Background: The aim of this study was to review clinical efficacy of acupuncture treatment of mild cognitive impairment.
Methods: Randomized controlled trials that performed acupuncture treatment for mild cognitive impairment were retrieved from 6 online databases (PubMed, Cochrane Library, EMBASE, CNKI, NDSL, OASIS) on September 30th, 2018. Studies were selected according to inclusion and exclusion criteria, and were reviewed by Risk of Bias assessment.
Results: In total, 21 studies were included in this review. All studies were Chinese (19 studies published in Chinese and 2 in English). The sample size, 50 to 100, and the number of treatment times, 20 to 30, were the largest range in all studies. The most treatments performed was 30. The longest treatment period was 56 days, which accounted for 33% of the studies. The most frequently used evaluation index was the Mini Mental State Examination followed by the Montreal Cognitive Assessment, each used 17 times and 15 times, respectively.
The most frequently used acupoints were GV20, EX-HN1, GB20, and GV24, which accounted for 47%
of total number of acupoints used. In 48% of the studies, needle retention time was 30 minutes. Western medicine treatment was the most common control group. Most studies reported that the intervention group was statistically significantly different to the control group.
Conclusion: These results suggest that acupuncture for mild cognitive impairment was effective. However, it is difficult to confirm this conclusion because the quality of most of these studies were of low quality.
©2019 Korean Acupuncture & Moxibustion Medicine Society. This is an open access article under the CC BY- NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Article history:
Submitted: April 27, 2019 Accepted: May 3, 2019 Keywords:
acupuncture,
mild cognitive impairment, systematic review
https://doi.org/10.13045/jar.2019.00108 pISSN 2586-288X eISSN 2586-2898
Review Article
Systematic Review of Acupuncture Treatment for Mild Cognitive Impairment
Min Wook Kim 1, Jae Hee Yoo 1, Hong Je Go 1, Seon Woo Kim 2, Seung Won Jang 3, Hyun Jin Jeong 4, Jae Hong Kim 1, *
1 Department of Acupuncture and Moxibustion Medicine, DongShin University, Naju, Korea
2 Department of Acupuncture and Moxibustion Medicine, Gwang-ju Jaseng Hospital of Oriental Medicine, Gwangju, Korea 3 Department of Acupuncture and Moxibustion Medicine, DongShin Korean Medicine Hospital, Seoul, Korea
4 Department of Oriental Internal Medicine, DongShin University Oriental Hospital, Gwangju, Korea
ABSTRACT
Journal of Acupuncture Research
Journal homepage: http://www.e-jar.org
Introduction
As the elderly population increases, the prevalence of dementia also increases, provoking interest in the prevention of dementia and mild cognitive impairment (MCI) [1]. Mild cognitive impairment is a condition that occurs as a result of normal aging, an intermittent stage that may lead to mild dementia [2], identified by Petersen, a psychiatrist in the United States in 1966.
A clinical study has shown that 44% of patients diagnosed with MCI developed dementia within 3 years [3]. Thus, the need for treatment of MCI is important to reduce the potential progression to dementia.
Currently there is no approved drug to treat MCI in Western
medicine. Alzheimer's drugs such as donepezil, rivastigmine, and cholinesterase inhibitors, have been evaluated as potential treatments for MCI in a number of clinical trials [4-6].
Alternatively, there are studies that suggest non-drug treatment, such as cognitive training or physical exercise therapy may be helpful [7,8], but further research is needed.
There is also no defined treatment for MCI in traditional oriental medicine [9,10], which have reportedly less side effects than Western drug treatment. Several randomized controlled trials (RCT) [11-31] have been reported where acupuncture treatment of MCI has been evaluated including systematic review [32-34].
However, in the study by Hu et al [32], EMBASE and Cochrane databases were absent. Studies by Mai and Zheng [33] and Wang
*Corresponding author.
Department of Acupuncture and Moxibustion Medicine, DongShin University Gwangju Korean Medicine Hospital, 141 Wolsan-ro, Nam-gu, Gwangju, 61619, Republic of Korea
[34] also excluded EMBASE, and there were some inconsistencies in the analysis. Among these systematic reviews, there were no studies including Korean databases.
The purpose of this study was to investigate the effectiveness of acupuncture treatment in MCI by using 6 online databases including the Korean database and EMBASE (PubMed, Cochrane Library, EMBASE, CNKI, NDSL, OASIS).
Materials and Methods Data sources
To investigate the efficacy of acupuncture treatment of MCI, database searches were performed to retrieve studies published until September 30, 2018. The databases included were PubMed/
MEDLINE, Cochrane, EMBASE, the China National Knowledge Infrastructure (CNKI) for international publications, the National Digital Science Library (NDSL), and the Oriental Medicine Advanced Searching Integrated System (OASIS) for Korean publications.
