106
Korean Circulation J 2005;35:106-114 ⓒ 2005, The Korean Society of Circulation
Effect of Distal Protection Device on the Microvascular Integrity during Primary Stenting in Acute Myocardial Infarction:
Distal Protection Device in Acute Myocardial Infarction
Myeong-Ho Yoon, M.D., Seung-Jea Tahk, M.D., So-Yeon Choi, M.D., Tae-Young Choi, M.D., Byoung-Joo Choi, M.D., Jung-Hyun Choi, M.D., Sang-Yong Yoo, M.D., Sung-Gyun Ahn, M.D., Zhen-Guo Zheng, M.D., Gyo-Seung Hwang, M.D. and Joon-Han Shin, M.D.
Department of Cardiology, Ajou University School of Medicine, Suwon, Korea ABSTRACT
Background and Objectives:Phasic coronary flow velocity patterns and microvascular integrities are known to be prognostic factors in acute myocardial infarction (AMI). The use of a distal protection device during primary percutaneous coronary interven- tion (PCI) may preserve the microvascular integrity of the myocardium by preventing distal embolization of thrombotic materials.
This study assessed the effects of such a device on microvascular integrity preservation through Doppler studies of the coronary flow velocities in AMI patients treated with primary PCI. Subjects and Methods:A total of fifty-eight consecutive patients (mean age 54±15, 46 males) with ST segment-elevated AMI, who had undergone primary PCI within 24 hours after onset, were enrolled in the study. The subjects were divided into two groups: 30 patients with the PurcuSurge GuardWire Temporary Occlusion and Aspiration System and 28 without. The TIMI flows and TMP grades (TIMI myocardial perfusion grade) were evaluated. The coronary flow velocities were measured after PCI with a Doppler wire at the baseline, and also after intracoronary adenosine (24-48 μg) induced hyperemia. The coronary flow velocity reserve (CFR), diastolic deceleration time (DDT) and microvascular resistance index (MVRI) were calculated. Results:Between the two groups, no significant differences were found in the angiographic characteristics and CFR. In patients with a distal protection device, however, the post-PCI TMP grades were more favorable (TMP 0/1: 13.3%, TMP 2:
23.3%, TMP 3: 63.4% vs. TMP 0/1: 35.7%, TMP 2: 35.7%, TMP 3: 28.6%, p=0.023), with TMP grade 3 being most common (63.4% vs. 28.6%, p=0.010). These patients also exhibited lower bMVRI and hMVRI levels (4.33±2.22 vs. 5.55±2.36 mmHg · m-1·sec (p=0.047) and 2.39±1.40 vs. 3.14±1.36 mmHg·cm-1 · sec (p=0.045), respectively), and longer bDDT and hDDT (679±273 vs. 519
±289 msec (p=0.035) and 761±256 vs. 618±272 msec (p=0.044), respectively). Conclusions:Distal protection with the Purcu- Surge GuardWire system may effectively preserve the microvascular integrity of the myocardium during primary PCI in AMI patients. (Korean Circulation J 2005;35:106-114)
KEY WORDS:Myocardial infarction;Microvascular integrity.
Introduction
Acute myocardial infarction(AMI) is commonly related with thrombotic occlusion following a plaque rupture. Accor- dingly, early relief of the occluded coronary artery and res- toration of the coronary flow to the jeopardized myocardium have been demonstrated to decrease mortality and adverse outcomes.1-3) Primary percutaneous coronary intervention (PCI), with stent deployment, in AMI cases has been widely
performed for restoring the coronary flow to the jeopardized myocardium, a more effective procedure than balloon angio- plasty, decreasing the target vessel revascularization and res- tenosis rate.4-6) However, as the distal embolization of ruptured atherosclerotic plaque debris or thrombus is common during primary PCI with catheter-based interventions, stent deploy- ment may also endow a greater chance of distal embolization than balloon angioplasty.6) Evidence that an obstruction of the distal microvasculature in the downstream bed of the infarct related artery(IRA) is caused by distal embolization of thrombotic materials and platelets during intervention has accumulated. These are critical pathophysiologic events of myocardial infarction,7-9) which is subsequently related with slow-flow or no-reflow phenomenon and with additional injury to the microvasculature of the myocardium and poor
Received:November 3, 2004 Accepted:February 1, 2005
Correspondence:Seung-Jea Tahk, M.D.,Department of Cardiology, Ajou University School of Medicine, San 5, Wonchun-dong, Youngtong-gu, Suwon 442-721, Korea
Tel:82-31-219-5723, Fax:82-31-219-5708 E-mail:sjtahk@ajou.ac.kr
clinical outcomes.10-12) Recanalization and restoration of the epicardial coronary artery will not always guarantee reperfu- sion at the microvasculature of the myocardium. Therefore, reperfusion of the myocardial tissue level by preserving the microvasculature is crucial, as is opening of the epicardial coronary artery during primary PCI. It has been suggested that a distal embolization protection device may be a feasible, safe and effective tool in preserving the microvasculature of the myocardium due to prevention of distal embolization of thrombotic debris during primary PCI in AMI.13-16) The coro- nary angiographic TIMI myocardial perfusion(TMP) gra- de17)18) and phasic coronary flow velocity patterns, as assessed by intracoronary Doppler wire after primary PCI, both of which represent the myocardial reperfusion status and mi- crovascular integrity of the IRA, were related to functional improvement of the left ventricle and prognosis of the pa- tient.19)20) Herein, the effectiveness of the PurcuSurge Guard- Wire system in preserving the microvascular integrity of the myocardium during primary PCI was evaluated in AMI pa- tients by assessing the TMP grades and phasic coronary flow velocity patterns of the IRA following primary PCI with stenting.
