-Abstract-Altered Findings of Hepatic Arteriography after Radiofrequency Ablation of Hepatocellular Carcinoma: Comparison of Pre-Ablation and Post-Ablation Angiograms
Purpose: To evaluate the altered findings of hepatic arteriography after
radiofrequency (RF) ablation of hepatocellular carcinoma.
Materials and Methods: Twenty-five patients with twenty-seven hepatocellular
carcinomas treated by RF ablation (M: F =23: 2, mean age: 54 years), in which hepatic arteriography was performed before and after RF ablation were evaluated. Patients with any treatment other than RF ablation between the two hepatic arteriograms were excluded. Pre-RF ablation arteriography was performed while performing computed tomography (CT) during arterial portography and CT hepatic angiography. Post-RF ablation arteriography was performed during transcatheter arterial chemoembolization (n=20), or follow up CT during arterial portography and CT hepatic angiography (n=7). The angiograms before and after the RF ablation were evaluated for the altered findings.
Results: The altered findings of hepatic arteriography after RF ablation of the
hepatocellular carcinoma were; arterio-portal shunt, periablational enhancement, varied caliber of the feeding artery to the tumor and occlusion/destruction of an adjacent arterial branch. Residual unablated or local tumor progression could not be visualized in the post-RF ablation arteriography in five of nineteen patients due to arterio-portal shunt or periablational enhancement. The interval from RF ablation to post-RF ablation arteriography was shorter when the tumor could not be visualized (Mann-Whitney test, p=0.026).
Conclusion: The altered findings of hepatic arteriography after RF ablation of
the hepatocellular carcinoma were; arterio-portal shunt, periablational enhancement, varied caliber of the feeding artery and occlusion/destruction of an adjacent arterial branch. The altered findings of may increase the difficulty in performing super-selective transcatheter arterial chemoembolization of the residual
unablated or locally progressed tumor.
Key Words: Radiofrequency ablation Liver neoplasms, therapy
TABLE OF CONTENTS
TITLE PAGE ---1 ABSTRACT ---2 TABLE OF CONTENTS ---4 LIST OF FIGURES ---5 LIST OF TABLES ---8 I. INTRODUCTION ---9II. MATERIALS AND METHODS ---10
A. Patient population ---10 B. RF ablation technique ---11 C. Angiography technique ---11 III. RESULTS ---13 IV. DISCUSSION ---31 V. CONCLUSION ---34 BIBLIOGRAPHY ---35 ---37
LIST OF FIGURES
Fig. 1. A. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. Hepatic arteriogram shows the three staining of hepatocellular carcinoma at right lobe of liver (white arrows)---16
Fig. 1. B. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. CT hepatic angiography shows the two hyper-dense enhancing tumors at segment 7 and 8 (arrows). Another tumor was present at segment 6 (not shown). Two sessions of ultrasonography-guided RF ablation of the tumor at segment 7 was
performed, but was poorly targeted due to the
iso-echogenicity.---17
Fig. 1. C. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. Transcatheter arterial chemoembolization was performed 2 days after the RF ablation, but arterio-portal shunt has developed. The staining of the tumor is embedded within the arterio-portal shunt and is not seen.---18