Keywords were used for the database searches with minor adjustments for each database: (“mild cognitive impairment”
or “cognitive dysfunction”), (“acupuncture” or “acupuncture therapy” or “chiropractic” or “acupuncture points” or “acupuncture analgesia” or “electroacupuncture” or “scalp acupuncture”)
Eligibility criteria Inclusion criteria
RCTs were included that reported on acupuncture treatment of patients with mild cognitive impairment, with no differentiation placed on the method of acupuncture treatment. In addition, there were no restrictions in the control group and on the year of publication.
Exclusion criteria
Studies that were not RCT’s, case studies, systematic reviews, literature reviews, articles, and protocols were all excluded.
Furthermore, vascular MCI, and MCI due to stroke or brain damage were excluded. Studies with only abstracts available or studies whose original text was unavailable, were also excluded.
Data collection and risk of bias
Studies that satisfied the inclusion criteria were selected and 2 reviewers performed data extraction and assessment independently. In cases of disagreement, the matter was reassessed by a 3rd reviewer. The risk of bias in RCT’s was assessed using the Cochrane risk of bias tool [35].
Results
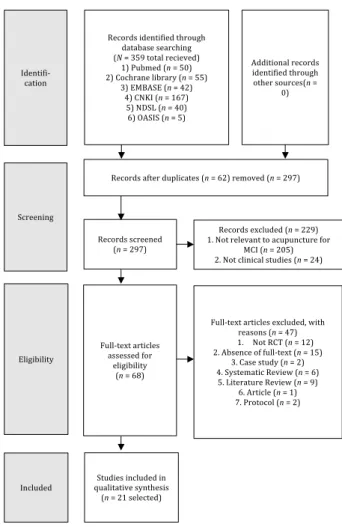
A total of 359 studies were retrieved from 6 online databases until September 30, 2018. Of the 359 articles retrieved, PubMed had 50, Cochrane 55, EMBASE 42, CNKI 167, NDSL 40 and OASIS 5. From the 359 studies, 62 duplicates were removed, along with 205 non-related studies, and 24 non-clinical studies. Of the 68 studies remaining, 15 studies were excluded as they did not have the original text, and 53 studies were excluded because 12 were not RCT, 2 were case studies, 6 were systematic reviews, 9 were literature reviews, 1 was an article, and 2 were protocols. This provided a final study sample of 21 (Table 1; Fig. 1). All 21 studies were published in China, of which 19 were in Chinese and 2 were in English.
Year of publication
Analysis by year showed that 21 studies used acupuncture to treat MCI from 2009 to 2017 (Fig. 2).
Fig. 2. Analysis of the number of articles published.
12
Fig. 2. Analysis of the number of articles published.
0 1 2 3 4 5 6
2009 2010 2011 2012 2013 2015 2016 2017
Publication year
12
Fig. 2. Analysis of the number of articles published.
0 1 2 3 4 5 6
2009 2010 2011 2012 2013 2015 2016 2017
Publication year
Fig. 1. Flow diagram according to the diagram of PRISMA.
MCI, mild cognitive impairment; RCT, randomized controlled trial.
8
Identifi-‐
cation
Records identified through database searching (N = 359 total recieved)
1) Pubmed (n = 50) 2) Cochrane library (n = 55)
3) EMBASE (n = 42) 4) CNKI (n = 167) 5) NDSL (n = 40) 6) OASIS (n = 5)
Additional records identified through other sources(n =
0)
Screening
Records after duplicates (n = 62) removed (n = 297)
Records screened (n = 297)
Records excluded (n = 229) 1. Not relevant to acupuncture for
MCI (n = 205) 2. Not clinical studies (n = 24)
Eligibility
Full-‐text articles assessed for
eligibility (n = 68)
Full-‐text articles excluded, with reasons (n = 47) 1. Not RCT (n = 12) 2. Absence of full-‐text (n = 15)
3. Case study (n = 2) 4. Systematic Review (n = 6) 5. Literature Review (n = 9)
6. Article (n = 1) 7. Protocol (n = 2)
Included Studies included in qualitative synthesis (n = 21 selected)
No. author (y) N Intervention Control Treatment Evaluation
