Ⅰ. INTRODUCTION
Glandular odontogenic cyst (GOC) is a rare odontogenic cyst which has been proposed as a distinct entity by Gardener et al. in 19881). GOC is characterized by a potentially aggressive behavior with a high recurrence rate,2,3) and therefore an accurate diagnosis is critical for treatment and follow-up. However, due to similar histopathological features between GOC and other lesions such as botryoid odontogenic cyst, dentigerous cyst with
mucous metaplasia or central mucoepidermoid carcinoma, the differential diagnosis can be challenging.4)
In a review of English language literature, Kaplan et al.4) have proposed a set of major and minor criteria for histological diagnosis of GOC. Fowler et al.5) have presented similar, but not identical, microscopic parameters for differential diagnosis between GOC and GOC mimickers. In addition to microscopic features, Macdonald-Jankowski6) evaluated the clinical and radiological features of GOC, which can help distinguish GOC from other cystic lesions, through systematic review.
To date, case series of GOC have been studied regarding the demographics, radiological, histopathological and immunohistochemical features, treatment, and recurrence.2-8) These accumulated data on GOC can help to make a correct
선치성낭에 대한 임상병리학적 연구
허영성, 오규영, 윤혜정, 이재일, 홍성두*
서울대학교 치의학대학원 구강병리학교실
<Abstract>
Glandular Odontogenic Cyst: Report of 20 Cases and Review of Literature
Young-Sung Huh, Kyu-Young Oh, Hye-Jung Yoon, Jae-Il Lee, Seong-Doo Hong*
Department of Oral Pathology, School of Dentistry and Dental Research Institute, Seoul National University, Seoul, Republic of Korea
The aim of this study was to present the clinical, radiological, and histopathological findings of 20 new Korean GOC cases with a brief literature review. The mean age of 20 GOC patients was 43.5 years (range, 29-73 years) with a strong predilection for male (male-to-female ratio, 4:1). Nine cases were located in the maxilla and 11 cases in the mandible. Eight cases involved the anterior areas of the jaws and 12 cases were located in the posterior area. Most of the cases (16/20, 80.0%) showed a well-defined unilocular radiolucency and some showed cortical perforation (55.6%) and bony expansion (72.2%) in computed tomography. The most common histopathological feature was eosinophilic cuboidal cells (100%), followed by clear cells (95.0%), mucous cells (85.0%), variations in thickness (85.0%), and intraepithelial microcysts (80.0%). All cases were surgically treated by enucleation and no recurrences were found in routine follow-up.
Key words : Glandular Odontogenic Cyst, Case Series, Review
Korean Journal of Oral and Maxillofacial Pathology 2016;40(2):761-768 ISSN:1225-1577(Print); 2384-0900(Online) Available online at http://journal.kaomp.org http://dx.doi.org/10.17779/KAOMP.2016.40.2.003
* Correspondence: Seong-Doo Hong
Department of Oral Pathology, School of Dentistry, Seoul National University, 101, Daehak-ro, Jongno-gu, Seoul, Republic of Korea.
Telephone: +82-2-740-8682, E-mail: hongsd@snu.ac.kr ORCID : 0000-0001-8876-7094
diagnosis and to choose the best treatment. In an Asian population, however, a case series study of GOC has been carried out in a single institution, reporting 14 Chinese cases.7,8) Furthermore, there has been only one case report in a Korean population.9)
The aim of this study was to present the clinical, radiological, and histopathological findings of 20 new Korean GOC cases. In addition, a brief review of the English literature was performed focusing on the demographic features, cyst location, and recurrence rate.
Ⅱ. MATERIALS and METHODS
The present study included a total of 20 patients who were diagnosed with GOC and surgically treated in the Seoul National University Dental Hospital between 2006 to 2015. The demographic and clinical information was retrieved from the electronic medical record system. The radiological findings were analyzed using panoramic radiography and computed tomography (CT). Hematoxylin and eosin-stained slides were reviewed for histopathological evaluation.