Subjects and Methods
Patient population
A total of fifty-eight patients(mean age: 54±15 years; 46 male, 12 female) with first acute ST-segment elevated myo- cardial infarction, who had experienced primary PCI within 24 hours of symptom onset, were enrolled in this study. The diagnosis of AMI was based on characteristic chest pains that had persisted in excess of 30 minutes, significant ST seg- ment elevation(>1 mm at limb lead and 2>mm at precordial lead) in ≥2 contiguous ECG leads, and an elevation of the myocardial band of creatine phosphokinase(CK-MB) ≥3 times of the upper normal limit. The exclusion criteria in- cluded the followings; 1) previous myocardial infarction, 2) cardiogenic shock, 3) previous history of coronary interven- tion or coronary artery bypass graft, 4) left main disease and 5) patients with significant tachy-arrhythmia or atrio-ventri- cular block, rendering an intracoronary Doppler study inap- propriate. The study population was divided into two groups:
30 patients(group A) with the PurcuSurge GuardWire® Tem- porary Occlusion and Aspiration System(Medtronic AVE, Santa Rosa, CA) and 28 patients(group B) without such protection during primary PCI.
Procedure
On admission, all patients were pretreated with chewable aspirin(300 mg) and clopidogrel(300-600 mg). An intra- venous infusion of heparin was started(1000 U/hr) after a 5000 U intravenous bolus injection, and additional heparin administered to attain a minimum 300 seconds of activated clotting time during the procedure. After a 7 Fr guiding catheter was engaged to the IRA, via the femoral artery, a 0.014-inch GuardWire was advanced directly(or, in cases where the GuardWire could not directly pass the culprit lesion, with the use of a steerable coronary angioplasty gui- dewire for backup). The occlusion balloon of the GuardWire was positioned distal to the culprit lesion. Following actua- tion of the MicroSeal adapter, the distal occlusion balloon of the GuardWire was inflated using an EZ-flator with diluted contrast media(1/3 contrast media and 2/3 heparinized nor- mal saline). The balloon size was adjusted according to the distal reference vessel size. In some patients, for the evalua- tion of the distal vessel diameter and side branches, a small amount of contrast was injected through the guiding catheter before inflation of the distal occlusion balloon of GuardWire.
When protection of the distal circulation had been achieved through the system, the MicroSeal Adapter was removed, leaving the distal occlusion balloon in an inflated state. Sub- sequent to stent deployment, a 5 Fr monorail aspiration ca- theter(Export® Aspiration Catheter) was loaded over the proximal end of the GuardWire, with several aspirations per- formed using the plunger of aspiration syringe. At the end of the procedure, angiography was performed to document the final TIMI flow grade and TMP grade.
Measurement of coronary flow velocity parameters and assess- ment of phasic coronary flow velocity patterns with intracoro- nary Doppler guide wire
After stenting and aspiration of the embolized materials, 100-300 μg nitroglycerin was administrated into the coro- nary artery, and a 0.014-inch Doppler guide wire(FloWireTM, Cardiometrics, Mountain View, CA, USA) introduced just distal to the culprit lesion. Maximal hyperemia was induced by a bolus of intracoronary adenosine administration(24 μg for the right coronary artery, 48 μg for the left coronary artery). The coronary flow velocity reserve(CFR) was de- fined as the ratio of the hyperemic averaged peak velocity (APV) to the baseline APV. The microvascular resistance index(MVRI) was calculated from the mean aortic blood pressure divided by the averaged peak velocity at the base-
line and during hyperemia, respectively. In three consecutive cardiac cycles at the baseline and during hyperemia, the de- celeration time of the diastolic flow velocity(DDT) were measured and averaged for their mean values(Fig. 1).
Statistical analysis
Data are expressed as percentages for discrete variables and as the mean ±standard deviation for continuous varia- bles. The continuous variables of the clinical, angiographic and intracoronary Doppler flow data were compared by the means between the two groups using the Student t-test. The categorical variables of the clinical characteristics, angiogra- phic TIMI and TMP grades, were compared by χ2 analysis or the Fisher exact test. A p of <0.05 was considered to in- dicate statistical significance.
Results
Clinical characteristics
The study population consisted of 58 consecutive patients, 46 men and 12 women, with a mean age of 54±15 years.
