UJ, Hwang JW, Kang SJ, Hwang GS, Shin JH:Comparison of the intracoronary continuous infusion method using a microcatheter and the intravenous continuous adenosine infusion method for inducing maximal hyperemia for fractional flow reserve measurement. Am Heart J157:1050-1056,2009 13. Kolozsvári R, Tar B, Lugosi P, Sánta J, Béres Z, Ungvári T, Polgár P, Kőszegi Z: Plaquevolume
derived from three-dimensional reconstruction of coronary angiography predicts the fractional flow reserve.Int J Cardiol2011 [Epub ahead of print]
14. Seiler C, Kirkeeide RL, Gould KL: Basic structure–function relations of the epicardial coronary vascular tree. Basis of quantitative coronary arteriography for diffuse coronary artery disease.
15. Gould K: Pressure–flow characteristics of coronary stenoses in unsedated dogs at rest and during coronary vasodilation. Circ Res 43:242–253, 1978
16. Spaan J, Piek J, Hoffman J, Siebes M: Physiological basis of clinically used coronaryhemodynamic indices. Circulation 113:446–455,2006
17. Lee CH, Tai BC, Soon CY, Low AF, Poh KK, Yeo TC, Lim GH, Yip J, Omar AR, Teo SG, Tan HC:New set of intravascular ultrasound-derived anatomic criteria for defining functionally significant stenoses in small coronary arteries (results from Intravascular Ultrasound Diagnostic Evaluation of Atherosclerosis in Singapore [IDEAS] study).Am J Cardiol 105:1378-1384,2010
18. Costa MA, Sabate M, Staico R, Alfonso F, Seixas AC, Albertal M, Crossman A, Angiolillo DJ, Zenni M, Sousa JE, Macaya C, Bass TA:Anatomical and physiologic assessments in patients with small coronary artery disease: final results of the Physiologic and Anatomical Evaluation Prior to and After Stent Implantation in Small Coronary Vessels (PHANTOM) trial. Am Heart
J153:296.e1-7, 2007
19. Abizaid A, Mintz GS, Pichard AD, Kent KM, Satler LF, Walsh CL, Popma JJ, Leon MB:Clinical, intravascular ultrasound, and quantitative angiographic determinants of the coronary flow reserve: before and after percutaneous transluminal coronary angioplasty. Am J
Cardiol 82:423–428, 1998
20. Abizaid AS, Mintz GS, Mehran R, Abizaid A, Lansky AJ, Pichard AD, Satler LF, Wu H, Pappas C, Kent KM, Leon MB: Long-term follow-up after percutaneous transluminal coronary angioplasty was not performed based on intravascular ultrasound findings: importance of lumen dimensions.Circulation100:256-261, 1999
21. Kristensen TS, Engstrøm T, Kelbæk H, von der Recke P, Nielsen MB, Kofoed KF: Correlation between coronary computed tomographic angiography and fractional flow reserve. Int J