The radiological analysis was done based on following eight radiological features mentioned in a previous systematic review:6) radiolucency, shape, marginal definition,
cortical status, expansion, tooth displacement, root resorption, and association with an impacted tooth. We evaluated the presence or absence of nine histological parameters which were previously suggested:4,5) eosinophilic cuboidal cells, intraepithelial microcysts, clear cells in the basal or spinous layer, mucous cells, papillary projections, cilia, epithelial spheres, variations in thickness, and multiple cystic spaces.
A review and a case series including more than 20 GOC cases were selected for our literature review. The information on demographics, cyst location, and recurrence rate as well as radiological and histopathological features of each study was reviewed and summarized.
Ⅲ. RESULTS
1. Demographics
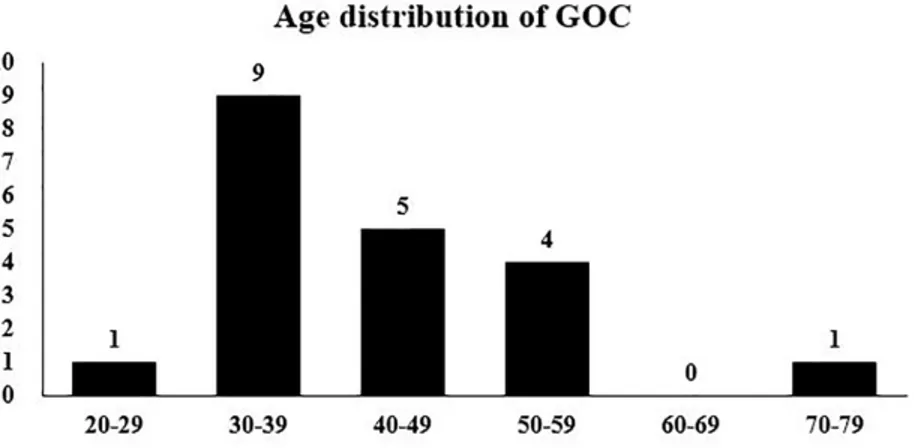
The age of the 20 GOC patients ranged from 29 to 73 years, with a mean age of 43.5 years (Fig. 1). Of the 20 GOC cases, 16 cases occurred in males and four in females, showing a strong male predilection (male-to-female ratio, 4:1).
Fig. 1. Age distribution of glandular odontogenic cyst.
2. Location
All of the 20 GOC cases occurred in the tooth-bearing area. Nine cases (45.0%) were located in the maxilla and 11 cases (55.0%) in the mandible. Eight cases (40.0%) involved the anterior areas of the jaws and 12 cases (60.0%) were located in the posterior areas (Fig. 2).
3. Radiological features
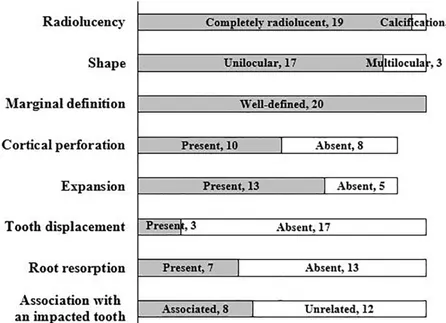
The results of our analysis of eight radiological features are presented in Fig. 3. Most of the cases (16/20, 80.0%) showed a well-defined unilocular radiolucency (Fig. 4A).
Cortical perforation and bony expansion were found in 10 (55.6%) and 13 (72.2%) cases, respectively, out of 18 cases (Fig. 4B). Of the 20 GOC cases, only one case showed heterogeneous calcification within radiolucency (Fig. 4C).
Eight cases (40.0%) were associated with an unerupted tooth, especially involving the crown of the tooth (Fig. 4D).
Fig. 2. Distribution of glandular odontogenic cyst in the jaws.
Fig. 3. Radiological features of glandular odontogenic cyst.
Fig. 4. Computed tomographic images of glandular odontogenic cyst. (A) A well-defined unilocular radiolucency with cortical thinning in the anterior mandible. (B) A well-defined unilocular radiolucency with cortical perforation and bucco-palatal expansion in the anterior maxilla. (C) A well-defined unilocular radiolucency containing heterogeneous calcification in the posterior mandible. No cortical perforation or bony expansion is observed. (D) A well-defined unilocular cyst surrounding the crown of an impacted mandibular third molar. The lesion is reminiscent of dentigerous cyst.