index Result
(A > B, C, D) Adverse
events Acupoints
No. Period
01.Liu (2009)
[11] 26 A: Atx
(n = 9) B: W-med (n = 8) 30 30 d
1.ADL 2.CDR 3.MMSE
4.CMS
1. p < 0.05 2. p < 0.05 3. p < 0.05 4. p < 0.05
NR Ex-HN1, HT7, GB20, BL23, KI3, GB39 02.Sun (2009)
[12] 60 A: E-Atx + B
(n = 30) B: W-med (n = 30) 30 30 d 1.MMSE 1. p < 0.01 NR GV20, PC6, SP6
03.Wang (2009)
[13] 60 A: Atx
(n = 30) B: W-med (n = 30) 28 28 d
1.MMSE 2.ADL 3.TCM syndrome table
1. p < 0.05 2. p < 0.05
3. p < 0.05 NR GV20, Ex-HN1, GV24, GB20, BL23, KI3 04.Zhang(2009)
[14] 60 A: Atx + B
(n = 30) B: W-med (n = 30) 30 30 d 1.MMSE
2.MoCA 1. p < 0.05
2. p < 0.05 NR GV20, GV24, ST8, PC6, SP6 05.Jin (2010)
[15] 30 A: E-Atx (n = 14) B: W-med (n = 16) 45 45 d 1.CMS
2.MoCA 3.MRS
1. p < 0.01 2. p < 0.01
3. p < 0.05 NR Ex-HN1, BL23, GB20, KI3 06.Liu (2010) [16] 45 A: E-Atx (n = 17) B: W-med (n = 19) 30 30 d 1.MMSE
2.MoCA 3.MRS
1. p < 0.05 2. p < 0.05
3. p < 0.05 NR GV20, GB20, BL23, KI3, GB39 07.Wang (2010)
[17] 60 A: E-Atx + B
(n = 35) B: Cognitive
training (n = 35) 48 56 d 1.MoCA 1. p < 0.05 NR Yu's scalp clustering
acupuncture 08.Wang (2011)
[18] 60 A: E-Atx + B
(n = 35) B: Cognitive
training (n = 35) 48 56 d 1.MoCA 1. p < 0.05 NR Yu's scalp clustering
acupuncture 09.Yu (2010) [19] 112 A: E-Atx
(n = 56) B: W-med (n = 56) 24 56 d 1.MMSE
2.WMS 3.CDT
1. p < 0.01 2. p < 0.01
3. p < 0.05 NR Ex-HN1, GV20, GV24, GB20 10.Chen (2011)
[20] 252
A1: E-Atx (n = 84) A2: E-Atx + CMD (n = 84)
B: W-med (n = 84) 24 56 d 1.MMSE
2.WMS 3.CDT
1. p < 0.05 2. p < 0.05
3. p < 0.05 NR GV20, Ex-HN1, GB20, GV24 11.Li (2011) [21] 60 A: B + C
(n = 20) B: Atx (n = 20)
C: W-med (n = 20) 24 28 d 1.MMSE
2.MoCA 3.ERP
1. p < 0.05 2. p < 0.05
3. p < 0.05 NR GV20, GV24, GB13, BL18, BL23, PC6, LI4,
KI6, LR3 12.Li (2012) [22] 60 A: Atx + C-med
(n = 30) B: W-med (n = 30) 28 28 d 1.MMSE
2.MoCA 3.ADL
1. p < 0.05 2. p < 0.05
3. p < 0.05 NR
GV20, Ex-HN1, GV24, GB20, KI3, ST36, BL23, ST40, GB39, SP6, PC6,
BL17 13.Zhang(2012)
[23] 120 A: Atx + B
(n = 65) B: W-med (n = 55) 10 3 mo 1.MoCA 1. p < 0.01 NR GV20, Ex-HN1
14.Zhao (2012)
[24] 60 A: Atx + B
(n = 30) B: W-med (n = 30) 32 56 d 1.MMSE
2.MoCA 3.ERP
1. p < 0.05 2. p < 0.05
3. p < 0.05 NR Ex-HN1, GB20, GV20, GB13 15.Zhang(2013)
[25] 252
A1: E-Atx (n = 80) A2: E-Atx + CMD (n = 78)
B: W-med (n = 75) 24 56 d 1.MMSE
2.WMS 3.CDT
1. p < 0.01 2. p < 0.01
3. p < 0.01 NR GV20, Ex-HN1, GB20, GV24
16.Du (2016) [26] 40 A: Atx
(n = 20) B: W-med (n = 20) 48 56 d 1.BDNF
2.MMSE 3.MoCA
1. p < 0.05 2. p < 0.05
3. p < 0.05 NR GV20, GV14i, GV23, GV16, GV15, Ex-HN1,
KI3, LR3, ST36, GB39 17.Wang (2015)
[27] 120 A: B + C
(n = 30)
B: Atx C: C-med D: W-med
(n = 30, 30, 30) 45 3 mo 1.MMSE 1. p < 0.01 NR GV20, GV24, GB41, EX-
HN5, GB20 18.Li (2016) [28] 60 A: Atx + C-med
(n = 30) B: W-med (n = 30) 45 3 mo 1.MMSE
2.MoCA 1. p < 0.01
2. p < 0.01 NR GV20, GV24, GB15, GB17, GV20, EX-HN5,
GB20 19.Chen (2017)
[29] 60 A: Atx + B
(n = 30) B: W-med (n = 30) 24 28 wk 1.MMSE
2.MoCA 3.ADL
1. p < 0.05 2. p < 0.05
3. p < 0.05 NR Five-element
acupuncture style 20.Liu (2017) [30] 60 A: Atx + B
(n = 30) B: W-med (n = 30) 30 30 d 1.MMSE
2.MoCA 3.Barthel
1. p < 0.05 2. p < 0.05
3. p > 0.05 NR Yu's scalp clustering acupuncture
21.Tan (2017) [31] 32 A: Atx
(n = 16) B: Sham Atx
(n = 16) 20 28 d 1.MMSE
2.MoCA 3.*Etc
1. p < 0.05 2. p < 0.05
3. p < 0.05 NR Ex-HN1, DU29, PC6, KI3, ST40, LR3 Table 1. Details of the Final Study Samples Included for Analysis.