Fig. 1. D. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. CT scan performed 1 day after transcatheter arterial chemoembolization shows that most of the iodized oil emulsion has bypassed the arterio-portal shunt, and is deposited at subcapsular region. Small amount of iodized oil emulsion is deposited at the tumor of segment 8.---19
Fig. 1. E. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. Four month follow up CT scan shows a newly developed tumor at segment 4 (white arrow head). The tumors at segment 6
and 8 have also progressed.---20
Fig. 2. A. Images of a 44-year-old man with newly developed hepatocellular
carcinoma during follow up of 2 years after RF ablation of hepatocellular carcinoma at segment 8. Early sinusoidal phase hepatic arteriograms show the staining of the tumor at segment 8 (white arrow). Two sessions of ultrasonography-guided RF ablation was performed.---22
Fig. 2. B. Images of a 44-year-old man with newly developed hepatocellular
carcinoma during follow up of 2 years after RF ablation of hepatocellular carcinoma at segment 8. Hepatic arteriogram performed 117 days after the RF ablation shows the periablational enhancement. The tumor staining is embedded within the periablational enhancement and is not seen.---23
Fig. 2. C. Images of a 44-year-old man with newly developed hepatocellular
carcinoma during follow up of 2 years after RF ablation of hepatocellular carcinoma at segment 8. Image of the CT hepatic angiography shows the hyper-dense staining tumor (black arrow) hidden within the periablational enhancement.---24
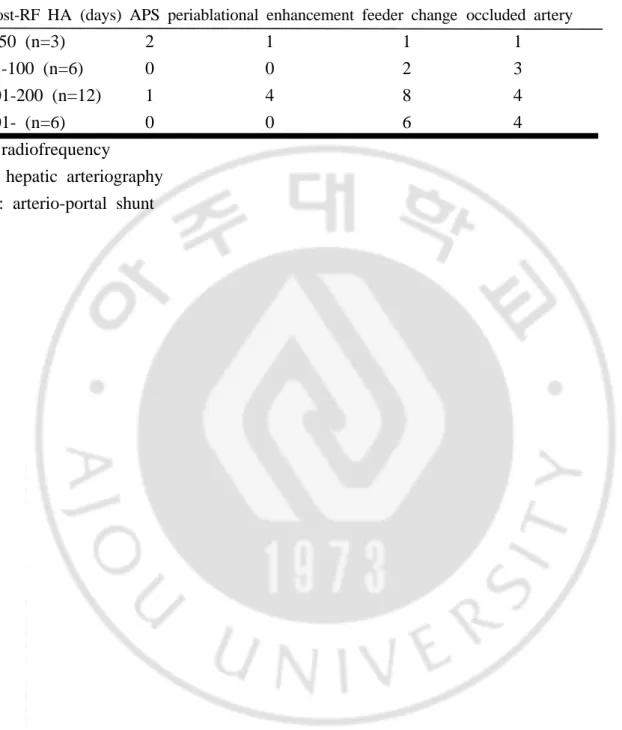
Fig. 3. A. Images of a 75-year-old woman with hepatocellular carcinoma at
segment 6. Arterial phase hepatic arteriograms performed during CT during arterial portography and CT hepatic angiography show the tumor stainging.---26
Fig. 3. B. Images of a 75-year-old woman with hepatocellular carcinoma at
segment 6. Hepatic arteriogram performed 55 days after RF ablation shows the staining of the locally progressed tumor. The feeding artery to the tumor has decreased in caliber (black arrow) compared
to the pre-RF ablation hepatic arteriography.---27
Fig. 4. A. Images of a 48-year-old man with hepatocellular carcinoma at
segment 3. Arterial phase hepatic arteriograms performed during CT during arterial portography and CT hepatic angiography show the tumor stainging at segment 3 (black arrow). Two sessions of ultrasonography-guided RF ablation was performed.---28
Fig. 4. B. Images of a 48-year-old man with hepatocellular carcinoma at
segment 3. Hepatic arteriography during follow up CT during arterial portography and CT hepatic angiography performed 313 days after RF ablation shows no recurrent tumor. Occlusion of an adjacent arterial branch (large black arrow head) and filling of the distal artery (small black arrow heads) by the intra-hepatic collaterals is seen.---29
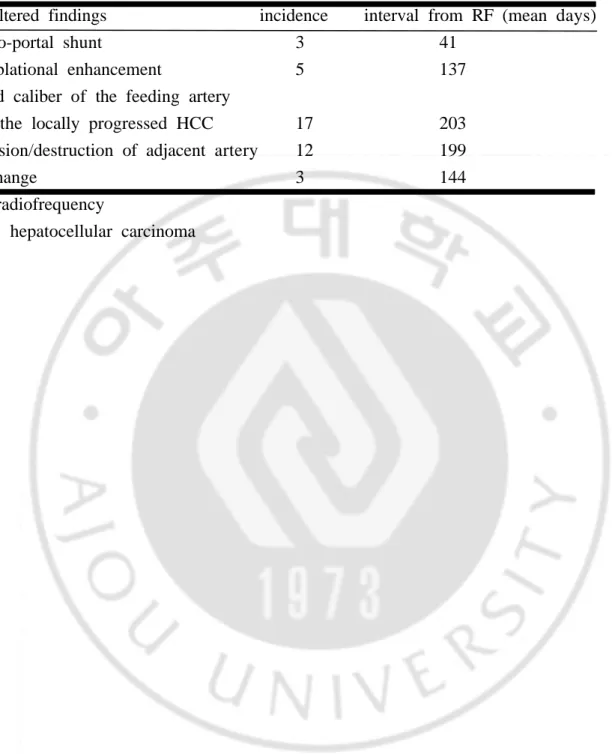
Table 1. Summary of the altered findings of hepatic arteriography after RF
ablation of HCC (N=27).---14
Table 2. Altered findings of hepatic arteriography according to the interval from
RF ablation to post-RF ablation hepatic arteriography. (N=27)---15
Table 3. Characteristics of patients with arterio-portal shunt on post-RF ablation
hepatic arteriography.---21
Table 4. Characteristics of patients with periablational enhancement on post-RF
I. Introduction
