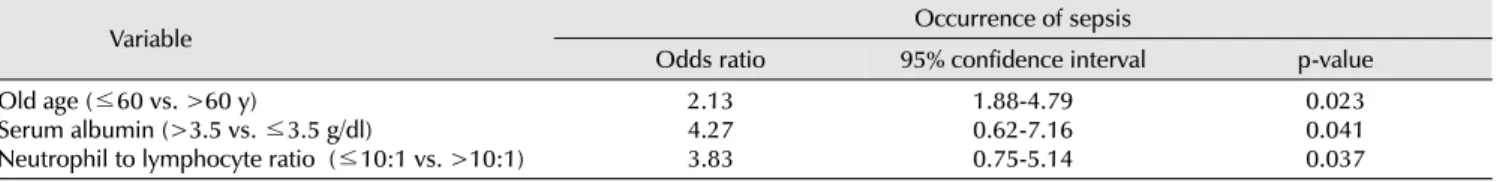
Risk Factors of Sepsis in Obstructive Acute Pyelonephritis Associated with Urinary Tract Calculi
전체 글
수치
관련 문서
Purpose: We investigated recent aspects of causative organism and antimicrobial susceptibility of urinary tract infections(UTI).. Materials and Methods:
Serum uric acid levels and risk for vascular disease in patients with metabolic syndrome... Prevalence if the metabolic syndrome in a Turkish
For my study, this being diagnosed with prostate cancer receiving treatment in patients with complementary and alternative therapies for their experience
(Background) Gallbladder wall thickening(GWT) and gallbladder contraction are often observed in patients with acute hepatitis.. The incidence of acute hepatitis A
Pelvic floor muscle training versus no treatment for urinary incontinence in women.. Acute back pain: a control-group comparison of behavioral vs
The risk of complicated acute appendicitis should be evaluated in terms of medical factors, including psychi- atric disease entity, psychotropic prescription, and
Undiagnosed malignancy in patients with deep vein thrombosis: incidence, risk indicators, and diagnosis.. Monreal M, Fernandez-Llamazares J, Perandreu
A Retrospective Study of Prevalence and Risk factors for Neonatal Occipital