Sample size of study
The total number of patients in the experimental group and control groups was analyzed. Of the 21 studies, 5 studies (24%) had less than 50 patients, 11 studies (52%) had 50 to 100 patients, 3 studies (14%) had 100 to 200 patients, and 2 studies (10%) had more than 200 patients (Fig. 3).
Treatment number of times and period
The number of acupuncture treatments ranged from 10 to 48, with 24 and 30 treatments being the most common. When expressed as a range, there was 1 study (5%) with 10 to 20 treatments, 8 studies (38%) with 20 to 30 treatments, 6 studies (28%) with 30 to 40 treatments, and 6 studies (29%) with 40 to 50 treatments (Fig. 4).
The most frequent treatment period was 56 days which was observed in 7 studies (33%), This was followed by 28 days and 30 days which were used in 5 studies each (24%), 45 days in 1 study (5%), and 3 months in 3 studies (14%; Fig. 5).
Evaluation index
In a single study at least 1 evaluation indicator was used and at the most 7 were used. A total of 1,610 patients were evaluated for 16 evaluation indices, in a total of 21 studies. There were 17 studies that used the mini mental state examination (MMSE) as the evaluation index. There were 15 studies that used the Montreal cognitive assessment (MoCA), 4 studies that used the activities of daily living (ADL), 3 studies that used Wechsler memory scale (WMS), clock drawing test (CDT), magnetic resonance imaging (MRI), 2 studies that used event-related potentials (ERP), clinical memory scale (CMS), respectively, and 8 other evaluation indices were used once for each scoring scale (Fig. 6).
Analysis of acupuncture treatment
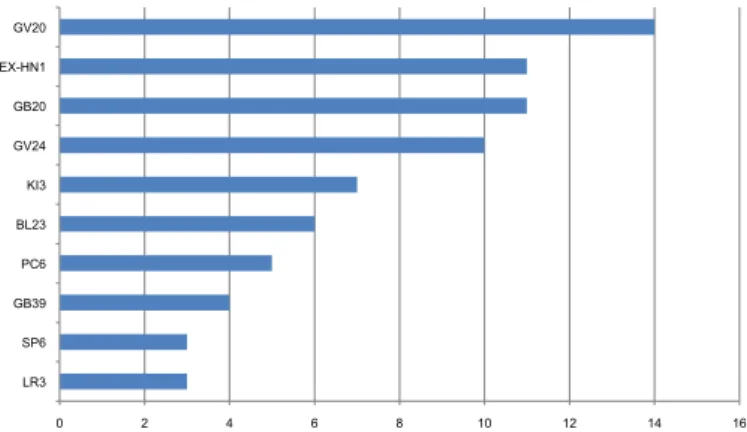
There were 17 studies that used acupoints and the most frequently used acupoint was Baihui (GV20), which was used in 14 studies. Sishencong (EX-HN 1) and Fengchi (GB20) were used in 11 studies, Shenting (GV24) in 10, Taixi (KI3) in 7, Shenyu (BL23)
Fig. 3. A depiction of the sample sizes recruited in the RCT’s. RCT, randomized controlled trial.
14
Fig. 3. A depiction of the sample sizes recruited in the RCT’s. RCT, randomized controlled trial.
24%
52%
14%
10%
n ≤ 50 50 < n ≤ 100 100 < n ≤ 200 n > 200
14
Fig. 3. A depiction of the sample sizes recruited in the RCT’s. RCT, randomized controlled trial.
24%
52%
14%
10%
n ≤ 50 50 < n ≤ 100 100 < n ≤ 200 n > 200
Fig. 5. Analysis of the duration of the treatment period.
18
Fig. 5. Analysis of the duration of the treatment period.
24%
24%
5%
33%
14%
28 days 30 days 45 days 56 days 3 months
18
Fig. 5. Analysis of the duration of the treatment period.
24%
24%
5%
33%
14%
28 days 30 days 45 days 56 days 3 months
Fig. 6. Analysis of the frequency and type of evaluation index performed.
ADL, activities of daily living; CDT, clock drawing test; CMS, clinical memory scale;
ERP, event-related potentials; MMSE, mini mental state examination; MoCA, Montreal cognitive assessment; MRI, magnetic resonance imaging; WMS, Wechsler memory scale.
20
Fig. 6. Analysis of the frequency and type of evaluation index performed.
ADL, activities of daily living; CDT, clock drawing test; CMS, clinical memory scale; ERP, event- related potentials; MMSE, mini mental state examination; MoCA, Montreal cognitive assessment;
MRI, magnetic resonance imaging; WMS, Wechsler memory scale.
0 2 4 6 8 10 12 14 16 18
Etc CMS ERP MRI CDT WMS ADL MoCA MMSE n ≤ 50
50 < n ≤ 100 100 < n ≤ 200 n > 200
Fig. 4. Analysis of the number of treatment used in the RCT’s. RCT, randomized controlled trial.