The hepatocellular carcinoma is a malignant neoplasm of the liver and commonly occurs in patients with cirrhosis. Surgical resection of the tumor remains the gold standard of therapy, but only 20% are eligible for surgical resection due to the decreased hepatic reserve or the unresectable location (1-4). In these patients with poor hepatic reserve and the hepatocellular carcinoma confined to the liver, minimally invasive therapy is considered as an alternative treatment.
Radiofrequency (RF) ablation and transcatheter arterial chemoembolization are among the widely used minimally invasive techniques in the treatment of the unresectable hepatocellular carcinoma (5-10). The RF ablation produces localized coagulation necrosis of the tumor by the heat induced by the alternating electric current. Transcatheter arterial chemoembolization produces ischemic necrosis of the tumor by selective embolization of the hepatic arterial supply. The transcatheter arterial chemoembolization can be performed before the RF ablation to reduce tumor perfusion and heat loss (11, 12), and the transcatheter arterial chemoembolization can be performed after the RF ablation in the treatment of residual unablated or locally progressed tumor.
The treatment of RF ablation may alter the findings of the hepatic arteriography, which may influence the treatment of transcatheter arterial chemoembolization. The computed tomography (CT) and the ultrasonography findings of the RF ablation zone and the locally progressed tumor after RF ablation have been reported (13-17). The purpose of this study was to evaluate the altered findings of the hepatic arteriography after RF ablation of the hepatocellular carcinoma.
II. Materials and Methods
A. Patient population
We retrospectively evaluated the hepatic arteriograms performed before and after the RF ablation of the hepatocellular carcinoma since August 1999. Since this period, one hundred and eleven patients with hepatocellular carcinoma underwent pre-RF ablation hepatic arteriography while performing CT during arterial portography and CT hepatic angiography as a part of staging work up and preoperative evaluation. In these patients, fifty-three patients underwent RF ablation of the hepatocellular carcinoma due to the inoperability, or the patients refusal for operation.
Among the fifty-three patients, twenty-five patients received RF ablation as the sole treatment of the hepatocellular carcinoma, and post-RF ablation hepatic arteriography was performed during follow up. In two patients, remote intrahepatic recurrence of the tumor developed in a different segment during follow-up, 21 months and 24 months after the first RF treatment respectively. These two patients underwent a second series of treatment of pre-RF ablation hepatic arteriography while performing CT during arterial portography and CT hepatic angiography, treatment of the tumor with RF ablation, and post-RF ablation hepatic arteriography during further follow up. So the twenty-seven hepatocellular carcinomas treated by the RF ablation, in which the pre-RF ablation hepatic arteriography and the post-RF ablation hepatic arteriography were performed were included in the study. Patients with any local or systemic treatment other than the RF ablation between the two hepatic arteriographies were excluded.
Since the hepatic arteriography and the RF ablation were performed during evaluation and treatment of the hepatocellular carcinomas, and since this is a retrospective study, by the policy of our institution, approval by the institutional review board was not required.