A B
C D
4. Histopathological features
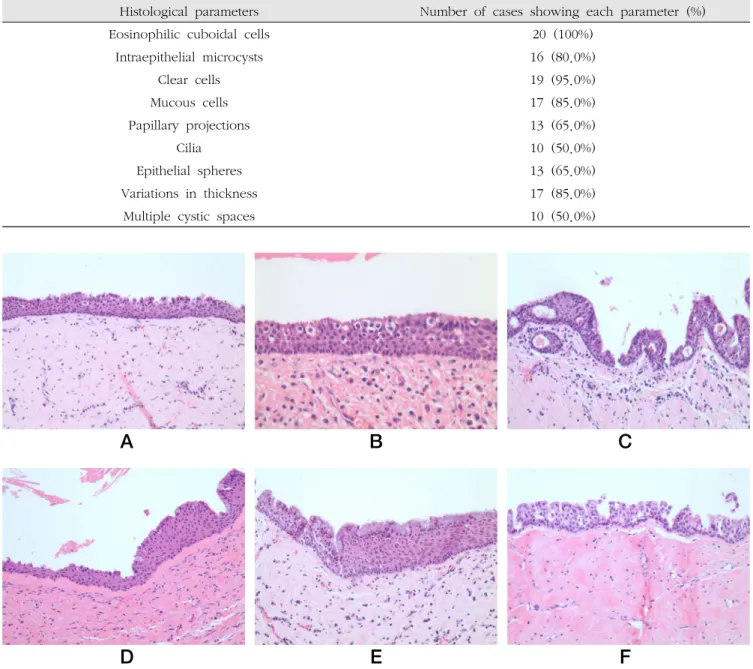
The results of our analysis of nine histological parameters are summarized in Table. 1. The most common histopathological
feature was eosinophilic cuboidal cells, so-called “hobnail cells”, on the surface of the lining (Fig. 5A). The second most common feature was clear cells in the basal or spinous layer of the lining (Fig. 5B). More than 80% of the cases
Table. 1. Histological analysis of glandular odontogenic cyst (N=20).
Histological parameters Number of cases showing each parameter (%)
Eosinophilic cuboidal cells 20 (100%)
Intraepithelial microcysts 16 (80.0%)
Clear cells 19 (95.0%)
Mucous cells 17 (85.0%)
Papillary projections 13 (65.0%)
Cilia 10 (50.0%)
Epithelial spheres 13 (65.0%)
Variations in thickness 17 (85.0%)
Multiple cystic spaces 10 (50.0%)
A B C
D E F
Fig. 5. Histopathological findings of glandular odontogenic cyst. (A) Eosinophilic cuboidal cells on the surface of the cyst lining (H&E, original magnification x200). (B) Clear cells in the lining epithelium (H&E, original magnification x400). (C) Intraepithelial microcysts or duct-like structures. (H&E, original magnification x200). (D) A variation in thickness of the lining epithelium. A few mucous cells are located in the superficial layer (H&E, original magnification x200). (E) Numerous mucous cells in the lining epithelium (H&E, original magnification x200). (F) Characteristic papillary projections of the lining epithelium (H&E, original magnification x200).
showed intraepithelial microcysts or duct-like structures, mucous cells, and variations in thickness of the lining epithelium (Fig. 5C-5E). Less commonly, papillary projections and epithelial spheres were found (Fig. 5F). Cilia and multiple cystic spaces were observed in half of the cases, respectively.
One case showed intraluminal dystrophic calcification corresponding to its radiological finding.
5. Treatment and Follow-up
All of the 20 GOC cases were surgically treated by enucleation without marginal resection. Follow-up information was obtained for 16 patients. Follow-up periods ranged from 1 month to 6 years, with a mean of 1.9 years.
All the cases showed no evidence of recurrence on follow-up radiography.