16
Fig. 4. Analysis of the number of treatment used in the RCT’s. RCT, randomized controlled trial.
5%
38%
28%
29%
10 ≤ n < 20 20 ≤ n < 30 30 ≤ n < 40 n ≥ 40
16
Fig. 4. Analysis of the number of treatment used in the RCT’s. RCT, randomized controlled trial.
5%
38%
28%
29%
10 ≤ n < 20 20 ≤ n < 30 30 ≤ n < 40 n ≥ 40
10 ≤ n < 20 20 ≤ n < 30 30 ≤ n < 40 n ≥ 40
in 6, Neiguan (PC6) in 5, Xuanzhong (GB39) in 4, and Sanyinjiao (SP6) and Taichong (LR3) were used in 3 studies. The acupoints were used 1 or 2 times, and over the course of treatment the acupoints were used 23 times in total (Fig. 7).
In the 17 studies that used acupoints, the needle retention times were 30 minutes in 10 studies, 20 minutes in 3 studies, 40 minutes
in 3 studies and 6 hours in 1 study (Fig. 8).
There were 9 monotherapy groups in the treatment group, and 12 in the combination therapy group. In the monotherapy group, 6 studies used electroacupuncture, and 3 studies acupuncture alone. In the combination therapy group, 7 studies combined treatment with Western medicine, 3 with Chinese medicine, and 2 with cognitive training. Among the combination therapy group, 2 studies used electroacupuncture and 10 studies used acupuncture alone.
Treatment of control group
The most common control group was Western medicine which was used in 17 studies. There were 2 studies that used cognitive training as a control, 1 that used sham acupuncture as a control, and 1 that used acupuncture, Chinese medicine, western medicine respectively (Fig. 9).
Therapeutic effect
Efficacy of acupuncture treatment was measured in the 21 selected studies, the experimental and control groups (n = 47) were analyzed and evaluation indices in the acupuncture treated groups showed improvement after treatment in 13 studies, (3 studies showed that only the experimental group improved after treatment). The comparison between the experimental group and the control group was made to assess the therapeutic effects. In 16 studies, the experimental group showed a statistically significant improvement for each evaluation index compared to the control group. In the remaining 5 studies, Wang et al [13] showed that treatment with traditional Chinese medicine (TCM) when using the syndrome table, had a statistically significant beneficial effect in the experimental group compared to the control group, but there was no significant difference between the 2 groups when using the MMSE and the ADL evaluation indices. In the study by Liu et al [16], only the experimental group showed improvement after treatment when using the MMSE and MoCA evaluation indices, and there was a significant difference compared to the control group after treatment. However, in the NAA/Cr (left hippocampus), there was no significant difference between the 2 groups after treatment. In the NAA/Cr and the CHO/Cr (left temporal lobe), only the experimental group showed improvement after treatment. There was a significant difference between the 2 groups after treatment. In the study by Yu et al [19], the MMSE and the WMS evaluation indices showed improvement after treatment in both experimental and control groups. There was a significant difference between the 2 groups after treatment, but only the control group showed improvement in the CDT evaluation index after treatment. There was no significant difference between the 2 groups. In the study by Zhang et al [25], the MMSE and the CDT evaluation indices showed improvement after treatment in both experimental and control groups. There was a significant difference in the experimental group compared to the control group, but only in the experimental group was there improvement after treatment in the WMS evaluation index. There was a significant difference between the groups. In the study by Liu et al [30], the MMSE and the MoCA evaluation indices showed improvement after treatment in both experimental and control groups, and there was a significant difference in the experimental group compared to the control group, but in the Barthel evaluation index, there was no significant beneficial effect after treatment in both experimental and control groups.
Fig. 7. Analysis of the frequency of acupoints used to treat MCI. MCI, mild cognitive impairment.
22
Fig. 7. Analysis of the frequency of acupoints used to treat MCI. MCI, mild cognitive impairment.
0 2 4 6 8 10 12 14 16
LR3 SP6 GB39 PC6 BL23 KI3 GV24 GB20 EX-HN1 GV20
Fig. 8. Analysis of needle retention time across the RCT’s. RCT, randomized controlled trial.
24
Fig. 8. Analysis of needle retention time across the RCT’s. RCT, randomiz
ed controlled trial.
0 2 4 6 8 10 12
unclear 6 h 40 min 30 min 20 min
Fig. 9. Analysis of the conditions used for the control group in each RCT.
Etc., acupuncture, Chinese medicine, western medicine group.
RCT, randomized controlled trial.
Fig. 9. Analysis of the conditions used for the control group in each RCT.
Etc., acupuncture, Chinese medicine, western medicine group.
RCT, randomized controlled trial.
0 2 4 6 8 10 12 14 16 18
Etc Sham acupuncture Cognitive training Western medicine
Adverse reaction
None of the 21 studies reported any adverse reactions.