The patients were twenty-three males and two females and ranged in ages from 41 years to 75 years (mean, 54 years). All patients had underlying liver
cirrhosis, of which twenty patients were hepatitis B viral carriers, one patient was a hepatitis C viral carrier, three patients had alcoholic liver cirrhosis and one patient had cryptogenic liver cirrhosis. The hepatocellular carcinoma was diagnosed by operation in three, biopsy in nine, elevated alpha-fetoprotein (>400ng/ml) in four, and clinical findings in eleven cases. The radiologic diagnoses of the CT, the hepatic arteriography and the CT during arterial portography and CT hepatic angiography were consistent with hepatocellular carcinoma in all patients. One patient received hepatic segmentectomy and five patients received transcatheter arterial chemoembolization for hepatocellular carcinoma located at a different segment of the liver, prior to the pre-RF ablation hepatic arteriography included in the study.
B. RF ablation technique
The RF ablation of the hepatocellular carcinoma was performed using the internally cooled electrode (Radionics Inc., Burlington, Mass, USA) or using the multitined expandable electrode (Rita Medical Systems, Mountain View, Calif., USA), 1 day to 33 days (mean, 10 days) after the pre-RF ablation hepatic arteriography. One session to five sessions (mean, 1.6 sessions) of RF ablation were performed, percutaneously in twenty-six tumors, and intra-operatively in one tumor.
C. Angiography technique
After the femoral arterial access, selective arteriography of the superior mesenteric artery and the celiac artery in postero-anterior projection, and selective arteriography of the common hepatic artery or the proper hepatic artery in postero-anterior projection and right anterior oblique projection (25-30 degrees) were performed. The arteriography was performed using the digital subtraction angiography technique using a 5-Fr Rosch hepatic catheter (Cook, Bloomington, USA) or a 5-Fr Rosch hepatic H catheter (Cook, Bloomington, USA). On the average, 80-90mL of the iodinated contrast material iodixanol (Visipaque; Nycomed Ireland, Cork, Ireland) was administered for the hepatic arteriography.
The CT during arterial portography and CT hepatic angiography and the transcatheter arterial chemoembolization were performed after the hepatic arteriography. Selective arteriography and CT hepatic angiography of the aberrant hepatic artery was also performed when present.
The pre-RF ablation hepatic arteriography was performed while performing the CT during arterial portography and CT hepatic angiography in all twenty-seven hepatocellular carcinomas. The post-RF ablation hepatic arteriography was performed when residual or recurrent tumor was suspected during follow up. The post-RF ablation hepatic arteriography was performed 2 days to 754 days (mean, 164 days) after the RF ablation, while performing transcatheter arterial chemoembolization in twenty tumors, and follow up CT during arterial portography and CT hepatic angiography in seven tumors. Ten tumors had local tumor progression, nine tumors had both local tumor progression and remote intrahepatic recurrence, and six tumors had only remote intrahepatic recurrence. Two had no evidence of recurrent tumor on hepatic arteriography, CT during arterial portography and CT hepatic angiography and further follow up of 12 months.
The pre-RF ablation hepatic arteriograms and the post-RF ablation hepatic arteriograms were evaluated for the altered findings of the hepatic arteriography after the RF ablation.
III. Results
The altered findings of the hepatic arteriography after the RF ablation of the hepatocellular carcinoma were: the arterio-portal shunt, the periablational enhancement, the varied caliber of the feeding artery to the locally progressed tumor, and the occlusion/destruction of an adjacent arterial branch (Table 1, 2).
The arterio-portal shunt was seen in three of the post-RF ablation hepatic arteriography (11.1%) performed for the residual unablated or locally progressed hepatocellular carcinoma, 2 days to 103 days (mean 41 days) after the RF ablation. The arterio-portal shunt was lobar/segmental in two, and peripheral subsegmental in one. The residual unablated tumor was located within the staining by the arterio-portal shunt and could not be visualized in two post-RF ablation hepatic arteriograms (Fig 1) (Table 3).
The periablational enhancement was seen in five of the post-RF ablation hepatic arteriography (18.5%) performed for the locally progressed or remote intrahepatic recurrent tumors, 50 days to 196 days (mean 137 days) after the RF ablation. The periablational enhancement was completely encircling the ablation zone in two and partially encircling the ablation zone in three. The locally progressed tumor was located within the periablational enhancement and could not be visualized in three of the post-RF ablation hepatic arteriograms (Fig 2) (Table 4).