Table. 2. Clinical, radiographic and microscopic features of glandular odontogenic cyst reported in the English language literature Kaplan et al. (2008)4 MacDonald (2010)6 Fowler et al. (2011)5
Age Mean, 45.7 years
(Range of 14-75 years)
Mean, 45.00 years (Range, NR)
Mean, 51 years (Range of 20-86 years) Gender Male : Female = 1.3 : 1 Male : Female = 1.8 : 1 Male : Female = 1 : 1
Location Mn, 70%; Mx, 30%
Ant, 24%; Post, 25%;
Ant & Post, 51%
Mn, 77%; Mx, 23%
Ant, 81%; Post, 19%
Mn, 80%; Mx, 20%
Ant, 63%; Post, 37%
Radiographic features
Unilocular, 53.8%;
Well-defined, 95%;
Scalloped, 13%
Radiolucent, 98.3%;
Unilocular, 58.5%;
Well-defined, 95.7%;
Cortication, 30.4%;
Perforation, 52.2%;
Expansion, 81.8%;
Tooth displacement, 50.0%;
Root resorption, 30.0%;
Association with an unerupted tooth, 11.1%
Unilocular, 65.6%;
Perforation, 7.3%;
Tooth displacement, 4.9%;
Root resorption, 2.4%;
Association with an unerupted tooth, 19.5%
Microscopic features
<Major criteria>
Squamous epithelial lining, Variations in thickness, Cuboidal eosinophilic cells, Mucous cells,
Intraepithelial glandular structures
<Minor criteria>
Papillary proliferation, Ciliated cells,
Multicystic architecture, Clear cells
NR Eosinophilic cuboidal cells, 100%;
Microcysts, 95.7%;
Apocrine snouting, 91.3%;
Clear cells, 89.1%;
Variable thickness, 89.1%;
Tufting, 84.8%;
Mucous cells, 71.7%;
Epithelial spheres, 67.4%;
Multiple compartments, 63.0%;
Cilia, 21.7%
Recurrence 13.8-30% 17.5% 19.6-50%
Abbreviations: NR, not reported; Mn, mandible; Mx, maxilla; Ant, anterior; Post, posterior
6. A brief review of the literature on GOC
Data on clinical, radiographic and microscopic features of GOC were collected from two reviews4,6) and one case series5) and are summarized in Table. 2.
Ⅳ. DISCUSSION
Compared to the mean age (range of 45-51 years) and the gender predilection (male/female ratio, range of 1 to 1.8) previously reported in GOC patients,4-6,10) our patients were slightly younger (43.5 years) and had a stronger predilection for male (male/female ratio, 4).
It has been generally known that GOC has a strong predilection for the mandible and the anterior areas of the jaws.5,6,10) However, almost half (9/20, 45.0%) of our GOC cases occurred in the maxilla and the posterior regions (12/20, 60.0%) were involved more frequently than the anterior regions (8/20, 40.0%).
Although GOC was referred to as “sialo-odontogenic cyst”
at first in 1987,11) its name was changed to “glandular odontogenic cyst” because of the lack of evidence of salivary gland origin.1) An immunohistochemical study was performed to investigate expression of cytokeratins (CKs) in GOC specimens.8) CK14 was detected in the basal and suprabasal layer, and CK19 was expressed in all the layers.8) CK14 is the main intermediate filament of odontogenic epithelium,12) and CK19 is a useful marker for identifying odontogenic epithelial componets.13) In addition, similar to a previous report,7) all of our GOC cases occurred in the tooth-bearing area. Consequently, the odontogenic origin of GOC can be supported by the immunohistochemical result and its close proximity to the tooth.
According to previous studies, most GOCs showed a well-defined radiolucency with a single case accompanying
calcification.2,4-6) Similarly, most of our GOC cases demonstrated a well-defined radiolucent lesion and one case showed heterogeneous calcification within radiolucency.
High et al.14) have suggested that dystrophic calcification within the cyst lumen is a form of heterotopic calcification in degenerating tissue and correlates with age changes of the cyst. Of the reported GOC cases, 53.8-65.6% were unilocular,4-6) and 11.1-19.5% of the cases were associated with an unerupted tooth.5,6) Our case series showed higher rates of cases exhibiting a unilocular lesion (85.0%) and an association with an impacted tooth (40.0%).