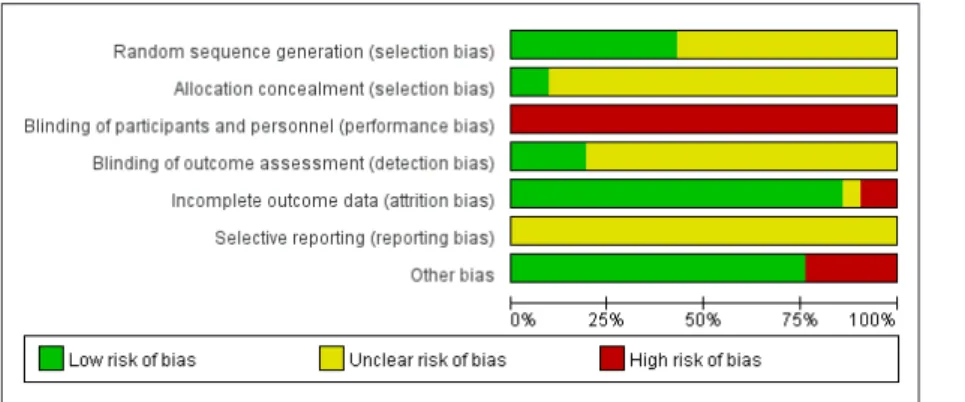
Risk of bias assessment
The risk of bias was assessed for 21 studies using Cochrane risk of bias tool (Figs. 10, 11).
Random sequence generation
Low risk was observed in 9 studies (43%) where 6 studies used a random number table, and 3 studies used computers for random sequence generation. In the remaining 12 studies (57%), the level of risk was unclear because of the random division of the group without description of the randomization method.
Allocation concealment
Low risk was observed in 2 studies (10%) which used sealed envelopes with serial numbers. The remaining 19 studies (90%) were classified as having an unclear risk because there was no mention of concealment or lack of judgment.
Blinding of participant and personnel
All 21 studies (100%) were categorized as high risk because the studies were not blinded, due to the characteristics of acupuncture treatment.
Blinding of outcome assessment
Four studies (19%) were classified as low risk because of the presence of a separate evaluator and blinding of the study. In the other 17studies (81%), all of them were classified as unclear risk because there was no mention of blinding of outcome assessment.
Incomplete outcome data
Low risk was observed in 18 studies (86%) where there were 4 studies with incomplete outcome data, but these 4 studies did not affect the outcome significantly, and there were 14 studies that had complete data. High risk was observed in 2 studies (10%), and it was judged that the incomplete data outcome could affect the results because there was no mention that it did not significantly affect the outcome. Unclear risk was observed in 1 study (5%), which stated that they did not know if there was an incomplete outcome.
Fig. 10. Risk of RCT bias. RCT, randomized controlled trial.
30
Fig. 10. Risk of RCT bias. RCT, randomized controlled trial.
Fig. 11. Risk of RCT bias summary.
(+) : Low risk of bias, (-) : High risk of bias, (?) : Unclear of bias.
RCT, randomized controlled trial.
31
Selective reporting
All 21 studies (100%) were categorized as unclear risk because there was no report of protocols and predefined plans.
Other bias
High risk was observed in 5 studies (24%). Among them, 1 study found that the number of patients initially recruited, and the number of patients assigned to the experimental group and the control group did not match, and there was no mention of the cause. There were 4 studies, which did not report the needle retention time, and were classified as high risk because it was considered that there was potential bias. In the remaining 16 studies (76%), the possibility of additional bias was not found and were classified as low risk.
Discussion
To evaluate the efficacy of acupuncture treatment for MCI, 6 online databases were searched and 21 RCT’s were selected for systematic review. All 21 studies were published in China, of which 19 were in Chinese and 2 in English. The largest sample size range was 50 to 100, all of which was 60 patients, accounting for 52% of all RCT studies. The largest number of treatment times range was 20 to 30, accounting for 38% of all studies. The highest number of treatments was 24 and 30. The longest treatment period was 56 days, which accounted 33% of the RCT’s. The results of these RCT’s suggests that acupuncture treatment performed 3 or 4 times per week may have a beneficial therapeutic effect against MCI.
A total of 1,610 patients were evaluated using 16 indices across 21 studies. The most frequently used evaluation was the MMSE, followed by the MoCA where each was used 17 and 15 times, respectively. This implies that the MMSE and the MoCA were the most common measures to evaluate the acupuncture treatment of MCI.In the 17 studies that used acupoint the most commonly used acupoint was Baihui (GV20), which was used 14 times. Sishencong (EX-HN 1) and Fengchi (GB20) were used 11 times. Shenting (GV24) was used 10 times. These 4 acupoints accounted for 46 out of 97 times (47%) acupoints, implying that these 4 acupoints were commonly used and were thought to have a more beneficial therapeutic effect than other acupoints. In these 17 studies, 10 selected the needle retention times as 30 minutes which was the longest time period over the total 17 RCT’s. Therefore, it was the most common retention time and may be the most effective time for acupuncture treatment. There were 9 monotherapy treatment groups, and 12 combination therapy groups. In the monotherapy group, 6 studies used electroacupuncture, 3 studies used only acupuncture. In the combination therapy group, 7 studies combined treatment with Western medicine, 3 with Chinese medicine, and 2 with cognitive training. Among the combination therapy groups, 2 studies used electroacupuncture, 10 studies used only acupuncture.