The feeding artery to the hepatocellular carcinoma could be identified in twenty cases of the pre-RF ablation hepatic arteriography, and varied caliber of the feeding artery to the locally progressed tumor was seen in seventeen of the post-RF ablation hepatic arteriograms (63.0%). The feeding artery disappeared in the two without local tumor progresssion, decreased in caliber in eleven when the locally progressed tumor was smaller in size than the index tumor (Fig 3), and increased in caliber in four when the locally progressed tumor was larger in size than the index tumor.
Occlusion/destruction of an adjacent subsegmental arterial branch was seen in twelve post-RF ablation hepatic arteriography (Fig 4) (44.4%).
Table 1. Summary of the altered findings of hepatic arteriography after RF
ablation of HCC (N=27).
the altered findings incidence interval from RF (mean days)
arterio-portal shunt 3 41
periablational enhancement 5 137
varied caliber of the feeding artery
to the locally progressed HCC 17 203
occlusion/destruction of adjacent artery 12 199
no change 3 144
RF: radiofrequency
Table 2. Altered findings of hepatic arteriography according to the interval from
RF ablation to post-RF ablation hepatic arteriography. (N=27)
interval from RF arteriographic findings
to post-RF HA (days) APS periablational enhancement feeder change occluded artery
0-50 (n=3) 2 1 1 1
51-100 (n=6) 0 0 2 3
101-200 (n=12) 1 4 8 4
201- (n=6) 0 0 6 4
RF: radiofrequency
HA: hepatic arteriography APS: arterio-portal shunt
Fig. 1. A. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. Hepatic arteriogram shows the three staining of hepatocellular carcinoma at right lobe of liver (white arrows).
Fig. 1. B. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. CT hepatic angiography shows the two hyper-dense enhancing tumors at segment 7 and 8 (arrows). Another tumor was present at segment 6 (not shown). Two sessions of ultrasonography-guided RF ablation of the tumor at segment 7 was performed, but was poorly targeted due to the iso-echogenicity.
Fig. 1. C. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. Transcatheter arterial chemoembolization was performed 2 days after the RF ablation, but arterio-portal shunt has developed. The staining of the tumor is embedded within the arterio-portal shunt and is not seen.
Fig. 1. D. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. CT scan performed 1 day after transcatheter arterial chemoembolization shows that most of the iodized oil emulsion has bypassed the arterio-portal shunt, and is deposited at subcapsular region. Small amount of iodized oil emulsion is deposited at the tumor of segment 8.
Fig. 1. E. Images of a 45-year-old man with three hepatocellular carcinomas in
right lobe. Four month follow up CT scan shows progression of the tumor in segment 8. The tumor in segment 6 also progressed and a new tumor developed in segment 4 (not shown).
Table 3. Characteristics of patients with arterio-portal shunt on post-RF ablation
hepatic arteriography.
stainging of HCC patient recurrence interval from RF (days) degree of shunt on arteriography
1 l and r 2 lobar not detected
2 l 17 segmental not detected
3 l 103 subsegmental detected
RF; radiofrequency
l; local progression of hepatocellular carcinoma
Fig. 2. A. Images of a 44-year-old man with newly developed hepatocellular
carcinoma during follow up of 2 years after RF ablation of hepatocellular carcinoma at segment 8. Early sinusoidal phase hepatic arteriograms show the staining of the tumor at segment 8 (white arrow). Two sessions of ultrasonography-guided RF ablation was performed.
Fig. 2. B. Images of a 44-year-old man with newly developed hepatocellular
carcinoma during follow up of 2 years after RF ablation of hepatocellular carcinoma at segment 8. Hepatic arteriogram performed 117 days after the RF ablation shows the periablational enhancement. The tumor staining is embedded within the periablational enhancement and is not seen.
Fig. 2. C. Images of a 44-year-old man with newly developed hepatocellular
carcinoma during follow up of 2 years after RF ablation of hepatocellular carcinoma at segment 8. Image of the CT hepatic angiography shows the hyper-dense staining tumor (black arrow) hidden within the periablational enhancement.