The clinical and laboratory data of both groups are summa- rized in Table 1. Of the 58 patients, 38, 17 and 3 had anterior, inferior and 3 lateral wall infarctions, respectively. All patients underwent echocardiography on admission or immediately after primary PCI. The mean ejection fraction was 52.5±
10.3%. The mean time elapsed from symptom onset to re- perfusion with primary PCI was 392±228 minutes. There were no significant differences in the clinical characteristics between the two groups, with the exception of the peak car- diac enzymes. The peak CK-MB was lower in group A than in group B patients(256±165 vs. 379±166 μg/mL, p=
0.011). No patient received glycoprotein IIb/IIIa inhibitors
before or during PCI.
Angiographic data
Table 2 and 3 summarize the angiographic data obtained before and after primary PCI. Before and after the primary PCI with stenting, the mean of minimal lumen diameter (MLD), diameter of stenosis(DS) and reference vessel dia- meter(RVD) were insignificant between the two groups.
Also, there was no significant difference in the respective TIMI flow grades before intervention(p=0.699)(Table 3).
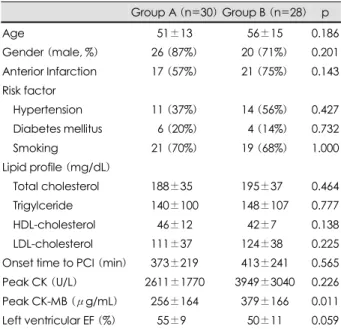
Table 1. Comparison of the clinical and laboratory characte- ristics
Group A (n=30) Group B (n=28) p Age 51±13 56±15 0.186 Gender (male, %) 26 (87%) 20 (71%) 0.201 Anterior Infarction 17 (57%) 21 (75%) 0.143 Risk factor
Hypertension 11 (37%) 14 (56%) 0.427 Diabetes mellitus 06 (20%) 04 (14%) 0.732 Smoking 21 (70%) 19 (68%) 1.000 Lipid profile (mg/dL)
Total cholesterol 188±350 195±370 0.464 Trigylceride 140±100 148±107 0.777 HDL-cholesterol 46±12 42±70 0.138 LDL-cholesterol 111±370 124±380 0.225 Onset time to PCI (min) 373±219 413±241 0.565 Peak CK (U/L) 2611±1770 3949±3040 0.226 Peak CK-MB (μg/mL) 256±164 379±166 0.011 Left ventricular EF (%) 55±90 50±11 0.059 Group A: patient with the PurcuSurge GuardWire, Group B: with- out the PurcuSurge GuardWire, HDL-cholesterol: high density lipoprotein-cholesterol, LDL-cholesterol: low density lipoprotein cholesterol, CK: creatine kinase, CK-MB: creatine kinase-myo- cardial band, EF: ejection fraction
Table 2. Comparison of the quantitative coronary angiographic results
Group A (n=30)
Group B (n=28) p Pre-intervention Minimal lumen diameter (mm) 0.17±0.27 0.22±0.41 0.608 Diameter stenosis (%) 96±70 93±13 0.326 Post-stent Minimal lumen diameter (mm) 3.0±0.4 3.0±0.5 0.607 Diameter stenosis (%) 12±70 12±90 0.900 Reference vessel size (mm) 3.3±0.4 3.4±0.5 0.647
Infarct related artery 0.143
Left anterior descending 17 (57%) 21 (75%) Left circumflex 03 (10%) 00 (0%)0 Right coronary 10 (33%) 07 (25%) Group A: patient with the PurcuSurge GuardWire, Group B: with- out the PurcuSurge GuardWire
Fig. 1. Measurement of the DDT, which was measured as the average of 3 consecutive cycles. DDT: deceleration time of the diastolic flow velocity. LAD: left anterior descending coronary artery.
DDT
After the primary PCI, the TIMI flow grades were more improved in patients with the distal protection device(group A) compared to those without(group B)(93.4% had TIMI grade 3, 3.3% grade 2 and 3.3% grades 0 or 1 in group A vs.
75.0, 25.0 and 0.0%, respectively, in group B, p=0.040) (Table 3). A significant difference was found in the respec- tive TMP grades between the two groups after the primary PCI(63.4% had TMP grade 3, 23.3% grade 2 and 13.3%
grades 0 or 1 in group A vs. 28.6, 35.7 and 35.7%, respec- tively, in group B, p=0.023)(Table 3)(Fig. 2A). Further, TMP grade 3 was more common in group A(63.4 vs. 28.6%, p=0.010). In 49 patients who achieved TIMI 3 flow after stenting, TMP grade 3 was also more common in group A (67.9 vs. 38.1%, p=0.048)(Fig. 2B).
