J Korean Soc Transplant | www.ksot.org 85 June 2009 | Volume 23 | Issue 1 책임저자:서경석, 서울시 종로구 연건동 28
서울대학교 의과대학 외과학교실, 110-744 Tel: 02-2072-3789, Fax: 02-2072-3975 E-mail: kssuh@plaza.snu.ac.kr 2008년 대한이식학회 추계학술대회에서 구연되었음.
접수일 : 2009년 5월 27일, 게재승인일 : 2009년 6월 25일 J Korean Soc Transplant | 2009;23:85-88
Case Report
Living Donor Liver Transplantation (LDLT) using Monosegment Graft for a Small Infant
Departments of Surgery
1, Plastic Surgery
2, Seoul National University College of Medicine, Seoul, Korea
Kyung-Suk Suh, M.D.
1, Taehoon Kim, M.D.
1, Woo Young Shin, M.D.
1, Nam-Joon Yi, M.D.
1, Kyung Won Min, M.D.
2and Kuhn Uk Lee, M.D.
1작은 유아에게 시행된 단일 분절 이식편을 이용한 생체 간이식
서경석1ㆍ김태훈1ㆍ신우영1ㆍ이남준1ㆍ민경원2ㆍ이건욱1 서울대학교 의과대학 외과학교실1 및 성형외과학교실2
A 1.5-month-old girl, weighing 4.7 Kg, presented with vomiting, blood tinged stool and jaundice. We performed living donor liver transplantation(LDLT) for the management of fulminant hepatic failure with worsening encephalopathy. The donor was her father, 30 years old, weighing 51 kg. During the pre-operative donor evaluation, a computed tomography volumetry was 170 mL for left lateral section of the liver, which was 3.61% of the graft-recipient weight ratio(GRWR). In donor oper- ation, the reduction of the left lateral section was made just after parenchyma resection of left lateral section was completed, and before clamping of the vessels. The segment II was resected from the left lateral section in situ. The transection plane between segment II and III was identified with the use of intraoperative ultrasonography and clamping of Glisson of segment II. The segment III graft weighed 135 g, which was 2.87 % GRWR. The operation time was 6 hours 15 minutes and transfusion was not needed. Recipient operation was performed in conventional manner of pediatric LDLT using left lateral section with primary closure of abdominal wall without tension. The operation time was 7 hours 35 minutes and cold ischemic time was 1 hour 33 minutes. She recovered well without any significant complications. She discharged on the post operative 24th day. Total bilirubin, aspartic acid transaminase and alanine aminotransferase was 0.6 mg/dL, 26 IU/L and 37 IU/L respectively at the point of discharge. LDLT with monosegment seems to be a feasible option for neonates and small infants requiring liver transplantation.
Key Words: Monosegment, Living donor liver transplantation, Infant 중심 단어: 단일 분절 이식편, 생체 간이식, 유아
INTRODUCTION
Children below 2 years of age have the highest in- cidence of end-stage liver disease in children and 80%
of pediatric deaths are caused by liver diseases.(1) The shortage of organ donors for low-weight liver transplant recipients, especially neonates or small in- fants, has led to the development of new surgical
techniques to increase the donor pool.(1,2) The left
lateral section graft (Couinaud’s segment II and III)
has been used to overcome size discrepancies be-
tween adult donors and pediatric recipients. For small
infants weighing less than 5 kg, however, problems
related to a large-for-size graft are sometimes encoun-
tered even when using the left lateral section graft.(3)
The main problems associated with large-for-size grafts
are the small size of the abdominal cavity in the recip-
ient and the inability to provide sufficient blood sup-
ply to the graft.(4) The reduced lateral section, mono-
segment, or reduced monosegment grafts have recently
been introduced to address these problems.(3,5,6) We
report herein our recent case experience using mono-
Kyung-Suk Suh, et al: LDLT using Monosegment Graft
J Korean Soc Transplant | www.ksot.org 86 June 2009 | Volume 23 | Issue 1
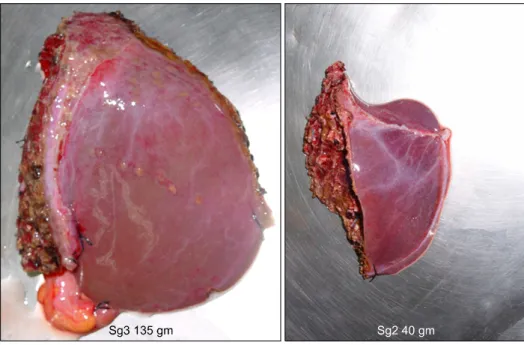
Fig. 1. The photography of the procured graft.
segment graft from a living donor that was reduced in situ for a small infant recipient.