In the control group setting, it was observed that 17 of the studies used Western medicine to determine the efficacy of acupuncture treatment of MCI. In the 21 studies, the experimental group and the control group were compared. In each evaluation index of 16 studies, the experimental group showed a statistically significant difference compared with the control group, indicating that acupuncture treatment was a beneficial treatment for MCI. In the remaining 5 studies, the difference between the control group and the treatment group was not statistically significant for each
for MCI.
Bias is a systematic error where the findings have deviated from the true value of the outcome or estimation. Understanding bias may reveal an underestimation or overestimation of the intervention effect. In this study, the risk of bias was evaluated in 7 areas using Cochrane’s risk of bias (RoB) tool [35] (random sequence generation, allocation concealment, blinding of participant and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias).
The overall risk assessment of bias was unclear for most of the 21 studies. Only 9 out of 21 studies described random sequence generation, and only 2 studies described allocation concealment.
Blinding of either patient and staff was difficult due to the nature of acupuncture treatment. Selective reporting areas were not mentioned in all studies. Analysis of bias risk showed that in most studies, explanations of research methods were overly concise, or not even described in the random sequence generation, allocation concealment or selective reporting area and so bias could not be avoided. These results suggested that researchers require greater awareness of bias when conducting RCT’s. Thus, in order to demonstrate the efficacy of acupuncture treatment for MCI, improved design of clinical studies with low bias will be required by referring to RCT guidelines such as CONSORT 2010 [36].
However, there is a limit to effectively designing a blinded trial due to the interventional nature of acupuncture treatment, therefore future research will be needed to improve study designs and controls for acupuncture research studies.
In conclusion, these results suggest that acupuncture treatment for MCI was effective and statistically significantly different to the control group, such as Western medicine or cognitive training.
However, the quality of most of the studies was low.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Acknowledgments
This research was supported by the DongShin University research grants.
References
[1] Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 1999;56:303-308.
[2] Xiao L, Shang HC, Wang JY, Hu J, Xiong J. Assessing the Quality of Reports about Randomized Controlled Trials of Acupuncture Treatment on Mild Cognitive Impairment. PLoS ONE 2011;6:1-6.
[3] Gmdman M, Petemen RC, Morris JC. Rate of dementia of the Alzheimer type in patients with mild cognitive impairment. Neurology 1996;46:A403.
[4] Doody RS, Ferris SH, Salloway S, Sun Y, Goldman R, Watkins WE et al.
Donepezil treatment of patients with MCI: a 48-week randomized, placebo- controlled trial. Neurology 2009;72:1555–1561.
[5] Petersen RC, Thomas RG, Grundman M, Bennett D, Doody R, Ferris S et al.
Vitamin E and donepezil for the treatment of mild cognitive impairment. N Engl J Med 2005;352:2379–2388.
[6] Salloway S, Ferris S, Kluger A, Goldman R, Griesing T, Kumar D et al.
Efficacy of donepezil in mild cognitive impairment: a randomized placebo- controlled trial. Neurology 2004;63:651–657.
[7] Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution. J Intern Med 2014;275:214- 228.
(LR2) on Scopolamine-induced Cognitive Impairment in Rat Model. J Acupunct Res 2018;35:28-36. [in Korean].
[10] Hyun MK, Mo MJ, Hwang DR, Yang TJ, Lee JH, Lee EJ et al. The Effects of Jodeungsan Pharmacopuncture at GB20 on Cognitive Impairment Induced by Focal Brain Injury in Rats. J Acupunct Res 2016;33:49-63. [in Korean].
[11] Liu J, Liu ZY. Clinical Observations on Electroacupuncture Treatment for Mild Cognitive Impairment of Kidney Essence Deficiency Type. Shanghai J Acupunct Moxibustion 2009;28:319-321. [in Chinese].
[12] Sun YZ, Zhang Y. Clinical Observations on the Treatment of Mild Cognitive Impairment in Elder People by Combined Acupuncture and Duxil. J Clin Acupunct Moxibustion 2009;25:16-17. [in Chinese].
[13] Wang QD [Dissertation]. Clinical study of jiannao bushen acupuncture for MCI. Harbin (China) : Heilongjiang University of Chinese Medicine; 2009.
[in Chinese].
[14] Zhang Y [Dissertation]. Observing the efficacy of the combination of acupuncture and duxil in treating mild cognitive impairment. Harbin (China): Heilongjiang University of Chinese Medicine; 2009. [in Chinese].
[15] Jin XZ [Dissertation]. Electro-acupuncture intervention in essence deficiency Mild Cognitive Impairment study of Clinical. Urumqi (China):
Xinjiang medical university; 2010. [in Chinese].