Coronary flow velocity parameters and phasic coronary flow velocity patterns
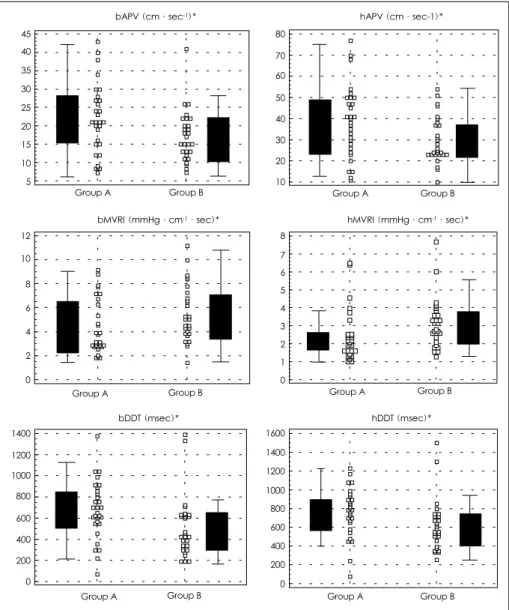
The heart rate and baseline mean aortic blood pressure were no different between the two groups. The hyperemic mean aortic pressure was lower in Group A than in Group B (74±12 vs. 83±17 mmHg, p=0.026). After the primary PCI, the bAPV and hAPV were higher in group A(21.6±
9.6 vs. 17.2±7.0 cm/sec, p=0.050; and 38.4±16.8 vs. 29.9
±11.0 cm/sec, p=0.027, respectively), and the bMVRI and hMVRI were lower in group A(4.33±2.22 vs. 5.55±2.36 mmHg·cm-1·sec, p=0.045; and 2.40±1.40 vs. 3.14±1.37 mmHg·cm-1·sec, p=0.045, respectively). However, the CFR was no different between the two groups(1.87±0.66 vs. 1.84±0.61, p=0.867). Early systolic reversal flow was
documented in 1 patient with the distal protection device, compared with 2 without. The bDDT and hDDT were signi- ficantly longer in group A(679±274 vs. 520±289 msec, p=0.035; and 761±256 vs. 618±272 msec, p=0.044, res- pectively)(Table 4)(Fig. 3).
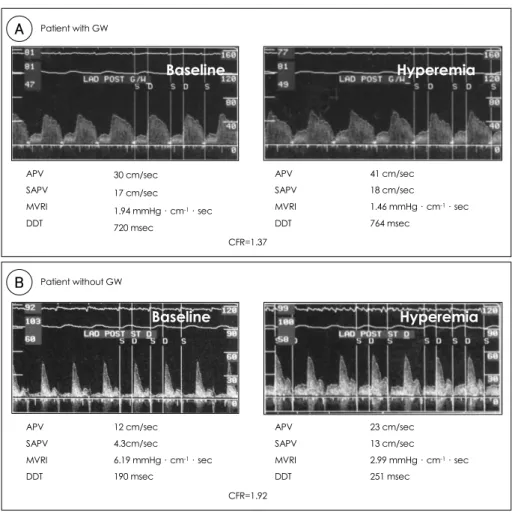
The comparative phasic coronary flow velocity patterns in cases with and without the distal protection device are illu- strated in Fig. 4A, B, respectively.
Discussion
The aim of AMI treatment is the early and sustained reperfusion of the myocardium at risk. As such, primary PCI is widely performed for the restoration of the coronary flow and reperfusion to the jeopardized myocardium. Recently, primary PCI with stent deployment in AMI has been re- garded as the optimal therapeutic regimen for the reperfusion of IRA, with lowering of the target vessel revascularization
Table 3. Comparison of the pre-intervention and post-stent an- giographic results of the TIMI and TMP grade
Group A (30) Group B (28) p
Pre-PCI 0.699
TIMI 0/1 20 (66.7%) 20 (71.4%) TIMI 2 07 (23.3%) 04 (14.3%) TIMI 3 03 (10.0%) 04 (14.3%)
Post-stent
TIMI flow 0.040
TIMI 0/1 01 (03.3%) 00 (00.0%) TIMI 2 01 (03.3%) 07 (25.0%) TIMI 3 28 (93.4%) 21 (75.0%)
TMP grade 0.023
TMP 0/1 04 (13.3%) 10 (35.7%) TMP 2 07 (23.3% 10 (35.7%) TMP 3 19 (63.4%) 08 (28.6%)
Group A: patient with the PurcuSurge GuardWire, Group B: with- out the PurcuSurge GuardWire, TIMI: thrombolysis in myocardial infarction, TMP: TIMI myocardial perfusion grade
Fig. 2. Post-stent TMP grade in the studied patients (panel A) and in selected patients with final TIMI 3 flow. The post-PCI TMP grade was more favorable in patients with a distal protection device than in those without (p=0.023) TMP grade 3 was ob- tained in 67.9and 38.1% in Groups A & B, respectively (p=0.048, by Chi-square analysis). Group A: patient with the PurcuSurge GuardWire, Group B: patients without the PurcuSurge GuardWire.