Table 4. Characteristics of patients with periablational enhancement on post-RF
ablation hepatic arteriography.
stainging of HCC patient recurrence interval from RF (days) enhancement on arteriography
a l 50 circular not detected
b l 117 circular not detected
c l and r 160 partial not detected
d l and r 162 partial detected
e l 196 partial detected
RFA; radiofrequency ablation HCC; hepatocellular carcinoma
l; local progression of hepatocellular carcinoma
Fig. 3. A. Images of a 75-year-old woman with hepatocellular carcinoma at
segment 6. Arterial phase hepatic arteriograms performed during CT during arterial portography and CT hepatic angiography show the tumor stainging.
Fig. 3. B. Images of a 75-year-old woman with hepatocellular carcinoma at
segment 6. Hepatic arteriogram performed 55 days after RF ablation shows the staining of the locally progressed tumor. The feeding artery to the tumor has decreased in caliber (black arrow) compared to the pre-RF ablation hepatic arteriography.
Fig. 4. A. Images of a 48-year-old man with hepatocellular carcinoma at
segment 3. Arterial phase hepatic arteriograms performed during CT during arterial portography and CT hepatic angiography show the tumor stainging at segment 3 (black arrow). Two sessions of ultrasonography-guided RF ablation was performed.
Fig. 4. B. Images of a 48-year-old man with hepatocellular carcinoma at
segment 3. Hepatic arteriography during follow up CT during arterial portography and CT hepatic angiography performed 313 days after RF ablation shows no recurrent tumor. Occlusion of an adjacent arterial branch (large white arrow head) and filling of the distal artery (small white arrow heads) by the intra-hepatic collaterals is seen.
No identifiable change at the region of the ablation zone except disappearance of the staining of the index hepatocellular carcinoma was seen in three of the post-RF ablation hepatic arteriography (11.1%).
Among the nineteen hepatocellular carcinomas with local tumor progression, the staining of the tumor could not be visualized in five cases (26.3%). They were due to the arterio-portal shunt in two and periablational enhancement in three. The interval from the RF ablation to the post-RF ablation hepatic arteriography was shorter in cases when the locally progressed tumor could not be visualized (2 days to 160 days, mean, 69 days), compared to the interval of the cases when the locally progressed tumor could be localized (55 days to 754 days, mean, 190 days) (Mann-Whitney test, p=0.026).
IV. Discussion
RF ablation is a thermal ablation procedure and produces localized and controlled tumor destruction. Alternating electric current conducted by an electrode produces local ionic agitation and subsequent friction heat, resulting in coagulation necrosis. It is usually performed in primary or secondary hepatic malignancies of 5cm or smaller, four or fewer, and without extra-hepatic tumor (10). Transcatheter arterial chemoembolization produces ischemic necrosis of the tumor by the selective embolization of the hepatic arterial supply. Transcatheter arterial chemoembolization has the capability of treating the entire liver and can be performed irrespective of the size and the location of the hepatocellular carcinoma. So transcatheter arterial chemoembolization can be performed before the RF ablation of the hepatocellular carcinoma to reduce tumor perfusion and heat loss (11, 12), and the transcatheter arterial chemoembolization can be performed after the RF ablation when the local tumor progression or remote intrahepatic recurrence has occurred. The procedure of RF ablation resulted in various alterations in the angiographic findings, which may affect the procedure of trancatheter arterial chemoembolization.
The arterio-portal shunt may develop spontaneously in a cirrhotic liver due to the structural distortions, due to the hepatocellular carcinoma, or iatrogenically along the path of a biopsy needle after a liver biopsy procedure. The frequency of the arterio-portal shunt after puncturing the liver with a needle depended on the interval between the needle puncture and the hepatic arteriography, as high as 50% within the first week and less than 10% after the first week (18). The arterio-portal shunt tended to close spontaneously in time. The arterio-portal shunt also occurred after the RF ablation procedure. The arterio-portal shunt induced by the RF ablation procedure has also closed spontaneously in time, explaining the low incidence, and with relative high incidence of more extensive, lobar or segmental arterio-portal shunts early after the RF ablation (Table 3).