CASE REPORT
The recipient was a 1.5-month-old girl, weighing 4.7 Kg, with the preemptive diagnosis of tyrosinemia.
She presented with vomiting, blood tinged stool and worsening jaundice. She was hospitalized into the in- tensive care unit (ICU) and conservative management was started. But, Jaundice and hepatic failure progressed rapidly in spite of 2-nitro-4-(triflouromethyl)benzoyl-1, 3-cyclohexanedione (NTBC) medication. Eventually, she was consulted to the transplantation team as a candi- date of urgent transplantation for the management of fulminant hepatic failure with comatous encephalo- pathy. Total bilirubin was 19.0 mg/dL and pro- thrombin time international normalized ratio (PT INR) was 4.53 at the point of operation.
The donor was her father. He was 30 years old, weighing 51 kg and had no relevant past medical history. During the pre-operative donor evaluation, a computed tomography volumetry was 170 mL for left lateral section of the liver, which was 3.61% of the re- cipient weight GRWR.
1) Donor surgery
The standard transverse and midline abdominal in- cision was used. After the quality of the liver and the size of the left lobe had been evaluated, the routine procedure of left lateral sectionectomy of living donor was performed. Using an ultrasonic surgical aspirator, the hepatic parenchyma was transected without any vascular clamping. The parenchymal transection line is just right side of the umbilical part of the portal vein.
After the size of left lateral section was checked, the reduction of the left lateral sectionwas made just after the first parenchyma resection was completed.The seg- ment II was resected from the left lateral section in situ. The transection plane between segment II and III was identified with clamping of Glisson pedicle of segment II and the main venous outflow of left hep- atic vein was identified with intraoperative ultra- sonography (Fig. 1∼3). The resected segment II was 40.5 g and was sent for pathologic study. After fix- ation it measured 9.5×5×2 cm.
The left hepatic artery, the left portal vein, and left
hepatic vein were clamped and divided. The segment
III was flushed with HTK preservation solution on the
back table. The segment III graft weighed 135 g,
which was 2.87% GRWR. The operation time was 6
hours 15 minutes and transfusion was not needed.
Kyung-Suk Suh, et al: LDLT using Monosegment Graft
J Korean Soc Transplant | www.ksot.org 87 June 2009 | Volume 23 | Issue 1
Fig. 2. Schematic drawing of the resection plane in monoseg- ment graft.
Fig. 3. Discolorization of S2 is shown after the clamping the Glisson of S2 (transaction of left lateral section was already per- formed).
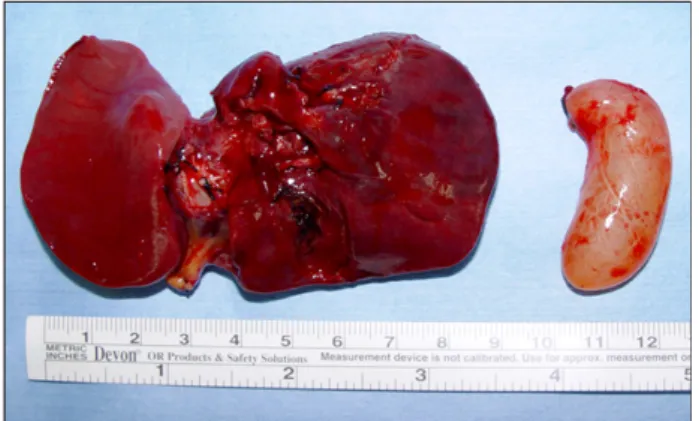
Fig. 4. Native liver (total hepatectomy was performed-weigh- ing 45 g).
2) Recipient surgery
After the standard transverse and midline abdominal incision, the abdominal cavity exploration showed minimal ascites. The hepatectomy was performed with vena cava preservation. The native liver was markedly shrunken weighed 45 g (Fig. 4). The hepatic vein anastomosis was performed with donor left hepatic vein being attached to the common orifice of the re- cipient right, middle and left hepatic veins. The portal vein anastomosis was performed between the graft left portal vein and the recipient main portal vein. After the portal vein anastomosis was performed, the clamps were removed and the liver was re-perfused. The hep-
atic artery anastomosis was performed between the graft left hepatic artery and the recipient common hepatic artery by the branch patch technique, creating a patch from the right and left hepatic arteries of the recipient using 10/0 Nylon interrupted sutures under the operating microscope. The bile duct anastomosis was performed by Roux-en Y retrocolic hepatico- jejunostomy. There was no tension following closure of the abdominal wall. The operation time was 7 hours 35 minutes and cold ischemic time of the graft was 1 hour 33 minutes.