0 10 20 30 40 50 60 70
Group A (n=30) Group B (n=28)
p=0.023
TMP 3 TMP 2 TMP 0/1
35.3
13.3 23.3 35.3
28.6
63.4
A
% of Patients
0 10 20 30 40 50 60 70 80
Grup A (n=30) Group B (n=28) TMP 3
TMP 2 TMP 0/1
7.1
28.6 33.3 38.1 25.0
67.9
p=0.048
B
% of Patients
and rate of restenosis during the first 30-days and long-term follow-ups.4-6) However, primary angioplasty with stent de- ployment has shown no more improvement to the TIMI flow grade than primary balloon angioplasty. This might be explained by the higher likelihood of distal embolization of thrombotic materials during intervention with stent deploy- ment.6) During primary PCI with either a stent or balloon, the slow-flow or no-reflow phenomenon occurred about 5-30%
of AMI patients.10-12) The no-reflow phenomenon, which represents a severely damaged microvascular integrity of the myocardium, contributes to poor left ventricular functional improvement and negative clinical prognosis of AMI pa- tients.10-12) Although the precise mechanisms of the no-reflow phenomenon have not been fully clarified, increasing evi- dence suggests the phenomenon might be related with em- bolization of athero and/or thrombotic debris, plugging with platelets and inflammatory cells, endothelial and myocardial edema, and the shedding of vasoactive proteins from the plaque.21-23) Angiographic evidence of distal embolization during primary PCI occurs in approximately 15% of cases, which is associated with a more extensive myocardial da- mage and poorer prognosis than when not seen.9) A distal protection device might be expected to protect the micro- vascular integrity of the myocardium by preventing em-
bolization of thrombotic materials during primary PCI in AMI patients. Recently, thrombosuction before the actual an-gioplasty, with an export aspiration catheter, in primary PCI has achieved excellent angiographic results, with all target vessels achieving TIMI grade 3 flow.15) TIMI grade 3 flow is generally regarded as a successful reperfusion after PCI in AMI,24) which results in more desirable left ventri- cular functional outcomes compared to TIMI grade 0-2 flows.25)26)
In our study, no difference in the pre-PCI TIMI grades were shown between the two groups; however, the post-PCI TIMI grades significantly improved in patients with the distal protection device(group A) than in those without(group B).
TIMI grade 3 flow was significantly more common in group A. These results showed that the use of the distal protection device was more desirable in restoring the epicardial co- ronary blood flow in AMI patients during primary PCI. Ho- wever, the TIMI grade 3 flow had inhomogeneous hemody- namic characteristics, with a wide range of coronary flow velocity values, and some patients had less optimal reperfu- sion at the myocardial tissue level, which may be related to the different clinical outcomes.9)18)
Gibson et al17) developed the TMP grading system, a simple semiquantitative classification scheme, which can be used to characterize the filling and clearance of myocardial perfusion from an angiogram. The TMP grading system, using coronary angiography in the catheterization laboratory, facilitates the detection of microvascular obstruction as a cause of impaired myocardial perfusion, and implicated distal embolization as the most likely explanation for microvascular plugging. They reported that the TMP grading system pro- vides independent risk stratification after thrombolytics in AMI. TMP 0/1 grades showed a three-fold increase in the 30-day mortality rates compared to TMP 3 grade, and even among patients with TIMI grade 3 flow, TMP 0/1 grade correlated with a seven-fold increase in the mortality rates compared to TMP 3 grade.
Huang et al14) reported that a distal protection device with a temporary occlusion system might be feasible, safe and ef- fective during primary angioplasty in AMI. They reported that all patients with such a device had procedural success and exhibited positive results with respect to TMP grades (86.7% of patients achieved TMP grade 3), with none de- veloping an angiographic no-reflow phenomenon. Yip et al16) reported the PurcuSurge device during primary PCI to be superior to adjunctive tirofiban therapy in terms of the epi-
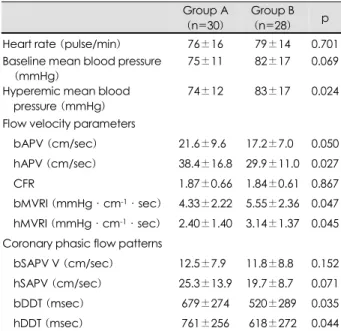
Table 4. Comparison of the hemodynamics, coronary flow velo- city and phasic coronary flow velocity patterns
Group A (n=30)
Group B (n=28) p Heart rate (pulse/min) 76±16 79±14 0.701 Baseline mean blood pressure
(mmHg)
75±11 82±17 0.069 Hyperemic mean blood
pressure (mmHg)
74±12 83±17 0.024
Flow velocity parameters
bAPV (cm/sec) 21.6±9.60 17.2±7.00 0.050 hAPV (cm/sec) 38.4±16.8 29.9±11.0 0.027 CFR 1.87±0.66 1.84±0.61 0.867 bMVRI (mmHg·cm-1·sec) 4.33±2.22 5.55±2.36 0.047 hMVRI (mmHg·cm-1·sec) 2.40±1.40 3.14±1.37 0.045 Coronary phasic flow patterns
bSAPV V (cm/sec) 12.5±7.90 11.8±8.80 0.152 hSAPV (cm/sec) 25.3±13.9 19.7±8.70 0.071 bDDT (msec) 679±274 520±289 0.035 hDDT (msec) 761±256 618±272 0.044 Group A: patient with the PurcuSurge GuardWire, Group B: with- out the PurcuSurge GuardWire, b, hAPV: baseline, hyperemic average peak velocity, CFR: coronary flow velocity reserve, b, hMVRI: baseline, hyperemic microvascular resistance index, b, hSAPV: baseline, hyperemic systolic average peak velocity, b, hDSVR: baseline, hyperemic diastolic and systolic velocity ratio, b, hDDT: baseline, hyperemic diastolic deceleration time
cardial flow, TMP grades and 30-day clinical outcomes. In our study, the post-PCI TMP grades were more favorable in group A than B. TMP grade 3 was also more common in group A and in 49 selected patients with TIMI grade 3 flow after primary PCI, TMP grade 3 was also more common in group A. These results suggested that a distal protection de- vice is more effective in the recovery of reperfusion at the myocardial tissue level, which may be effective in preserving the micorvascular integrity of the myocardium during pri- mary PCI.
