관련 문서
Method : : : : We evaluate clinical features of 714 Korean vitiligo patients who lived in the Gwangju chonnam province(315 males and 399 females).. Results
Drug-intoxicated patients were predominantly male, with the highest incidence of intoxication among patients above the seventh decade of age(21.5%) and the
Materials and methods: In 37 patients (20 men, 17 women; mean age: 52.65 ± 8.19 years [range: 37∼72 years]), anorganic bovine bone (ABB, n = 16), mineralized cancellous
Abstract: This study was aimed to investigate the adhesion control standards of pain relieving patch (PRP) drugs and to survey it′s adverse effects on the skin of patients
Purpose: This study was performed to identify the association between family support, ADL and depression among hospitalized older patients with chronic
Comparison of pain scale between the conventional and 2-step needle insertion technique according to the injection area ··· 11... The combination of pain scale and
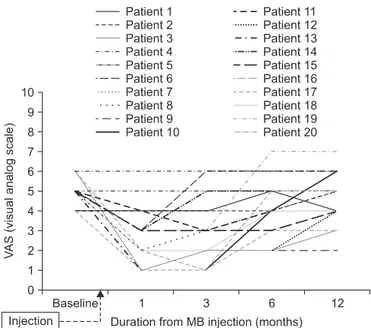
Lumbar discogenic radiculopathy (LDR) is one of the most common spinal disorders which can lead to high medical expenses for the patient, occupational impairment,
Baseline characteristics of genotype 1b chronic hepatitis C patients who treated with daclatasvir and asunaprevir (n=231)... Characteristics of genotype 1b