Etiologies and Predictors of ST-Segment Elevation Myocardial Infarction
전체 글
수치
관련 문서
However, the present study showed that four components of the BSS (cough, sputum, dyspnea, and chest pain) were improved more with HL301 treat- ment than with placebo
In elderly metastatic colon cancer patients, the treatment results of combination therapy with targeted treatment showed similar results to those reported in clinical trials
Gait status and lower extremity strength cannot be prop- erly evaluated in patients with hip fractures due to their pain and loss of walking ability at the time of injury.
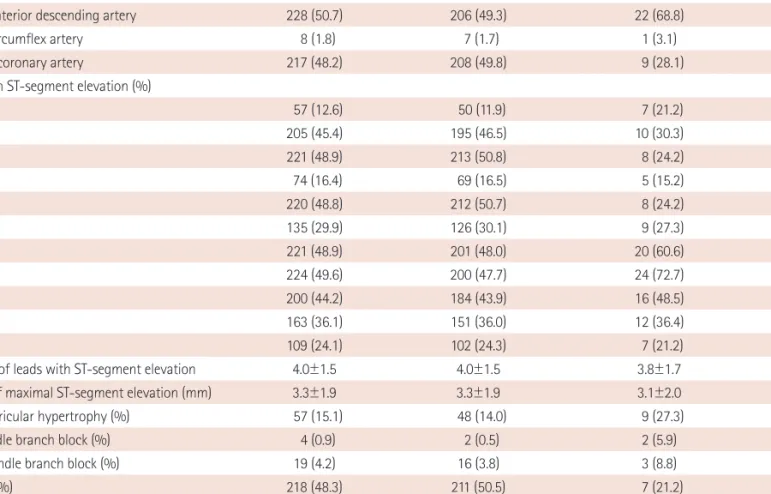
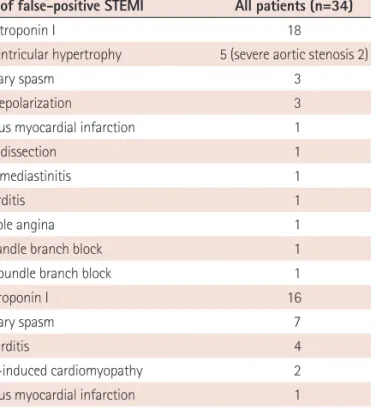
STEMI, ST segment elevation myocardial infarction; CURRENT/OASIS-7, Clopidogrel Optimal Loading Dose Usage to Reduce Recurrent EveNTs/Optimal Antiplatelet Strategy
Grines et al., “Angiographic and clinical characteristics associated with increased in- hospital mortality in elderly patients with acute myocardial infarction
The purpose of this study is to evaluate whether the 30-day mortality rate in hospitalization of patients with acute myocardial infarction (AMI), ischemic stroke (IS),
To date, no large-scale study has compared the clinical and angiographic predictors of cardiovascular events in patients with left main bifurcation (LMB) and non-LMB
경찰행정학과 관광학부 보건의료계열 컴퓨터공학부 건축토목공학부 화학공학부 레포츠과학부.. 또한 디자인 패턴 기반의 소프트웨어 개발 실습을 통해 이론 뿐