The CFR and phasic coronary flow velocity patterns are known to be prognostic factors for left ventricular functional improvement and for the clinical prognosis in AMI.19)20)27)28)
We directly evaluated the microvascular function by asses- sing the coronary flow velocity and coronary flow velocity
patterns using an intracoronary Doppler wire after primary PCI. In severely damaged myocardium, with diffuse obstruc- tion of the microvasculature due to cell necrosis or multiple microvascular emboli, the distal coronary pressure increased and the coronary flow velocity rapidly decreased as a result of the increased microvascular resistance. Therefore, the in- creased microvascular resistance after relief of the epicardial stenosis with stenting may be related with severely damaged myocardium and microvascular dysfunction.12) In group A, the bAPV and hAPV were significantly higher and the bMVRI and hMVRI significantly lower than in group B.
The higher APV and lower MVRI strongly suggested that patients with the distal protection device, compared to those without, had less damage, with preserved microvascular cir- culation of the infarct-related myocardium, due to the pre-
Fig. 3. Comparison of coronary flow velocity, MVRI and DDT between patients with and without a distal protection device. Group A:
patient with the PurcuSurge GuardWire, Group B: patients without the PurcuSurge GuardWire, b: baseline, h: hyperemic, APV: average peak velocity, MVRI: microvascular resistance index, DDT: diastolic deceleration time, *: p<0.05 between two groups.
Group B Group A
bAPV (cm·sec-1)*
45 40 35 30 25 20 15 10 5
Group A Group B bMVRI (mmHg·cm-1·sec)*
12 10
8 6 4 2 0
Group B Group A
bDDT (msec)*
1400 1200 1000 800 600 400 200 0
Group B Group A
hAPV (cm·sec-1)*
80 70 60 50 40 30 20 10
Group A Group B hMVRI (mmHg·cm-1·sec)*
8 7 6 5 4 3 2 1 0
Group B Group A
hDDT (msec)*
1600 1400 1200 1000 800 600 400 200 0
vention of distal embolization during primary PCI.
The CFR, as assessed immediately after the primary PCI, and within 24 hours of myocardial infarction onset, showed no difference in the left ventricular wall motion between the recovered and non-recovered groups,29) so was not conside- red to be an indicator of viable myocardium and left ven- tricular functional improvements in AMI patients. Hori et al30) reported that the changes in the coronary blood flow after acute embolization were related to the extent of embo- lization. In a resting state, the coronary blood flow is ma- intained or even enhanced due to the hyperemia of non- occluded vessels. As the particulate burden begins to overw- helm the compensatory mechanisms, the coronary flow de- creases almost linearly as embolization increases. However, in an adenosine-induced hyperemic state, according to the increased embolization, the hyperemic coronary flow pro- gressively decreases, without a transient increase of the blood flow. In our study, the CFR showed no difference between
the two groups. However, in group A, the bAPV was signifi- cantly higher, which may have been related to the compen- satory hyperemic response due to the relatively small amount of distal embolization in patients with the distal protection device than in those without. Therefore, the CFR in this stu- dy might have been underestimated after primary PCI in the patients with the device.
In AMI patients with severe extensive damaged myocar- dium, the myocardial blood pool should be considerably decreased and the microvascular resistance increased. These facts may impact on the coronary flow velocity patterns. In these patients, coronary blood flows rapidly fill the residual intramyocardial blood pool during the diastolic phase, but soon rapidly decrease thereafter. As such, in patients with severe extensive damaged myocardium, the coronary flow velocity showed rapid deceleration of the diastolic flow. Du- ring the systolic phase, the coronary flow resulted in an early systolic retrograde flow or a decreased systolic flow.12) Thus,
Fig. 4. Phasic coronary flow velocity patterns and CFR in patient with and without a distal protection device (A & B, respectively). In patient with a distal protection device, the CFR was 1.37 and the coronary flow velocity patterns and microvascular resistance index were favorable. In patients without a distal protection device, the CFR was 1.92 and the coronary flow velocity patterns and micro- vascular resistance index were unfavorable. Note: the baseline APV of patient with distal protection was higher than that of those without, which might result in a low CFR value. GW: PurcuSurge GuarWire, APV: average peak velocity, SAPV: systolic average peak velocity, MVRI: microvascular resistance index, DDT: diastolic deceleration time, CFR: coronary flow velocity reserve.