[16] Liu XP [Dissertation]. Electro-acupuncture intervention in essence deficiency Mild Cognitive Impairment Study of H-MRS. Urumqi (China):
Xinjiang medical university; 2010. [in Chinese].
[17] Wang Y, Cao H, Xing Y. Observation of Effect of Cluster Needling of Electro-‘qi’acupuncture Combination of Cognitive Training in Acupuncture treatment of Mild Cognitive Impairment. J Clin Acupunct Moxibustion 2010;26:32-34. [in Chinese].
[18] Wang Y [Dissertation]. Observation of Effect of Cluster Needling of Electro-‘qi’acupuncture Combination of Cognitive Training in Acupuncture treatment of Mild Cognitive Impairment. Harbin (China): Heilongjiang University of Chinese Medicine; 2010. [in Chinese].
[19] Yu T [Dissertation]. Randomized controlled clinical study of “Dredge Du Channel and Regulate Marrow” with Electric Acupuncture on Mild Cognitive Impairment. Chengdu (China): Chengdu University of Traditional Chinese Medicine; 2010. [in Chinese].
[20] Chen ZG [Dissertation]. A Multicenter Randomized Controlled Trial on Treatment of Mild Cognitive Impairment by Electric Scalp Acupuncture.
Chengdu (China): Chengdu University of Traditional Chinese Medicine;
2011. [in Chinese].
[21] Li KS [Dissertation]. Clinical Observation on the Treatment of Mild Cognitive Impairment by Combined Acupuncture and Medication. Harbin (China): Heilongjiang University of Chinese Medicine; 2011. [in Chinese].
[22] Li MP [Dissertation]. Clinical Observation on the Treatment of Mild Cognitive Impairment by Combined Acupuncture and Yizhiyin. Harbin (China): Heilongjiang University of Chinese Medicine; 2012. [in Chinese].
[23] Zhang ZJ, Yuan WQ, Zhang JY, Zhang YF, Li JM, Tian HJ et al. Clinical Observation on the Treatment of Mild Cognitive Impairment by Combined Acupuncture and Nimodipine, Naoxingtong Capsules. Med Innov Chin 2012;9:40-41. [in Chinese].
[24] Zhao Y. Efficacy of Acupuncture Combined with Nimodipine in the Treatment of Mild Cognitive Impairment. Chin J Clin Ration Drug Use 2012;5:16-17. [in Chinese].
[25] Zhang H, Zhao L, Yang S, Chen ZG, Li YK, Peng XH et al. Clinical observation on effect of scalp electroacupuncture for mild cognitive impairment. J Tradit Chin Med 2013;33:46-50.
[26] Du L [Dissertation]. Study of Tongdu Tiaoshen Acupuncture on Mild Cognitive Impairment Patients with Serum BDNF Effect. Hefei (China):
Anhui University of Chinese Medicine; 2015. [in Chinese].
[27] Wang J, Li X, Xia DJ. Clinical Observation on Treatment of Mild Cognitive Impairment by Acupuncture Combined with Jiangzhi Yizhi Granule.
Zhejiang J Integr Tradit Chin West Med 2015;25:908-911. [in Chinese].
[28] Li X [Dissertation]. Clinical Observation on the Treatmnet of Mild Cognitive Impairment by combined Acupuncture and Jiangzhi Yizhi granule. Hangzhou (China): Zhejiang Chinese Medical University; 2016. [in Chinese].
[29] Chen J [Dissertation]. Clinical Observation on the Five Elements of Acupuncture in the Treatment of the Patients with Mild Cognitive Impairment. Nanning (China): Guangxi Traditional Chinese Medical University; 2017. [in Chinese].
[30] Liu L [Dissertation]. Clinical Observation on Herapeutic effect of Mild Cognitive Impairment by Yu style Cluster Acupuncture. Harbin (China):
Heilongjiang University of Chinese Medicine; 2017. [in Chinese].
[31] Tan TT, Wang D, Huang JK, Zhou XM, Yuan X, Liang JP et al. Modulatory effects of acupuncture on brain networks in mild cognitive impairment patients. Neural Regen Res 2017;12:250-258.
[32] Hu J, Zhang N, Wang ZX, Liang YW, Qian Q. Systematic review of acupuncture in treating mild cognitive impairment. Chin J Ethnomed Ethnopharma 2014;12:17-21. [in Chinese].
[33] Mai W, Zheng JH. Clinical Efficacy of Scalp Acupuncture on Mild Cognitive Impairment: A Meta-analysis Study. J Liaoning University Tradit Chin Med 2015;17:121-124. [in Chinese].
[34] Wang Y [Dissertation]. The Study of Minimum Mental State Examination, blood lipid and the Analysis of Acupuncture and Moxibustion Treatment of MCI. Nanning (China): Guangxi Traditional Chinese Medical University;
2017. [in Chinese].
[35] Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions Version 5.1.0. Chichester (UK): John Wiley & Sons, Ltd; 2011.
[36] Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomized Trials. Int J Surg 2011;9:672-677.