It is not certain whether the arterio-portal shunt which occurred after RF ablation have been induced by the procedure of puncturing with a RF electrode
or by the thermal injury of the RF ablation. However, the staining of the hepatocellular carcinoma at the margin or adjacent to the ablation zone can be hidden within the staining of the arterio-portal shunt, and localization for super-selective transcatheter arterial chemoembolization will be difficult. Furthermore, the iodized oil/doxorubicin emulsion will bypass the arterio-portal shunt and selective uptake by the hepatocellular carcinoma will be prohibited (Fig 1).
The periablational enhancement seen in the contrast enhanced CT correlated with a rim constituting of a mixture of viable hepatic parenchyma, necrosis, and hemorrhage (13). The enhancement was hyper-attenuating in the arterial phase, and differentiation from the locally progressed hepatocellular carcinoma was difficult (17). The frequency of the periablational enhancement also depended upon the interval from the RF ablation to the CT, and persisted as long as six months after the RF ablation (17). Differentiating the locally progressed hepatocellular carcinoma from the surrounding periablational enhancement on hepatic arteriography was also difficult (Fig 2) and precise localization for the super-selective transcatheter arterial chemoembolization was not possible. The periablational enhancement also persisted as long as 196 days after RF ablation in the hepatic arteriograms.
The caliber of an artery will vary with the arterial demand of the tissue the artery is supplying. When the size of the locally progressed hepatocellular carcinoma of the post-RF ablation hepatic arteriography has varied compared to the index tumor, the caliber of the feeding artery will also vary (Fig 3). The advances of the quality of the microcatheters manufactured recently have made super-selective transcatheter arterial chemoembolization feasible, and most feeding arteries to the hepatocellular carcinomas can be easily super-selected. But the decreased caliber of a feeding artery to a hepatocellular carcinoma will increase the difficulty of super-selective transcatheter arterial chemoembolization, especially when fine collaterals are feeding the hepatocellular carcinoma.
When RF ablation of a hepatic malignancy is performed, some amount of the normal liver parenchyma adjacent to the tumor is also ablated to acquire the
ablative margin of 0.5 to 1 cm. There is a high possibility that a subsegmental artery adjacent to the tumor will be supplying the normal liver parenchyma adjacent to the tumor, especially at subcapsular region. Occlusion of a subsegmental artery adjacent to a subcapsular hepatocellular carcinoma after RF ablation may have resulted from direct thermal injury by the RF ablation, or the diminished demand by the liver parenchyma adjacent to the hepatocellular carcinoma. Occlusion of a subsegmental artery in a deep region of the liver parenchyma was seen in one case. Intra-hepatic collaterals were supplying the liver parenchyma distal to the occluded artery (Fig 4). When a recurrent hepatocellular carcinoma has occurred distal to an occluded artery deep in the liver parenchyma, it will also be supplied by the intra-hepatic collaterals, which will increase the difficulty of super-selective transcatheter arterial chemoembolization.
There are some limitations in the results of our study. The study was retrospectively designed and is descriptive. Hepatocellular carcinomas were pathologically diagnosed in only twelve patients. Locally progressed or remote intrahepatic recurrent hepatocellular carcinomas after RF ablation were radiologically diagnosed, but not pathologically diagnosed. The post-RF ablation hepatic arteriography was performed only when recurrent hepatocellular carcinoma was suspected on follow up liver CT scans resulting in a selection bias and the number of hepatic arteriography within 3 months from RF ablation is small. The arterio-portal shunt may have been induced by the RF electrode, but not by the thermal injury of the RF ablation. And the changes of the portal vein and the hepatic vein could not be evaluated.
V. CONCLUSION
In conclusion, the altered findings of hepatic arteriography after RF ablation of the hepatocellular carcinoma were: arterio-portal shunt, periablational enhancement, varied caliber of the feeding artery to the locally progressed hepatocellular carcinoma, and occlusion of an adjacent subsegmental artery. The arterio-portal shunt and the periablational enhancement may hide the staining of a residual unablated hepatocellular carcinoma or locally progressed hepatocellular carcinoma adjacent to the ablation zone when the interval from the RF ablatin to the post-RF ablation hepatic arteriography is short. The altered findings of hepatic arteriography after RF ablation will increase the difficulty in performing super-selective transcatheter arterial chemoembolization of the locally progressed hepatocellular carcinoma or recurrent hepatocellular carcinoma after RF ablation due to the arterio-portal shunt, the poorly defined margin by the periablational enhancement, decreased caliber of the feeding artery, or by development of the intrahepatic collateral feeding arteries.
