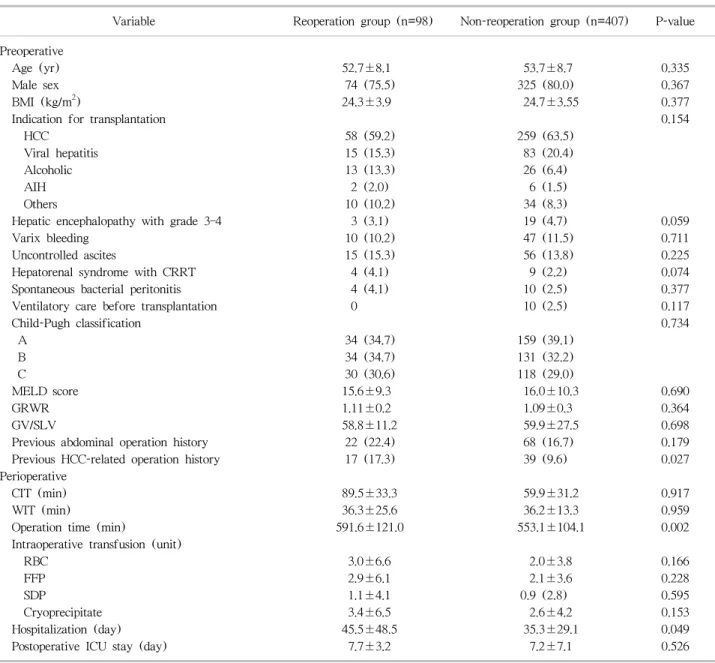
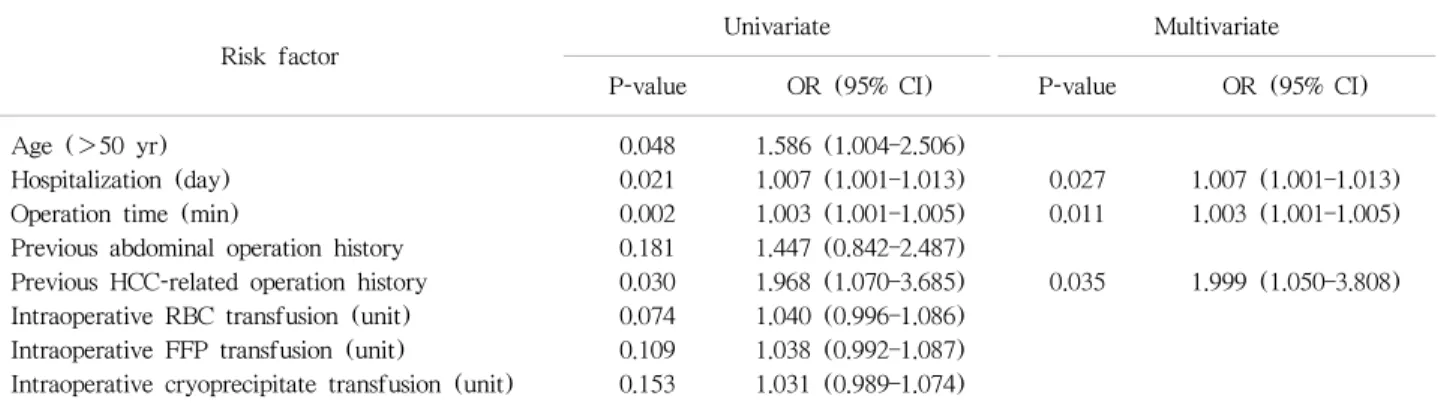
Early reoperation after adult living-donor liver transplantation is associated with poor survival
전체 글
수치
관련 문서
Early efficacy signals in the mid dose cohort suggest positive biological activity and potential early clinical benefits. High dose adult cohort is currently ongoing with no
Based on the results of root cause analysis, the following corrective action to mitigate the erosion and corrosion damage at hot leg check valve were
Also, peak to end time of T-wave, T-wave width/depth in patients with apical hypertrophic cardiomyopathy is more longer and greater than in those with stress-induced cardiomyopathy
In 4-week group, the group filled with bone graft with decortication revealed larger new bone formation area than shown in the group that had a defect area
This study focuses on the overall survival(OS) and the re-recurrence free survival (RFS) rates for patients according to the Milan criteria status at the time of recurrence as
This study has the following academic suggestions: First, this study focused on the effects of workplace innovation on living quality of rural people with
Although van der Waals equation is still less accurate at high
The associations of hepatic steatosis and fibrosis using fatty liver index and BARD score with cardiovascular outcomes and mortality in patients with new‑onset type 2