Baseline Hyperemia
APV SAPV MVRI DDT
A
CFR=1.37 30 cm/sec
17 cm/sec
1.94 mmHg·cm-1·sec 720 msec
APV SAPV MVRI DDT
41 cm/sec 18 cm/sec
1.46 mmHg·cm-1·sec 764 msec
Patient with GW
APV SAPV MVRI DDT
B
CFR=1.92 12 cm/sec
4.3cm/sec
6.19 mmHg·cm-1·sec 190 msec
APV SAPV MVRI DDT
23 cm/sec 13 cm/sec
2.99 mmHg·cm-1·sec 251 msec
Patient without GW
Baseline Hyperemia
an early systolic retrograde flow or a decreased systolic flow velocity, with rapid deceleration of the diastolic flow velocity, may be representative of severe damage to the microvascular integrities of infarct-related myocardium. In the study by Kawamoto et al,19) a systolic averaged peak flow velocity (SAPV) less than 6.5 cm/sec and a DDT less than 600 msec, assessed just after primary PCI, were related with poor re- covery of the left ventricular function. Akasaka et al,20) also reported that unfavorable coronary flow velocity patterns, such as decreased DDT and SAPV or early systolic reversal flow, in TIMI 2 grade after primary PCI, were related to se- vere damage of the myocardium and poor functional re- covery of the left ventricle.
Our study showed that patients with the distal protection device exhibited more favorable coronary flow velocity pa- tterns. The bDDT and hDDT were significantly longer in pa- tients with the device. These results indicate a preserved mi- crovascular pool and less damage of the myocardium in pa- tients with the device. Therefore, the PurcuSurge GuardWire® Temporary Occlusion and Aspiration System may be effective in preserving the microvascular integrity due to prevention of atherothrombotic microembolization or large particular embolization during primary PCI in AMI patients.
Limitation
This study was limited in several respects. First, it was not randomized in nature, with only a relatively small number of patients assessed. However, there were no significant clinical and angiographic characteristic differences between the two groups. Despite the small study population, statistically sig- nificant differences in the TIMI grade, TMP grade, MVRI and phasic coronary flow patterns were also observed bet- ween the two groups. These results may strongly suggest the effectiveness of the distal protection device in the preserva- tion of myocardial integrities during primary PCI in AMI pa- tients. Second, the coronary flow velocity and coronary flow velocity patterns might be affected, not only the microvas- cular integrity, but the infarct location and other hemodyna- mic factors also. In this study, the infarct locations between the two groups were no different. Also, there was no signifi- cant difference in the hemodynamic factors, with the excep- tion of the hyperemic mean aortic pressure. However, the hy- peremic mean aortic pressure was higher in patients without the distal protection device. Further studies will be required to evaluate the follow-up results for the left ventricular func- tion and clinical outcomes.
Conclusion
This study is the first to show the effectiveness of the PurcuSurge GuardWire system as a distal protection device for preserving the microvascular integrity according to the coronary flow reserve, microvascular resistance indexes and phasic coronary flow velocity patterns using an intracoronary Doppler wire. The distal protection device is feasible and effective in the preservation of the microvascular integrity during primary PCI in AMI patients.
REFERENCES
1) Gibson CM, Murphy SA, Rizzo MJ, et al. Relation between TIMI frame count and clinical outcomes after thrombolytic administration. Circulation 1999;99:1945-50.
2) Puma JA, Skech MH Jr, Thompson TD, et al. Support for the open-artery hypothesis in survivors of acute myocardial infarc- tion: analysis of 11228 patients treated with thrombolytic therapy.
Am J Cardiol 1999;83:482-7.
3) White HD, Cross DB, Elliott JM, Norris RM, Yee TW. Long- term prognostic importance of the infarct-related coronary artery after thrombolytic therapy for acute myocardial infarction. Cir- culation 1994;89:61-7.
4) Stone GW, Brodie BR, Griffin JJ, et al. Clinical and angiogra- phic follow-up after primary stenting in acute myocardial infarc- tion. Circulation 1999;99:1548-54.
5) Stone GW, Grines CL, Cox DA, et al. Comparison of angioplas- ty with stenting, with or without abciximab, in acute myocardial infarction. N Engl J Med 2002;346:957-66.
6) Grines CL, Cox DA, Stone GW, et al. Coronary angioplasty with or without stent implantation for acute myocardial infarction. N Engl J Med 1999;341:1949-56.
7) Califf RM, Abdelmeguid AE, Kuntz RE, et al. Myonecrosis after revascularization procedure. J Am Coll Cardiol 1998;31:241-51.
8) Topol EJ, Yadav JS. Recognition of the importance of emboliza- tion in atherosclerotic vascular disease. Circulation 2000;101:
570-80.