BIBLIOGRAPHY
1. Steele G Jr, Ravikumar TS. Resection of hepatic metastasis from colorectal cancer: biological perspective. Ann Surg 1989; 210:127-138 2. Gayowski TJ, Iwatsuki S, Madariaga JR, et al. Experience in hepatic
resection for metastatic colorectal cancer: analysis of clinical and pathologic risk factors. Surgery 1994; 116:703-711
3. Arii S, Okamoto E, Imamura M. Registries in Japan: current status of hepatocellular carcinoma in Japan. Liver Cancer Study Group of Japan. Semin Surg Oncol 1996; 12:204-211
4. Cady B, Jenkins RL, Steele GD Jr, et al. Surgical margin in hepatic resection for colorectal metastasis: a critical and improvable determinant of outcome. Ann Aurg 1998;227:566-571
5. Nakamura H, Hashimoto T, Oi H, Sawada S. Transcatheter oily chemoembolization of the hepatocellular carcinoma. Radiology 1989; 170:783-786
6. Uchida H, Ohishi H, Matsuo N, et al. Transcatheter hepatic segmental arterial embolization using lipiodol mixed with an anticancer drug and gelfoam particles for hepatocellular carcinoma. Cardiovasc Intervent Radiol 1990; 13:140-145
7. Libraghi T, Goldberg SN, Lazzaroni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radiofrequency ablation versus ethanol injection. Radiology 1999; 210:661-665
8. Wood TF, Rose DM, Chung M, Allegra DP, Foshag LJ, Bilchik AJ. Radiofrequency ablation of 231 unresectable hepatic tumors: indications, limitations, and complications. Ann Surg Oncol 2000; 7:593-600
9. Curley SA, Izzo F, Ellis LM, Nicolas Vauthey J, Vallone P. Radiofrequency ablation of hepatocellular cancer in 110 patients with cirrhosis. Ann Surg 2000; 232:381-391
10. Dodd GD III, Soulen MC, Kane RA, et al. Minimally invasive treatment of malignant hepatic tumors: at the threshold of a major breakthrough.
Radiographics 2000; 20:9-27
11. Rossi S, Garbagnati F, Lencioni R, et al. Percutaneous radio-frequency thermal ablation of nonresectable hepatocellular carcinoma after occlusion of tumor blood supply. Radiology 2000; 217:119-126
12. Lencioni R, Cioni D, Donati F, Bartolozzi C. Combination of interventional therapies in hepatocellular carcinoma. Hepatogastroenterology 2001; 48:8-14
13. Raman SS, Lu DS, Vodopich DJ, Sayre J, Lassman C. Creation of radiofrequency lesions in a porcine model: correlation with sonography, CT and histopathology. AJR Am J Roentgenol 2000; 175:1253-1258
14. Chopra S, Dodd GD III, Chintapalli KN, Leyendecker JR, Karahan OI, Rhim HC. Tumor recurrence after radiofrequency thermal ablation of hepatic tumors: spectrum of findings on dual-phase contrast enhanced CT. AJR Am J Roentgenol 2001; 177:381-387
15. Catalano O, Lobiance R, Exposito M, Siani A. Hepatocellular carcinoma recurrence after percutaneous ablation therapy: helical CT patterns. Abdom Imaging 2001; 26:375-383
16. Cioni D, Lencioni R, Rossi S et al. Radiofrequency thermal ablation of hepatocellular carcinoma: using contrast-enhanced harmonic power doppler sonography to assess treatment outcome. AJR Am J Roentgenol 2001; 177:783-788
17. Tsuda M, Majima K, Yamada T, Saitou H, Ishibashi T, Takahashi S. Hepatocellular carcinoma after radiofrequency ablation therapy: dynamic CT evaluation of treatment. Clin Imaging 2001; 25:409-415
18. Hellekant CH. Vascular complications following needle puncture of the liver. Acta Radiol [Diagn] (Stockh) 1976;17:209-222