Kaplan et al.4) have proposed five major microscopic criteria which is mandatory for diagnosis of GOC. However, three major criteria were observed in not all of our GOC cases: variations in thickness (85.0%), mucous cells (85.0%), and intraepithelial glandular structures (80.0%). Although Kaplan et al.4) have proposed clear cells as one of the minor criteria, most of our cases (95.0%) showed clear cells in the basal or spinous layer. Our results of analysis of each histological parameter were generally similar to those Fowler et al.5) have reported. The presence of eosinophilic cuboidal cells on the surface of the lining (Fowler, 100%;
our, 100%) is the most common histopathological finding, whereas multiple cystic spaces (Fowler, 63.0%; our, 50.0%) and cilia (Fowler, 21.7%; our, 50.0%) are least frequently observed in the lining epithelium of GOC.
GOC is characterized by a high recurrence rate which is comparable to that of odontogenic keratocyst.2,3,15) However, no recurrence was found in all of our cases. This can be explained by two possibilities. One is related to the fact that a majority of our cases were unilocular in shape.
Based on an association of a high frequency of multilocularity with a high recurrence rate, Kaplan et al.2,4) have suggested that locularity is a significant factor related to the tendency to recur. The other possibility is associated with short follow-up periods in our case series. Fowler et
al.5) have reported that the average time interval from initial treatment to first recurrence was 8 years, with a range of 3-13 years. Considering the mean follow-up period of 1.9 years in our case series, continuous follow-ups are required for detection of recurrence.
Ⅴ. REFERENCES
1. Gardner DG, Kessler HP, Morency R, Schaffner DL: The glandular odontogenic cyst: an apparent entity. J Oral Pathol. 1988;17:359-366.
2. Kaplan I, Gal G, Anavi Y, Manor R, Calderon S: Glandular odontogenic cyst: treatment and recurrence. J Oral Maxillofac Surg. 2005;63:435-441.
3. Momeni Roochi M, Tavakoli I, Ghazi FM, Tavakoli A: Case series and review of glandular odontogenic cyst with emphasis on treatment modalities. J Craniomaxillofac Surg.
2015;43:746-750.
4. Kaplan I, Anavi Y, Hirshberg A: Glandular odontogenic cyst:
a challenge in diagnosis and treatment. Oral Dis.
2008;14:575-581.
5. Fowler CB, Brannon RB, Kessler HP, Castle JT, Kahn MA:
Glandular odontogenic cyst: analysis of 46 cases with special emphasis on microscopic criteria for diagnosis. Head Neck Pathol. 2011;5:364-475.
6. Macdonald-Jankowski DS: Glandular odontogenic cyst:
systematic review. Dentomaxillofac Radiol. 2010;39:127-139.
7. Qin XN, Li JR, Chen XM, Long X: The glandular odontogenic
cyst: clinicopathologic features and treatment of 14 cases.
J Oral Maxillofac Surg. 2005;63:694-699.
8. Shen J, Fan M, Chen X, Wang S, Wang L, Li Y: Glandular odontogenic cyst in China: report of 12 cases and immunohistochemical study. J Oral Pathol. Med 2006;35:
175-182.
9. Lee BD, Lee W, Kwon KH, Choi MK, Choi EJ, Yoon JH:
Glandular odontogenic cyst mimicking ameloblastoma in a 78-year-old female: A case report. Imaging Sci Dent.
2014;44:249-252.
10. Neville BW, Damm DD, Allen CM, Bouquot JE: Oral and Maxillofacial Pathology, 3rd ed. St. Louis, MO: Saunders, 2008:697-698.
11. Padayachee A, Van Wyk CW: Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: sialo-odontogenic cyst? J Oral Pathol. 1987;16:499-504.
12. Crivelini MM, de Araujo VC, de Sousa SO, de Araujo NS:
Cytokeratins in epithelia of odontogenic neoplasms. Oral Dis. 2003;9:1-6.
13. Kumamoto H, Yoshida M, Ooya K: Immunohistochemical detection of amelogenin and cytokeratin 19 in epithelial odontogenic tumors. Oral Dis. 2001;7:171-176.
14. High AS, Hirschmann PN: Age changes in residual radicular cysts. J Oral Pathol. 1986;15:524-528.
15. Antonoglou GN, Sandor GK, Koidou VP, Papageorgiou SN:
Non-syndromic and syndromic keratocystic odontogenic tumors: systematic review and meta-analysis of recurrences.
J Craniomaxillofac Surg. 2014;42:e364-371.