3) Post-operative hospital course
She recovered well without any significant complica- tions. Diet was started on the post operative 6th day.
She stayed at ICU for 11 days postoperatively and was moved to the pediatric ward. She discharged on the post operative 24th day.
The ultrasonic liver Doppler scan performed regu- larly showed normal flow pattern of intrahepatic artery and no significant stenosis of the portal vein and hep- atic vein throughout the hospital course. Total bilir- ubin, PT INR, aspartic acid transaminase and alanine aminotransferase was 0.6 mg/dL, 1.09, 26 IU/L and 37 IU/L respectively at the point of discharge.
Discussion
Because donor availability has been the rate-limiting
step in pediatric liver transplantation, new techniques
have been developed to increase the donor supply for
Kyung-Suk Suh, et al: LDLT using Monosegment Graft
J Korean Soc Transplant | www.ksot.org 88 June 2009 | Volume 23 | Issue 1
children. In some small infants and neonates, the left lateral section can cause the large-for-size graft syn- drome. The problems of large-for-size graft are the in- sufficient blood supply to the revascularized graft and the small size of the recipient's abdominal cavity, with graft compression and subsequent poor tissue oxyge- nation.(7) Avoiding the use of synthetic mesh and sec- ondary closure can also reduce the chance of compli- cations. Prior to the year 2000, there were no reports of LDLT using monosegment graft. Santibanes et al.
reported two cases of LDLT using monosegment graft for the first time.(8) To the best of our knowledge, this is the first report of LDLT using monosegment graft reduced in situ in Korea and also the above de- scribed patient is the youngest liver transplantation re- cipient with the lowest body weight in Korea. Kasa- hara et al. already provided a positive evidence that good operative and survival outcomes can be achieved by using monosegment liver grafts from live donors, even though their incidence of vascular complication was relatively high (20%) and their number of patients was small (n=10).(9) Recently, Ogawa et al. have re- ported the feasible results of LDLT with reduced mon- osegment grafts for neonates and small infants.(3) They reported that for neonates and extremely small infants with relative much bigger donors, further re- duction to a reduced monosegment was required. If the estimated GRWR of the left lateral section is more than 4% on pre-operative volumetry, a further graft re- duction could be necessary to overcome the large-for- size graft syndrome. Enne et al. concluded in their meta-analysis that LDLT using monosegment seems to be as safe as standard pediatric LDLT using left lateral section and the survival was comparable.(7)
In summary, we report the first case of LDLT using
monosegment in Korea. LDLT with monosegment seems to be a feasible option for neonates and small infants requiring liver transplantation.
REFERENCES
1) Broelsch CE, Emond JC, Whitington PF, Thistlethwaite JR, Baker AL, Lichtor JL. Application of reduced-size liver transplants as split grafts, auxiliary orthotopic grafts, and living related segmental transplants. Ann Surg 1990;212:
368-75.
2) Ozawa K, Uemoto S, Tanaka K, Kumada K, Yamaoka Y, Kobayashi N, et al. An appraisal of pediatric liver trans- plantation from living relatives. Initial clinical experiences in 20 pediatric liver transplantations from living relatives as donors. Ann Surg 1992;216:547-53.
3) Ogawa K, Kasahara M, Sakamoto S, Ito T, Taira K, Oike F, et al. Living donor liver transplantation with reduced monosegments for neonates and small infants. Transplan- tation 2007;83:1337-40.
4) Kiuchi T, Kasahara M, Uryuhara K, Inomata Y, Uemoto S, Asonuma K, et al. Impact of graft size mismatching on graft prognosis in liver transplantation from living donors.
Transplantation 1999;67:321-7.
5) Srinivasan P, Vilca-Melendez H, Muiesan P, Prachalias A, Heaton ND, Rela M. Liver transplantation with monoseg- ments. Surgery 1999;126:10-2.
6) de Santibanes E, McCormack L, Mattera J, Pekolj J, Sivori J, Beskow A, et al. Partial left lateral segment transplant from a living donor. Liver Transpl 2000;6:108-12.
7) Enne M, Pacheco-Moreira L, Balbi E, Cerqueira A, Santa- lucia G, Martinho JM. Liver transplantation with mono- segments. Technical aspects and outcome: a meta-analysis.
Liver transpl 2005;11:564-9.
8) Enne M, Pacheco-Moreira LF, Cerqueira A, Balbi E, Halpern M, Luiz Pereira J, et al. Liver transplantation with monosegment from a living donor. Pediatr Transplant 2004;8:189-91.
9) Kasahara M, Uryuhara K, Kaihara S, Kozaki K, Fujimoto Y, Ogura Y, et al. Monosegmental living donor liver trans- plantation. Transplant Proc 2003;35:1425-6.