9) Henriques JP, Zijlstra F, Ottervanger JP, et al. Incidence and cli- nical significance of distal embolization during primary angio- plasty for acute myocardial infarction. Eur Heart J 2002;23:
1112-7.
10) Ito H, Tomooka T, Sakai N, et al. Lack of myocardial perfusion immediately after successful thrombolysis: a predictor of poor recovery of left ventricular function in anterior myocardial in- farction. Circulation 1992;85:1699-705.
11) Ito H, Maruyama A, Iwakura K, et al. Clinical implications of the ‘no-reflow’ phenomenon: a predictor of complications and left ventricular remodeling in reperfused anterior wall myocardi- al infarction. Circulation 1996;93:223-8.
12) Ito H, Iwakura K. Assessing the relation between coronary re- flow and myocardial reflow. Am J Cardiol 1998;81(Supple 12A): 8G-12G.
13) Kalaria VG, Rouch C, Bourdillon PD, Breall JA. Distal emboli protection in patients undergoing percutaneous coronary inter- vention after myocardial infarction. Catheter Cardiovasc Interv 2002;57:54-60.
14) Huang Z, Katoh O, Nakamura S, Negoro S, Kobayashi T, Ta- nigawa J. Evaluation of the percusurge guardwire plus tempo- rary occlusion and aspiration system during primary angio- plasty in acute myocardial infarction. Catheter Cardiovasc Interv
2003;60:443-51.
15) Wang HJ, Kao HL, Liau CS, Lee YT. Export aspiration catheter thrombosuction before actual angioplasty in primary coronary intervention for acute myocardial infarction. Catheter Cardio- vasc Interv 2002;57:332-9.
16) Yip HK, Wu CJ, Chang HW, Fang CY, Yang CH, Chen SM.
Effect of the Percusurge guardeire device on the integrity of mi- crovasculature and clinical outcomes during primary transradial coronary intervention in acute myocardial infarction. Am J Car- diol 2003;92:1331-5.
17) Gibson CM, Cannon CP, Murphy SA, et al. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 2000;101:125-30.
18) Stone GW, Peterson MA, Lansky AJ, Dangas G, Mehran R, Leon MB. Impact of normalized myocardial perfusion after successful angioplasty in acute myocardial infarction. J Am Coll Cardiol 2002;39:591-7.
19) Kawamoto T, Yoshida K, Akasaka T, et al. Can coronary flow velocity pattern after percutaneous transluminal coronary an- gioplasty (correlation of angiography) predict recovery of re- gional left ventricular function in patients with acute myocardial infarction? Circulation 1999;100:339-45.
20) Akasaka T, Yoshida K, Kawamoto T, et al. Relation of phasic coronary flow velocity characteristics with TIMI perfusion grade and myocardial recovery after primary percutaneous translumi- nal coronary angioplasty and rescue stenting. Circulation 2000;
101:2361-7.
21) Kloner R, Ganote CE, Jennings RB. The “no-reflow” pheno- menon after temporary coronary occlusion in the dog. J Clin Invest 1974;54:1496-508.
22) Kloner RA, Giacomelli F, Alker K, Hale S, Matthews R, Bel- lows B. Influx of neutrophils into the walls of large epicardial
coronary arteries in response to ischemia/reperfusion. Circula- tion 1991;84:1758-72.
23) Bonderman D, Teml A, Jakowitch J, et al. Coronary no-reflow is caused by shedding of active tissue factor from dissected athe- rosclerotic plaque. Blood 2002;99:2794-800.
24) Smith SC Jr, Dove JT, Jacobs AK, et al. ACC/AHA guidelines for percutaneous coronary intervention (revision of the 1993 PTCA guidelines): executive summary. Circulation 2001;103:
3019-41.
25) Simes RJ, Topol EJ, Holmes DR Jr, et al. Link between the angiographic substudy and mortality outcomes in a large ran- domized trial of myocardial reperfusion: importance of early and complete infarct artery reperfusion. Circulation 1995;91:
1923-8.
26) Ito H, Okamura A, Iwakura K, et al. Myocardial perfusion pa- tterns related to thrombolysis in myocardial infarction grades after coronary angiography in patients with anterior wall myo- cardial infarction. Circulation 1996;93:1993-9.
27) Mazur W, Bitar JN, Lechin M, et al. Coronary flow reserve may predict myocardial recovery after myocardial infarction in pa- tients with TIMI grade 3 flow. Am Heart J 1998;136:335-44.
28) Teiger E, Garot J, Aptecar E, et al. Coronary blood flow reserve and wall motion recovery in patients undergoing angioplasty after myocardial infarction. Eur Heart J 1999;20:285-92.
29) Lepper W, Hoffmann R, Kamp O, et al. Assessment of myocar- dial reperfusion by intravenous myocardial contrast echocar- diography and coronary flow reserve after primary transluminal coronary angiography in patients with acute myocardial infarc- tion. Circulation 2000;101:2368-74.
30) Hori M, Inoue M, Kitakaze M, et al. Role of adenosine in hy- peremic response of coronary blood flow in microembolization.
Am J Physiol 1986;250:H509-18.